Abstract
Objective
If individuals want to integrate health-enhancing physical activity in their everyday life, they need specific competences. This person-oriented study aimed to: 1) Identify patterns of physical activity-related health competence, 2) examine how structurally and individually stable these patterns are over 4 months and 3) test how changes in patterns are associated with changes in subjective health indicators.
Materials and methods
A total of 769 individuals (82% women, Mage = 27 years) were recruited from exercise courses offered by university sport. Four facets of physical activity-related health competence (control competence for physical training, physical activity-specific affect regulation, self-determined motivation for exercise, physical activity-specific self-control) and subjective health (subjective vitality and perceived fitness) were measured twice. Patterns were identified using latent profile analysis. Their stability and associations with subjective health changes were examined with latent transition analyses and a configural frequency analysis.
Results
Seven patterns of physical activity-related health competence were identified. Besides three level patterns, four shape patterns were found with differing ratings across the studied variables (e.g. average values for control competence for physical training, self-determined motivation and physical activity-specific self-control, but a high level in physical activity affect regulation). These patterns proved to be structurally stable over time. In all, 72% of the individuals stayed in the same pattern, whereas 20% moved to a more and 8% to a less competent pattern. Changes in patterns are linked to change in subjective vitality and perceived fitness.
Conclusion
The results presented here demonstrate the added value of using a person-oriented approach to investigate development of physical activity-related health competence. Furthermore, they generate knowledge for designing tailored interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
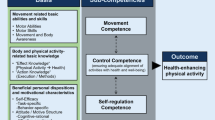
Physical activity (PA) has various positive impacts on health and well-being. It reduces the risk for several diseases and promotes health resources (Beauchamp, Puterman, & Lubans, 2018; Lubans et al., 2016; Warburton & Bredin, 2017). However, if individuals want to initiate and maintain PA in a way that is effective for their health and well-being, they face diverse challenges. To overcome these challenges individuals need to have a complex set of abilities, skills, knowledge, motivation and willingness. In Germany, diverse models have been developed to systematise these required competences (Pfeifer, Sudeck, Geidl, & Tallner, 2013; Töpfer & Sygusch, 2014). The domain-specific models were inspired by concepts of health literacy (Sørensen et al., 2012) and physical literacy (Edwards, Bryant, Keegan, Morgan, & Jones, 2017; Giblin, Collins, & Button, 2014), which are internationally recognised in research and practice (Sørensen et al., 2012; World Health Organization, 2018). One of the aforementioned approaches is the PA-related health competence model (PAHCO; Pfeifer et al., 2013; Sudeck & Pfeifer, 2016). Based on a functional pragmatic understanding of competence (Klieme, Hartig, & Rauch, 2008), the researchers differentiated three areas in this model: (1) Movement competence, (2) control competence for PA and (3) PA-specific self-regulation competence.
(1) Movement competence enables individuals to meet the movement-related requirements of physical activities (e.g. motor abilities, motor skills for cycling or gymnastics). (2) Control competence for PA allows people to gear their own activity to achieve positive effects in health and well-being. Two facets were empirically differentiated here: (a) Control competence for physical training reflects a person’s ability to apply training-specific knowledge in a targeted manner and thus effectively select and structure activities (e.g. the use of body signals to gauge physical strain in strength training in a situation-specific manner). In contrast, (b) PA-specific affect regulation reflects a person’s ability to steer their activity in order to optimise psychological health benefits (e.g. to choose jogging in the forest to reduce stress). Finally, (3) PA-specific self-regulation competence enables individuals to be regularly active. It involves both motivational and volitional factors. On the motivational side, having (a) a self-determined intention to integrate PA into everyday life is crucial. Self-determination refers to the degree of internalisation of a behaviour. It is seen as a continuum, ranging from a person’s intrinsic motivation mode, where the PA is inherently interesting, to an external motivation mode, where the person wants to be active due to external pressure or positive consequences (Deci & Ryan, 2000). On the volitional side, having (b) self-control to translate intentions into actual PA behaviour is important. Self-control includes cognitive strategies, such as developing action and coping plans (Gollwitzer & Oettingen, 2016).
