Abstract
Background
Probiotics have tremendous potential to develop healthy diets, treatment, and prevention. Investigation of in vitro cultural properties of health-promoting microorganisms like lactic acid bacteria (LAB) and bifidobacteria is crucial to select probiotic strains for treatments based on gut microbiota modulation to justify individualized and personalized approach for nutrition and prevention of variety of diseases. The aim was to study the biological properties of LAB and bifidobacteria probiotic strains, namely adhesive properties; resistance to antibiotics; and biological fluids (gastric juice, bile, pancreatic enzymes), and to overview the literature in the field.
Materials and methods
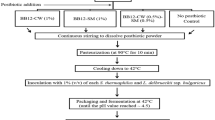
We studied six LAB strains (Lactobacillus acidophilus ІМV В-7279, L. casei ІМV В-7280, L. delbrueckii subsp. bulgaricus ІМV В-7281, L. rhamnosus LB-3 VK6, L. delbrueckii LE VK8, L. plantarum LM VK7), and two bifidobacteria strains (Bifidobacterium animalis VKL, B. animalis VKB). We characterized tinctorial, culturally morphological, physiological, and biochemical properties of probiotic strains of LAB and bifidobacteria by commonly used research methods. Determination of the resistance to antibiotics was carried out using disc-diffusion method. The effects of gastric juice, bile, and pancreatin on the viability of LAB and bifidobacteria were evaluated. Adhesive properties of LAB and bifidobacteria to epithelial cells were assessed calculating three indicators: average adhesion rate (AAR), participation rate of epithelial cells (PRE), and adhesiveness index of microorganisms (AIM). Electron microscopy of LAB and bifidobacteria cells was conducted.
Results
The studied strains of LAB and bifidobacteria did not form spores, were positively stained by Gram, grow on medium in a wide range of pH (1.0–9.0, optimum pH 5.5–6.5), were sensitive to a wide range of antibiotics; and showed different resistance to gastric juice, bile, and pancreatic enzymes. The most resistant to antibiotics were L. rhamnosus LB-3 VK6 and L. delbrueckii LE VK8 strains. The most susceptible to gastric juice was L. plantarum LM VK7, which stopped its growth at 8% of gastric juice; L. acidophilus IMV B-7279, B. animalis VKL, and B. animalis VKB strains were resistant even in the 100% concentration. Strains L. acidophilus IMV В-7279, L. casei IMV В-7280, B. animalis VKL, B. animalis VKB, L. rhamnosus LB-3 VK6, L. delbrueckii LE VK8, and L. delbrueckii subsp. bulgaricus IMV В-7281 were resistant to pancreatic enzymes. Adhesive properties of the strains according to AIM index were high in L. casei IMV В-7280, B. animalis VKL, and B. animalis VKB; were moderate in L. delbrueckii subsp. bulgaricus IMV В-7281; and were low in L. acidophilus IMV В-7279, L. rhamnosus LB-3 VK6, L. delbrueckii LE VK8, and L. plantarum LM VK7.
Conclusion
We recognized strain-dependent properties of studied LAB and bifidobacteria probiotic strains (adhesive ability, resistance to antibiotics, and gut biological fluids) and discussed potential for most effective individualized treatment for gut and distant sites microbiome modulation.





Similar content being viewed by others
References
Parekh PJ, Balart LA, Johnson DA. The influence of the gut microbiome on obesity, metabolic syndrome and gastrointestinal disease. Clin Transl Gastroenterol. 2015 Jun 18;6:e91. https://doi.org/10.1038/ctg.2015.16.
WHO/FAO scientific document. http://who.int/foodsafety/fs_management/en/probiotic_guidelines.pdf. Accessed 11 Feb 2018.
Hill C, Guarner F, Reid G, Gibson GR, Merenstein DJ, Pot B, et al. Expert consensus document. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol. 2014;8:506–14. https://doi.org/10.1038/nrgastro.2014.66.
Gibson GR, Hutkins R, Sanders ME, Prescott SL, Reimer RA, Salminen SJ, et al. Expert consensus document: the International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of prebiotics. Nat Rev Gastroenterol Hepatol. 2017;14(8):491–502. https://doi.org/10.1038/nrgastro.2017.75.
