Abstract
Introduction
Ayurvedic and herbal medicines (AHM) are known to cause varying degrees of drug-induced liver injury (DILI). Clinical, biochemical, histological spectrum and outcomes of AHM linked to severe DILI are not well studied.
Methods
Out of 1440 liver disease patients, 94 were found to have a severe liver injury and associated AHM intake. Thirty-three patients were suspected to have AHM-DILI on Roussel Uclaf Causality Assessment Scoring Method. Forty-seven and 30 of retrieved AHM samples were analyzed for heavy metals and hepatotoxic volatile organic compounds (hVOCs), respectively. Eleven patients ingested AHM from unregistered traditional healers (UTH). Clinicopathological outcomes were analyzed in 27 patients (who underwent liver biopsy) and outcomes with respect to chemical analyses were studied in 33 patients.
Results
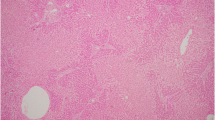
Males predominated (70.4%) with mean age 46.9±15.8 years. Mean follow up was 119.2±81.4 days. The median duration of drug intake was 28 days (10 – 84). Five patients died (18.5%). Hepatic encephalopathy, hypoalbuminemia, and hepatic necrosis were significantly associated with mortality (p < 0.005). Arsenic and mercury ingestion was significantly associated with death (p < 0.005). hVOCs were detected in more than 70% of samples. AHM intake from UTH was associated with higher mortality.
Conclusion
Adequate regulation and scrutiny regarding AHM use among the general population is an unmet need. Early liver biopsy after clinical identification of at-risk patients can expedite definitive treatment with a liver transplant.



Similar content being viewed by others
References
Kleiner DE. The pathology of drug-induced liver injury. Semin Liver Dis. 2009;29:364–72.
Bent S, Ko R. Commonly used herbal medicines in the United States: a review. Am J Med. 2004;116:478–85.
Seeff LB. Herbal hepatotoxicity. Clin Liver Dis. 2007;11:577–96.
Chalasani N, Fontana RJ, Bonkovsky HL, et al. Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology. 2008;135:1924–34, 1934 e1-4.
Devarbhavi H, Dierkhising R, Kremers WK, Sandeep MS, Karanth D, Adarsh CK. Single-center experience with drug-induced liver injury from India: causes, outcome, prognosis, and predictors of mortality. Am J Gastroenterol. 2010;105:2396–404.
Bunchorntavakul C, Reddy KR. Review article: herbal and dietary supplement hepatotoxicity. Aliment Pharmacol Ther. 2013;37:3–17.
Aithal GP, Watkins PB, Andrade RJ, et al. Case definition and phenotype standardization in drug-induced liver injury. Clin Pharmacol Ther. 2011;89:806–15.
Danan G, Benichou C. Causality assessment of adverse reactions to drugs—I. A novel method based on the conclusions of international consensus meetings: application to drug-induced liver injuries. J Clin Epidemiol. 1993;46:1323–30.
Agarwal VK, McHutchison JG, Hoofnagle JH, Drug-Induced Liver Injury Network. Important elements for the diagnosis of the drug-induced liver injury. Clin Gastroenterol Hepatol. 2010;8:463–70.
de Boer YS, Sherker AH. Herbal and dietary supplement-induced liver injury. Clin Liver Dis. 2017;21:135–49.
Ou P, Chen Y, Li B, et al. Causes, clinical features and outcomes of drug-induced liver injury in hospitalized patients in a Chinese tertiary care hospital. Spring. 2015;4:802.
Björnsson E, Talwalkar J, Treeprasertsuk S, et al. Drug-induced autoimmune hepatitis: clinical characteristics and prognosis. Hepatology. 2010;51:2040–8.
Czaja AJ. Drug-induced autoimmune-like hepatitis. Dig Dis Sci. 2011;56:958–76.
Sebode M, Schulz L, Lohse AW. “Autoimmune(-Like)” drug and herb induced liver injury: new insights into molecular pathogenesis. Int J Mol Sci. 2017;18:E1954.
Kleiner DE, Chalasani NP, Lee WM, et al. Hepatic histological findings in suspected drug-induced liver injury: systematic evaluation and clinical associations. Hepatology. 2014;59:661–70.
Chalasani N, Bonkovsky HL, Fontana R, et al. Features and outcomes of 899 patients with drug-induced liver injury: the DILIN prospective study. Gastroenterology. 2015;148:1340–52.
Kleiner DE, Chalasani NP, Conjeevaram HS, Bonkovsky HL, Russo MW, Davern TJ. Relationship of biochemical to histologic findings and the pathological pattern of injury among cases identified in the NIH Drug-Induced Liver Injury Network (DILIN) study. Gastroenterology. 2007;132:A773.
Björnsson E, Kalaitzakis E, Olsson R. The impact of eosinophilia and hepatic necrosis on prognosis in patients with drug-induced liver injury. Aliment Pharmacol Ther. 2007;25:1411–21.
Saper RB, Phillips RS, Sehgal A, et al. Lead, mercury, and arsenic in US- and Indian-manufactured ayurvedic medicines sold via the internet. JAMA. 2008;300:915–23.
Navarro VJ, Barnhart H, Bonkovsky HL, et al. Liver injury from herbals and dietary supplements in the US drug induced liver injury network. Hepatology. 2014;60:1399–408.
Sharma B, Singh S, Siddiqi NJ. Biomedical implications of heavy metals induced imbalances in redox systems. Biomed Res Int. 2014;2014:640754.
Wahlang B, Beier JI, Clair HB, et al. Toxicant-associated steatohepatitis. Toxicol Pathol. 2013;41:343–60.
Tolman KG, Sirrine RW. Occupational hepatotoxicity. Clin Liver Dis. 1998;2:563–89.
Cotrim HP, Andrade ZA, Parana R, Portugal M, Lyra LG, Freitas LA. Nonalcoholic steatohepatitis: a toxic liver disease in industrial workers. Liver. 1999;19:299–304.
Perez CA, Bosia JD, Cantore MS, et al. Liver damage in workers exposed to hydrocarbons. Gastroenterol Hepatol. 2006;29:334–7.
Neuberger M, Rappe C, Bergek S, et al. Persistent health effects of dioxin contamination in herbicide production. Environ Res. 1999;81:206–14.
Malaguarnera G, Cataudella E, Giordano M, Nunnari G, Chisari G, Malaguarnera M. Toxic hepatitis in occupational exposure to solvents. World J Gastroenterol. 2012;18:2756–66.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
CAP, RP, AKJ, KLA, and PA declare that they have no conflict of interests.
Ethics statement
The authors declare that the study was performed in a manner to conform to the Helsinki Declaration of 1975, as revised in 2000 and 2008, concerning human and animal rights. The protocol was approved by the Institutional Ethics Committee and informed consent was obtained from the study subjects. The authors are responsible for the findings and the content of the paper.
Additional information
Parts of this study results were presented as Parallel Oral and Presidential Plenary at the American Association for the Study of Liver Diseases annual conference, The Liver Meeting, held at Washington D.C. on 22nd and 24th October 2017, respectively.
Rights and permissions
About this article
Cite this article
Philips, C.A., Paramaguru, R., Joy, A.K. et al. Clinical outcomes, histopathological patterns, and chemical analysis of Ayurveda and herbal medicine associated with severe liver injury—A single-center experience from southern India. Indian J Gastroenterol 37, 9–17 (2018). https://doi.org/10.1007/s12664-017-0815-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-017-0815-8