Two assumptions of the PAHCO model were relevant for the present article: Firstly, Sudeck and Pfeifer (2016) hypothesised that PAHCO influences the quantity of PA. In fact, they were able to show that the individual competence facets were linked to the habitual amount of exercise in leisure time. In line with social cognitive models of health behaviour (e.g. Biddle & Fuchs, 2009), the strongest effect was found for PA-specific self-regulation. Secondly, Sudeck and Pfeifer (2016) assumed that it is both the quantity and quality of PA that is important for optimal effects on health and well-being. Put differently, it not only matters how many times or for how long a person engages in strength training, for instance, but also which specific exercise the person chooses and if it is appropriate to their psychophysiological precondition (e.g. vitality). Consequently, especially control competence for PA should be linked with health benefits and well-being (Sudeck & Pfeifer, 2016). So far, two empirical studies support these associations: On the one hand, Sudeck and Pfeifer (2016) showed that control competence for physical training is (in)directly related to physical fitness. On the other hand, Sudeck, Jeckel and Schubert (2018) demonstrated that PA-specific affect regulation moderated the association between PA and affective well-being; individuals with higher PA-specific affect regulation showed more positive affective well-being after PA in everyday life. Taken together, initial findings underline the relevance of PAHCO. Moreover, they support interventions that focus on competences required for a healthy, physically active lifestyle (Geidl et al., 2017; Haible et al., 2019). However, further empirical research is indicated. Firstly, it is important to know which patterns of PAHCO exist (Cairney, Dudle, Kwan, Bulten, & Kriellaars, 2019). Only by focusing on such configurations can one learn how competence facets interact within individuals. Secondly, it is important to understand how stable PAHCO profiles are over time. Addressing these questions is relevant for research and practice, since it might result in more effective promotion of PA. When one is informed about both the pattern and development of PAHCO areas, one can address them with more individually tailored programs.
PAHCO patterns and their stability
When investigating patterns of PAHCO areas within individuals, the person-oriented approach could be relevant (Bergman & Lundh, 2015; Bergman & Magnusson, 1997). This approach assumes that various factors of an individual’s behaviour do not develop independently of one another, but rather in a complex reciprocal interplay. Consequently, statistical procedures which allow inferences about single individuals should be used for the investigation. Variable-oriented methods do not usually fulfil this requirement, as variables are analysed on an aggregated group level. To give an example: the relatively high correlation coefficient found between control competence for physical training and PA-specific affect regulation in a sample (0.48 ≤ r ≤ 0.59; Sudeck & Pfeifer, 2016) does not mean that the correlation is the same for every single person (Bergman & Lundh, 2015). Rather, it is conceivable that an individual may have high control competence for physical training and low PA-specific affect regulation or vice versa.
When examining the stability of PAHCO patterns using a person-oriented approach, two different types of stability need to be distinguished: (a) Structural stability refers to the similarity of PAHCO patterns found at different measurement points on a group level. The structural stability is high if patterns were replicated in similar forms (i.e. indicator means of the PAHCO patterns are more or less the same). In contrast, (b) individual stability refers to development paths between PAHCO patterns on an individual level. Individual stability is given if the majority of individuals of a certain pattern at the first measurement point belong to approximately the same pattern at the second measurement point (Bergman, Magnusson, & El-Khouri, 2003).
The present study
The present study aimed to examine PAHCO patterns, their stability over time and their associations with subjective health indicators. Examining these aspects is important, since it helps to develop tailored interventions to promote PAHCO. Compared to existing research, the longitudinal design of this investigation adds value. Previous studies were based mostly on cross-sectional data (Sudeck & Pfeifer, 2016). By focussing on PAHCO patterns, this study helps to clarify how PAHCO areas interact within individuals. In contrast to the current variable-oriented research, these person-oriented results allow us (to some extent) to make inferences pertaining to individuals rather than the group as a whole.
The following three research questions were posed:
- 1.
Which PAHCO patterns exist in people engaging in exercise in a primary prevention setting?
Here the aim was to identify patterns from two facets of control competence (control competence for physical training, PA-specific affect-regulation) and two facets of self-regulation competence (self-determined motivation for exercise, PA-specific self-control). The focus was on two competence areas, since there was no validated instrument available at the time of data collection to assess movement competence. Of particular interest was whether there are only level patterns, or whether shape patterns also exist. Level patterns have overall low, medium or high values across the PAHCO variables, and can therefore be placed on a continuum. In contrast, shape patterns have differing ratings across the variables (Morin, Boudrias, Marsh, Madore, & Desrumaux, 2016a). The detected patterns were then compared in terms of exercise behaviour. There were no hypotheses about the existence of specific patterns; however, there was a general assumption regarding the link between the PAHCO patterns and exercise behaviour. Individuals in patterns with high levels of PA-specific self-regulation competence were expected to be more physically active than people with low levels in these factors. Although all PAHCO areas are theoretically and empirically linked to exercise volume, it is the PA-specific self-regulation competence which should be particularly closely related, since it refers to the regularity of behaviour (Sudeck & Pfeifer, 2016).