Bubnov RV, Spivak MY, Lazarenko LM, Bomba A, Boyko NV. Probiotics and immunity: provisional role for personalized diets and disease prevention. EPMA J. 2015;6:14.
Aron-Wisnewsky J, Clément K. The gut microbiome, diet, and links to cardiometabolic and chronic disorders. Nat Rev Nephrol. 2016 Mar;12(3):169-81. doi: 10.1038/nrneph.2015.191.
Lazarenko LM, Babenko LP, Bubnov RV, Demchenko OM, Zotsenko VM, Boyko NV, et al. Imunobiotics are the novel biotech drugs with antibacterial and immunomodulatory properties. Mikrobiol Z. 2017;79(1):66–75.
Bubnov RV, Babenko LP, Lazarenko LM, Mokrozub VV, Demchenko OA, Nechypurenko OV, et al. Comparative study of probiotic effects of lactobacillus and bifidobacteria strains on cholesterol levels, liver morphology and the gut microbiota in obese mice. EPMA J. 2017;8(4):357–76. https://doi.org/10.1007/s13167-017-0117-3.
Jobin C. Precision medicine using microbiota. Science. 2018 Jan 5;359(6371):32–4. https://doi.org/10.1126/science.aar2946.
Lebeer S, Bron PA, Marco ML, VanPijkeren JP, O'Connell Motherway M, Hill C, et al. Identification of probiotic effector molecules: present state and future perspectives. Curr Opin Biotechnol. 2017;49:217–23. https://doi.org/10.1016/j.copbio.2017.10.007.
Marchesi JR, Adams DH, Fava F, Hermes GD, Hirschfield GM, Hold G, et al. The gut microbiota and host health: a new clinical frontier. Gut. 2016;65(2):330–9. https://doi.org/10.1136/gutjnl-2015-309990.
Reid G, Abrahamsson T, Bailey M, Bindels LB, Bubnov R, Ganguli K, et al. How do probiotics and prebiotics function at distant sites? Benef Microbes. 2017 Aug 24;8(4):521–33. https://doi.org/10.3920/BM2016.0222.
Golubnitschaja O, Baban B, Boniolo G, Wang W, Bubnov R, Kapalla M, et al. Medicine in the early twenty-first century: paradigm and anticipation—EPMA position paper 2016. EPMA J. 2016;7:23.
Shapiro H, Suez J, Elinav E. Personalized microbiome-based approaches to metabolic syndrome management and prevention. J Diabetes. 2017;9(3):226–36. https://doi.org/10.1111/1753-0407.12501. Review.
Dao MC, Clément K. Gut microbiota and obesity: Concepts relevant to clinical care. Eur J Intern Med. 2018;48:18-24. https://doi.org/10.1016/j.ejim.2017.10.005.
van den Nieuwboer M, Browne PD, Claassen E. Patient needs and research priorities in probiotics: a quantitative KOL prioritization analysis with emphasis on infants and children. Pharma Nutrition. 2016;4(1):19–28.
Park S, Bae JH. Probiotics for weight loss: a systematic review and meta-analysis. Nutr Res. 2015;35:566–75.
Rondanelli M, Faliva MA, Perna S, Giacosa A, Peroni G, Castellazzi AM. Using probiotics in clinical practice: where are we now? A review ofexisting meta-analyses. Gut Microbes. 2017;8(6):521–43. https://doi.org/10.1080/19490976.2017.1345414.
Papadimitriou K, Zoumpopoulou G, Foligné B, et al. Discovering probiotic microorganisms: in vitro, in vivo, genetic and omics approaches. Front Microbiol. 2015;6:58. https://doi.org/10.3389/fmicb.2015.00058.
Fijan S. Microorganisms with claimed probiotic properties: an overview of recent literature. Int J Environ Res Public Health. 2014;11(5):4745–67.
Shah P, Fritz JV, Glaab E, Desai MS, Greenhalgh K, Frachet A, et al. A microfluidics-based in vitro model of the gastrointestinal human-microbe interface. Nat Commun. 2016;7:11535. https://doi.org/10.1038/ncomms11535.
Nguyen TL, Vieira-Silva S, Liston A, Raes J. How informative is the mouse for human gut microbiota research? Dis Model Mech. 2015;8(1):1–16. https://doi.org/10.1242/dmm.017400.
Neville BA, Forster SC, Lawley TD. Commensal Koch’s postulates: establishing causation in human microbiota research. CurrOpinMicrobiol. 2017;42:47–52. https://doi.org/10.1016/j.mib.2017.10.001.
Qin J, Li R, Raes J, Arumugam M, Burgdorf KS, Manichanh C, et al. A human gut microbial gene catalogue established by metagenomic sequencing. Nature. 2010;464:59–65.
D'Aimmo MR, Mattarelli P, Biavati B, Carlsson NG, Andlid T. The potential of bifidobacteria as a source of natural folate. J Appl Microbiol. 2012;112(5):975–84. https://doi.org/10.1111/j.1365-2672.2012.05261.x.
Lilly DM, Stillwell RH. Growth promoting factors produced by probiotics. Science. 1965;147:747–8.
Gao C, Ganesh BP, Shi Z, Shah RR, Fultz R, Major A, et al. Gut microbe-mediated suppression of inflammation-associated colon carcinogenesis by luminal histamine production. Am J Pathol. 2017 Oct;187(10):2323–36. https://doi.org/10.1016/j.ajpath.2017.06.011.
Bermudez-Brito M, Plaza-Díaz J, Muñoz-Quezada S, Gómez-Llorente C, Gil A. Probiotic mechanisms of action. Ann Nutr Metab. 2012;61(2):160–74. https://doi.org/10.1159/000342079.
Rodrigues RR, Greer RL, Dong X, DSouza KN, Gurung M, Wu JY, et al. Antibiotic-induced alterations in gut microbiota are associated with changes in glucose metabolism in healthy mice. Front Microbiol. 2017;8:2306. https://doi.org/10.3389/fmicb.2017.02306.
Penders J, Stobberingh EE, Savelkoul PHM, Wolffs PFG. The human microbiome as a reservoir of antimicrobial resistance. Front Microbiol. 2013;4:87. https://doi.org/10.3389/fmicb.2013.00087.
D'Aimmo MR, Modesto M, Biavati B. Antibiotic resistance of lactic acid bacteria and Bifidobacterium spp. isolated from dairy and pharmaceutical products. Int J Food Microbiol. 2007;115(1):35–42.
Avdeeva LV, Osadchaia AI, Kharkhota MA. Influence of lactitol and lactulose on adhesion properties of Bacillus subtilis probiotic strains. Mikrobiol Z. 2012;74(5):22–5.
Lagier JC, Armougom F, Million M, Hugon P, Pagnier I, Robert C, et al. Microbial culturomics: paradigm shift in the human gut microbiome study. Clin Microbiol Infect. 2012;18:1185–93.
Lagier JC, Hugon P, Khelaifia S, Fournier PE, la Scola B, Raoult D. The rebirth of culture in microbiology through the example of culturomics to study human gut microbiota. Clin Microbiol Rev. 2015;28:237–64.
Lagier JC, Khelaifia S, Alou MT, Ndongo S, Dione N, Hugon P, Caputo A, Cadoret F, Traore SI, Seck EH et al.: Culture of previously uncultured members of the human gut microbiota by culturomics. 2016;1:16203. doi: https://doi.org/10.1038/nmicrobiol.2016.203.
Browne HP, Forster SC, Anonye BO, Kumar N, Neville BA, Stares MD, et al. Culturing of “unculturable” human microbiota reveals novel taxa and extensive sporulation. Nature. 2016 May 26;533(7604):543–6. https://doi.org/10.1038/nature17645.
Ruiz L, Delgado S, Ruas-Madiedo P, Sánchez B, Margolles A. Bifidobacteria and their molecular communication with the immune system. Front Microbiol. 2017;8:2345. https://doi.org/10.3389/fmicb.2017.02345.