- 2.
How stable are the PAHCO patterns over several months?
This study investigated both structural and individual stability. However, since there is no research on this topic, an explorative approach with no prior assumption was pursued.
- 3.
How is change in PAHCO patterns associated with change in subjective health indicators?
It was hypothesised that individuals who moved from a low to a more competent pattern would report health gains over time.
Methods
Procedures and participants
Participants of the study were recruited from university sport exercise courses.Footnote 1 The first data collection (T1) was at the beginning of the 2014 autumn semester. Individuals were invited by email to fill out an online questionnaire. If individuals completed the survey, they were eligible to win one of ten free memberships for a course in the paid university sports programme or one of 15 book vouchers worth € 20. The second data collection (T2) was 4 months later, at the end of the 2015 spring semester. All participants received information about the general purpose of the study, gave their written informed consent and were free to decline participation in line with the Declaration of Helsinki.
Of the 3603 individuals contacted (100.0%), 1374 completed the questionnaire at T1 (38.1%). Of these, 805 people (22.3%) also filled out the questionnaire at T2. In accordance with Wirtz (2004), individuals with >50% missing data were deleted. This was the case for 27 individuals. Nine more individuals were deleted due to the fact that they showed extreme response bias or were identified as multivariate outliers (Mahalanobis distance values as χ2 at p < 0.001; Tabachnick & Fidell, 2013). The analysis reported in this article is based on a final sample with data from 769 individuals (21.3%).
Characteristics of the final sample are shown in Table 1. A study dropout analysis was conducted by comparing those who participated only at T1 (n = 605) with those who completed both questionnaire assessments and were included in the longitudinal study (n = 769). Both the main study variables and the socio-demographic variables were examined. No differences were found for control competence for physical training, PA-related affect regulation, perceived vitality, exercise behaviour and sex. However, t‑tests revealed differences in PA-specific self-control [t(1247) = −2.50, p = 0.01, d = 0.14], self-determined motivation [t(1241) = −3.49, p = 0.01, d = 0.19], perceived fitness [t(1256) = −3.11, p < 0.005, d = 0.17], and age [t(1247) = −2.81, p = 0.01, d = 0.15]. Individuals that were included in this longitudinal study had higher PA-specific self-control, were more motivated, reported a higher fitness level and were older than those who participated only in the questionnaire at T1.
Measures
Control competence for physical training
Control competence for physical training was assessed at T1 and T2 with a six-item scale developed by Sudeck and Pfeifer (2016). Participants were asked to rate statements such as “If I want to enhance my health by strengthening trunk muscles (back, stomach), I am confident that I know the right exercises to do so” or “I can use my body signals (pulse, breathing speed) very well to gauge and regulate the amount of physical load”. The response format was a four-point scale ranging from 1 (“disagree completely”) to 4 (“agree completely”). The internal consistency of the scale was good (T1: α = 0.81; T2: α = 0.83). See also the electronic supplementary material Table 1 and Table 2 for descriptive statistics of the measures.
PA-related affect regulation
The competence for PA-related affect regulation was measured at T1 and T2 with a four-item scale (Sudeck & Pfeifer, 2016). Items included, for example “I am very able to improve my depressed mood by exercising” or “If I am feeling down, I can distract myself well through physical activity”. The response format was again a four-point scale ranging from 1 (“disagree completely”) to 4 (“agree completely”). The internal consistency of the scale was rated as good (T1/T2: α = 0.88).
PA-specific self-control
PA-specific self-control was assessed at T1 and T2 with a three-item scale (Sudeck & Pfeifer, 2016). Individuals were asked to rate statements such as “I stick with my plan to exercise and am not easily distracted from that plan” or “When I decide to exercise more, I am very disciplined in implementing this plan”. The response format was again a four-point scale ranging from 1 (“disagree completely”) to 4 (“agree completely”). The internal consistency of the scale was good (T1: α = 0.80; T2: α = 0.84).