Kobayashi H, Kanmani P, Ishizuka T, Miyazaki A, Soma J, Albarracin L, et al. Development of an in vitro immunobiotic evaluation system against rotavirus infection in bovine intestinal epitheliocytes. Benef Microbes. 2017;8:309–21. https://doi.org/10.3920/BM2016.0155.
Mokrozub VV, Lazarenko LM, Sichel LM, Bubnov RV, Spivak MY. The role of beneficial bacteria wall elasticity in regulating innate immune response. EPMA J. 2015;6:13.
Hidalgo-Cantabrana C, Sánchez B, Milani C, Ventura M, Margolles A, Ruas-Madiedo P. Genomic overview and biological functions of exopolysaccharide biosynthesis in Bifidobacterium spp. ApplEnvironMicrobiol. 2014;80(1):9–18. https://doi.org/10.1128/AEM.02977-13.
Hidalgo-Cantabrana C, Sánchez B, Álvarez-Martín P, López P, Martínez-Álvarez N, Delley M, et al. A single mutation in the gene responsible for the mucoid phenotype of Bifidobacterium animalis subsp. lactis confers surface and functional characteristics. ApplEnvironMicrobiol. 2015;81(23):7960–8. https://doi.org/10.1128/AEM.02095-15.
Kailasapathy K, Chin J. Survival and therapeutic potential of probiotic organisms with reference to lactobacillus acidophilus and Bifidobacterium spp. Immunol Cell Biol. 2000;78(1):80–8.
Liu Z, Jiang Z, Zhou K, Li P, Liu G, Zhang B. Screening of bifidobacteria with acquired tolerance to human gastrointestinal tract. Anaerobe. 2007;13(5–6):215–9.
Chou LS, Weimer B. Isolation and characterization of acid- and bile-tolerant isolates from strains of lactobacillus acidophilus. J Dairy Sci. 1999;82(1):23–31.
Bernet MF, Brassart D, Neeser JR, Servin AL. Adhesion of human bifidobacterial strains to cultured human intestinal epithelial cells and inhibition of enteropathogen-cell interactions. Appl Environ Microbiol. 1993;59(12):4121–8.
Golding CG, Lamboo LL, Beniac DR, Booth TF. The scanning electron microscope in microbiology and diagnosis of infectious disease. Sci Rep. 2016 May 23;6:26516. https://doi.org/10.1038/srep26516.
Teuber M, Meile L, Schwarz F. Acquired antibiotic resistance in lactic acid bacteria from food. Antonie Van Leeuwenhoek. 1999;76(1–4):115–37. Review
Singer RS, Finch R, Wegener HC, Bywater R, Walters J, Lipsitch M. Antibiotic resistance—the interplay between antibiotic use in animals and human beings. Lancet Infect Dis. 2003 Jan;3(1):47–51.
Gueimonde M, Sánchez B, de los Reyes-Gavilán CG, Margolles A. Antibiotic resistance in probiotic bacteria. Front Microbiol. 2013;4:202. https://doi.org/10.3389/fmicb.2013.00202.
Zheng M, Zhang R, Tian X, Zhou X, Pan X, Wong A. Assessing the risk of probiotic dietary supplements in the context of antibiotic resistance. Front Microbiol. 2017;8:908.
Sharma P, Tomar SK, Goswami P, Sangwan V, Singh R. Antibiotic resistance among commercially available probiotics. Food Res Int. 2014;57:176–95.
Tannock GW, Luchansky JB, Miller L, Connell H, Thode-Andersen S, Mercer AA, et al. Molecular characterization of a plasmid-borne (pGT633) erythromycin resistance determinant (ermGT) from Lactobacillus reuteri 100-63. Plasmid. 1994;31(1):60–71.
Mater DD, Langella P, Corthier G, Flores MJ. A probiotic lactobacillus strain can acquire vancomycin resistance during digestive transit in mice. J Mol Microbiol Biotechnol. 2008;14(1–3):123–7.
EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies). General scientific guidance for stakeholders on health claim applications. EFSA Journal. 2016;14(1):4367 [38 pp.] https://doi.org/10.2903/j.efsa.2016.4367.
European Food Safety Authority (EFSA). Technical guidance—update of the criteria used in the assessment of bacterial resistance to antibiotics of human or veterinary importance. EFSA J. 2008;732:1–15. https://doi.org/10.2903/j.efsa.2008.732.
González-Rodríguez I, Ruiz L, Gueimonde M, Margolles A, Sánchez B. Factors involved in the colonization and survival of bifidobacteria in the gastrointestinal tract. FEMS Microbiol Lett. 2013 Mar;340(1):1–10.
Hassanzadazar H, Ehsani A, Mardani K, Hesari J. Investigation of antibacterial, acid and bile tolerance properties of lactobacilli isolated from Koozeh cheese. Veterinary research Forum. 2012;3(3):181–5.
Ruiz L, Margolles A, Sánchez B. Bile resistance mechanisms in lactobacillus and bifidobacterium. Front Microbiol. 2013;4:396. https://doi.org/10.3389/fmicb.2013.00396.
Nie YF, Hu J, Yan XH. Cross-talk between bile acids and intestinal microbiota in host metabolism and health. J Zhejiang Univ Sci B. 2015 Jun; 16(6):436-46. doi: 10.1631/jzus.B1400327
Park MY, Kim SJ, Ko EK, Ahn SH, Seo H, Sung MK. Gut microbiota-associated bile acid deconjugation accelerates hepatic steatosis in Ob/Ob mice. J Appl Microbiol. 2016 Sep;121(3):800–10.
Gu Y, Wang X, Li J, Zhang Y, Zhong H, Liu R, et al. Analyses of gut microbiota and plasma bile acids enable stratification of patients for antidiabetic treatment. Nat Commun. 2017;8(1):1785. https://doi.org/10.1038/s41467-017-01682-2.
Tanaka H, Doesburg K, Iwasaki T, Mierau I. Screening of lactic acid bacteria for bile salt hydrolase activity. J Dairy Sci. 1999;82:2530–5.
Wang T, Cai G, Qiu Y, Fei N, Zhang M, Pang X, et al. Structural segregation of gut microbiota between colorectal cancer patients and healthy volunteers. ISME J. 2012;6:320–9.
Del Piano M, Strozzi P, Barba M, Allesina S, Deidda F, Lorenzini P, et al. In vitro sensitivity of probiotics to human pancreatic juice. J Clin Gastroenterol. 2008;42(Suppl 3 Pt 2):S170–3. https://doi.org/10.1097/MCG.0b013e3181815976.
Collado MC, Sanz Y. Induction of acid resistance in bifidobacterium: a mechanism for improving desirable traits of potentially probiotic strains. J Appl Microbiol. 2007 Oct;103(4):1147–57.
Lebeer S, Vanderleyden J, De Keersmaecker SC. Genes and molecules of lactobacilli supporting probiotic action. Mucosal adhesion properties of the probiotic Lactobacillus rhamnosus GG SpaCBA and SpaFED pilin subunits. Microbiol Mol Biol Rev. 2008;72(4):728–64.
Lebeer S, Claes I, Tytgat HL, Verhoeven TL, Marien E, von Ossowski I, et al. Functional analysis of lactobacillus rhamnosus GG pili in relation to adhesion and immunomodulatory interactions with intestinal epithelial cells. Appl Environ Microbiol. 2012;78(1):185–93. https://doi.org/10.1128/AEM.06192-11.
von Ossowski I, Reunanen J, Satokari R, Vesterlund S, Kankainen M, Huhtinen H, et al. Mucosal adhesion properties of the probiotic Lactobacillus rhamnosus GG SpaCBA and SpaFED pilin subunits. Appl Environ Microbiol. 2010;76(7):2049–57. https://doi.org/10.1128/AEM.01958-09.
Tytgat HL, van Teijlingen NH, Sullan RM, Douillard FP, Rasinkangas P, Messing M, et al. Probiotic gut microbiota isolate interacts with dendritic cells via glycosylated heterotrimeric pili. PLoS One. 2016;11(3):e0151824. https://doi.org/10.1371/journal.pone.0151824. eCollection 2016.
Burgain J, Scher J, Lebeer S, Vanderleyden J, Corgneau M, Guerin J, et al. Impacts of pH-mediated EPS structure on probiotic bacterial pili-whey proteins interactions. Colloids Surf B Biointerfaces. 2015;134:332–8. https://doi.org/10.1016/j.colsurfb.2015.06.068. Epub 2015 Jul 15
Burgain J, Gaiani C, Francius G, Revol-Junelles AM, Cailliez-Grimal C, Lebeer S, et al. In vitro interactions between probiotic bacteria and milk proteins probed by atomic force microscopy. Colloids Surf B Biointerfaces. 2013;104:153–62. https://doi.org/10.1016/j.colsurfb.2012.11.032.
Tytgat HL, Schoofs G, Vanderleyden J, Van Damme EJ, Wattiez R, Lebeer S, et al. Systematic exploration of the glycoproteome of the beneficial gut isolate Lactobacillus rhamnosus GG. J Mol Microbiol Biotechnol. 2016;26(5):345–58. https://doi.org/10.1159/000447091.
Guerin J, Burgain J, Borges F, Bhandari B, Desobry S, Scher J, et al. Use of imaging techniques to identify efficient controlled release systems of lactobacillus rhamnosus GG during in vitro digestion. Food Funct. 2017;8(4):1587–98. https://doi.org/10.1039/c6fo01737a.
Tripathi P, Beaussart A, Alsteens D, Dupres V, Claes I, von Ossowski I, et al. Adhesion and nanomechanics of pili from the probiotic Lactobacillus rhamnosus GG. ACS Nano. 2013;7(4):3685–97. https://doi.org/10.1021/nn400705u.
Garcia SL, Buck M, McMahon KD, Grossart HP, Eiler A, Auxotrophy WF. Intrapopulation complementary in the ‘interactome’ of a cultivated freshwater model community. Mol Ecol. 2015;24(17):4449–59. https://doi.org/10.1111/mec.13319.
Garcia SL, Stevens SLR, Crary B, Martinez-Garcia M, Stepanauskas R, Woyke T, et al. Contrasting patterns of genome-level diversity across distinct co-occurring bacterial populations. ISME J. 2018;12(3):745-55. doi: https://doi.org/10.1038/s41396-017-0001-0
Salas-Jara MJ, Ilabaca A, Vega M, García A. Biofilm forming Lactobacillus: new challenges for the development of probiotics. Microorganisms. 2016;4(3). https://doi.org/10.3390/microorganisms4030035.
O'Connell Motherway M, Zomer A, Leahy SC, Reunanen J, Bottacini F, Claesson MJ, et al. Functional genome analysis of Bifidobacterium breve UCC2003 reveals type IVb tight adherence (Tad) pili as an essential and conserved host-colonization factor. Proc Natl Acad Sci U S A. 2011 Jul 5;108(27):11217–22. https://doi.org/10.1073/pnas.1105380108.
Shokryazdan P, Sieo CC, Kalavathy R, Liang JB, Alitheen NB, Faseleh Jahromi M, et al. Probiotic potential of lactobacillus strains with antimicrobial activity against some human pathogenic strains. Biomed Res Int. 2014;2014:927268. https://doi.org/10.1155/2014/927268.
He S, Ran C, Qin C, Li S, Zhang H, de Vos WM, et al. Anti-infective effect of adhesive probiotic lactobacillus in fish is correlated with their spatial distribution in the intestinal tissue. Sci Rep. 2017;7:13195. https://doi.org/10.1038/s41598-017-13466-1.
Collado MC, Jalonen L, Meriluoto J, Salminen S. Protection mechanism of probiotic combination against human pathogens: in vitro adhesion to human intestinal mucus. Asia Pac J Clin Nutr. 2006;15(4):570–5.
Compare D, Rocco A, Zamparelli MS, Nardone G. The gut bacteria-driven obesity development. Dig Dis. 2016;34(3):221–9.
Jiang TT, Shao TY, Ang WXG, Kinder JM, Turner LH, Pham G, et al. Commensal Fungi recapitulate the protective benefits of intestinal bacteria. Cell Host Microbe. 2017;22(6):809–816.e4. https://doi.org/10.1016/j.chom.2017.10.013.
Ilavenil S, Park HS, Vijayakumar M, Arasu MV, Kim DH, Ravikumar S, et al. Probiotic potential of lactobacillus strains with antifungal activity isolated from animal manure. ScientificWorldJournal. 2015;2015:802570. https://doi.org/10.1155/2015/802570.
Yatsunenko T, Rey FE, Manary MJ, Trehan I, Dominguez-Bello MG, Contreras M, et al. Human gut microbiome viewed across age and geography. Nature. 2012;486:222–7. https://doi.org/10.1038/nature11053
De Filippo C, Cavalieri D, Di Paola M, Ramazzotti M, Poullet JB, Massart S, et al. Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc Natl Acad Sci U S A. 2010;107:14691–6. https://doi.org/10.1073/pnas.1005963107.
Kong LC, Holmes BA, Cotillard A, Habi-Rachedi F, Brazeilles R, Gougis S, et al. Dietary patterns differently associate with inflammation and gut microbiota in overweight and obese subjects. PLoS One. 2014;9:e109434. https://doi.org/10.1371/journal.pone.0109434.
Cotillard A, Kennedy SP, Kong LC, Prifti E, Pons N, Le Chatelier E, et al. Dietary intervention impact on gut microbial gene richness. Nature. 2013;500:585–8. https://doi.org/10.1038/nature12480
Beaumont M, Goodrich JK, Jackson MA, Yet I, Davenport ER, Vieira-Silva S, et al. Heritable components of the human fecal microbiome are associated with visceral fat. Genome Biol. 2016;17:189. https://doi.org/10.1186/s13059-016-1052-7.
Org E, Blum Y, Kasela S, Mehrabian M, Kuusisto J, Kangas AJ, et al. Relationships between gut microbiota, plasma metabolites, and metabolic syndrome traits in the METSIM cohort. Genome Biol. 2017;18:70. https://doi.org/10.1186/s13059-017-1194-2.
Liu J, Chen FH, Qiu SQ, Yang LT, Zhang HP, Liu JQ, et al. Probiotics enhance the effect of allergy immunotherapy on regulating antigen specific B cell activity in asthma patients. Am J Transl Res. 2016 Dec 15;8(12):5256–70.
Vieira AT, Galvão I, Amaral FA, Teixeira MM, Nicoli JR, Martins FS. Oral treatment with Bifidobacterium longum 51A reduced inflammation in a murine experimental model of gout. Benef Microbes. 2015;6(6):799–806. https://doi.org/10.3920/BM2015.0015.
Konopelniuk VV, Goloborodko II, Ishchuk TV, Synelnyk TB, Ostapchenko LI, Spivak MY, et al. Efficacy of fenugreek-based bionanocomposite on renal dysfunction and endogenous intoxication in high-calorie diet-induced obesity rat model-comparative study. EPMA J. 2017;8(4):377–90. https://doi.org/10.1007/s13167-017-0098-2.
Babenko LP, Lazarenko LM, Shynkarenko LM, Mokrozub VV, Pidgorskyi VS, Spivak MY. The effect of lacto- and bifidobacteria compositions on the vaginal microflora in cases of intravaginal staphylococcosis. Mikrobiol Z. 2012 Nov-Dec;74(6):80–9.
Al Kassaa I, Hober D, Hamze M, Chihib NE, Drider D. Antiviral potential of lactic acid bacteria and their bacteriocins. Probiotics Antimicrob Proteins. 2014;6(3–4):177–85. https://doi.org/10.1007/s12602-014-9162-6.
Dillon SM, Frank DN, Wilson CC. The gut microbiome and HIV-1 pathogenesis: a two-way street. AIDS. 2016;30(18):2737–51.
Hager CL, Ghannoum MA. The mycobiome: role in health and disease, and as a potential probiotic target in gastrointestinal disease. Dig Liver Dis. 2017;49(11):1171–6. https://doi.org/10.1016/j.dld.2017.08.025.
Talwalkar A, Kailasapathy K. Metabolic and biochemical responses of probiotic bacteria to oxygen. J Dairy Sci. 2003;86(8):2537–46.
Talwalkar A, Kailasapathy K. The role of oxygen in the viability of probiotic bacteria with reference to L. acidophilus and Bifidobacterium spp. Curr Issues Intest Microbiol. 2004 Mar;5(1):1–8.
Wang Y, Kirpich I, Liu Y, Ma Z, Barve S, McClain CJ, et al. Lactobacillus rhamnosus GG treatment potentiates intestinal hypoxia-inducible factor, promotes intestinal integrity and ameliorates alcohol-induced liver injury. Am J Pathol. 2011;179(6):2866–75. https://doi.org/10.1016/j.ajpath.2011.08.039.
Bubnov R, Jr PJ, Zubor P, Koniczka K, Golubnitschaja O. Pre-metastatic niches in breast cancer: are they created by or prior to the tumour onset? “Flammer syndrome” relevance to address the question. EPMA J. 2017;8:141–57. https://doi.org/10.1007/s13167-017-0092-8.
Bubnov RV. Ultrasonography diagnostic capability for mesenteric vascular disorders. Gut. 2011;60(Suppl 3):A104.
Taur Y, Jenq RR, Perales MA, Littmann ER, Morjaria S, Ling L, et al. The effects of intestinal tract bacterial diversity on mortality following allogeneic hematopoietic stem cell transplantation. Blood. 2014;124(7):1174–82.
Grech G, Zhan X, Yoo BC, Bubnov R, Hagan S, Danesi R, et al. Position paper in cancer: current overview and future perspectives. EPMA J. 2015;6(1):9. https://doi.org/10.1186/s13167-015-0030-6.
York A. Microbiome: gut microbiota sways response to cancer immunotherapy. Nat Rev Microbiol. 2018;16(3):121. https://doi.org/10.1038/nrmicro.2018.12.
Kobyliak NM, Falalyeyeva TM, Kuryk OG, Beregova TV, Bodnar PM, Zholobak NM, et al. Antioxidative effects of cerium dioxide nanoparticles ameliorate age-related male infertility: optimistic results in rats and the review of clinical clues for integrative concept of men health and fertility. EPMA J. 2015 Jun 10;6(1):12. https://doi.org/10.1186/s13167-015-0034-2.
Babenko L, Bubnov R, Lazarenko L, Mokrozub V, Ganova L Kiseleva E, Shevchuk V, Spivak M. Use of probiotic bacteria increase effectiveness of vactination against hepatitis B in experimental studies Reviews in antiviral therapy infectious diseases (abstract book of the 3rd CEE meeting on viral hepatitis and co-infection with HIV, 27-28 September 2017, Ljubliana, Slovenia) 2017, 9:35.
Vitetta L, Saltzman ET, Thomsen M, Nikov T, Hall S. Adjuvant probiotics and the intestinal microbiome: enhancing vaccines and immunotherapy outcomes. Vaccines (Basel). 2017;5 (4). doi: https://doi.org/10.3390/vaccines5040050.
Kassaian N, Aminorroaya A, Feizi A, Jafari P, Amini M. The effects of probiotic and synbiotic supplementation on metabolic syndrome indices in adults at risk of type 2 diabetes: study protocol for a randomized controlled trial. Trials. 2017;18(1):148. https://doi.org/10.1186/s13063-017-1885-8.
Acknowledgements
The study was conducted with the support of the State Agency on Science, Innovations, and Informatization of Ukraine.
Authors’ contributions
RVB suggested the idea and design of the study, participated in experiments, did the study analysis, prepared discussion, formulated future outlooks, and performed article drafting. LML and LPB prepared the first draft of manuscript, did the literature analysis, interpreted the results, and performed the statistical analysis. LPB and LML, performed the experiments on animals and participated analysis of the study. VVM performed the experiments. MYS did the organization, revision manuscript, and data interpretation, and contributed to the overall development of the studied topic. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Bubnov, R.V., Babenko, L.P., Lazarenko, L.M. et al. Specific properties of probiotic strains: relevance and benefits for the host. EPMA Journal 9, 205–223 (2018). https://doi.org/10.1007/s13167-018-0132-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13167-018-0132-z