Self-determined motivation for exercising
Self-determined motivation was measured at T1 and T2 using the exercise-related self-concordance scale by Seelig and Fuchs (2006). In contrast to well-known English scales, such as “the behavioural regulation in exercise” questionnaire (Markland & Tobin, 2004), this scale refers to the quality of intention, not the behaviour (Sheldon, 2014). However, it was used, since it is the only validated German questionnaire which measures the degree of internalisation. Previous research showed that the intrinsic and identified intentions correlate consistently positively with exercise. In contrast, findings for introjected and external regulation as well as for amotivation were somewhat mixed (Teixeira, Carraca, Markland, Silva, & Ryan, 2012). Consequently, it was focussed only on these two subscales and it was calculated a single score. By forming a composite score, it was possible to ensure that the PAHCO facets were represented in a balanced way. Including two different measures for self-determined motivation would mean giving the facet a “double weight” in relation to the other PAHCO facets in the latent profile analyses. The item stems of the subscales were: “I intend to exercise regularly within the next few weeks and months because …” and were followed by statements like “it’s just fun for me” (intrinsic), and “I have good reasons to be active” (identified). The response format was a six-point scale ranging from 1 (“not true”) to 6 (“exactly true”). The internal consistency of the score was rated satisfactory to good (T1: α = 0.73; T2: α = 0.80).
Subjective vitality
To assess subjective vitality at T1 and T2, a German version of the vitality scale with six items was used (Bostic, McGartland Rubio, & Hood, 2000; Goldbeck, Hautzinger, & Wolkenstein, 2019). Items on the scale included, for example “I feel energised” and “I feel alive and vital”. Individuals were asked to indicate to which degree the statements are true for them and their life in general. The seven-point rating scale ranged from 1 (“not at all true”) to 7 (“very true”). The internal consistency of the vitality scale was good (T1: α = 0.79; T2: α = 0.83).
Perceived fitness
Perceived physical fitness was measured at T1 and T2 with a modified version of a subscale from the adjective list for assessing perceived physical state (PEPS; Kleinert, 2006). Participants were asked to judge to what extent they feel “strong”, “fit”, “well-trained” and “enduring”. They were asked to answer on a six-point rating scale from 0 (“not at all”) to 5 (“totally”). The internal consistency for this subscale was good (T1: α = 0.84; T2: α = 0.83).
Exercise behaviour
To gather a comprehensive view of past exercise behaviour, four questions from a German version of the Baecke inventory were used at T1 (Baecke, Burema, & Frijters, 1982; Wagner & Singer, 2003). For example, participants were asked to report how many hours a week and how many months a year they exercise. An index was formed using these items in accordance with Baecke et al. (1982). At T2, current exercise behaviour was recorded instead of habitual behaviour. This was done in order to obtain more precise insight into exercise behaviour between the measurement time points. Therefore, two different instruments were combined: To assess university sport activities, participants named a maximum of five courses they had attended at least once in the past 15 weeks. They then indicated the frequency of participation for each course using five categories (≤2 times, 3–6 times, 7–9 times, 10–12 times, ≥13 times). The duration of activity per course was not requested, since it remained a weekly constant and the information was available to the project team. To assess activities beyond the scope of university sport a validated questionnaire by Fuchs, Klaperski, Gerber and Seelig (2015) was used. Participants specified a maximum of three exercise activities they had regularly engaged in within the previous 4 weeks. They indicated the frequency and duration per session in minutes for each activity. Based on this information from T2, a total index value in “hours per week” was calculated.
Data analyses
To identify the PAHCO patterns (research question 1), latent profile analyses were conducted separately for T1 and T2 (Masyn, 2013). Several indices were used to select the optimal number of patterns. The statistical indicators examined were the Bayesian information criterion (BIC), the adjusted BIC (aBIC), Akaike’s information criterion (AIC) and entropy and the Bootstrapped likelihood-ratio test (BLRT). Models with relatively low BIC, aBIC and AIC values as well as relatively high entropy values are preferred. In the BLRT, a p < 0.05 suggests that the k-pattern solution fits data better than the solution with k-1 patterns (Morin & Wang, 2016). The content-related indicators examined were the principle of parsimony, replication, theoretical consideration and the interpretability of the patterns found (Masyn, 2013; Morin & Wang, 2016). To further characterise the patterns, Wald tests were used to investigate their relationship with the exercise activity level (Lanza, Tan, & Bray, 2013).
To examine the stability of the PAHCO patterns (research question 2), a latent transition analysis was conducted. The procedure is a longitudinal extension of the latent profile analysis. The following three steps were carried out: Firstly, structural stability was investigated on an overall level by assessing measurement invariance of patterns between measurement points (Morin et al., 2016b). Therefore, two models were compared: a configural similarity model with freely estimated pattern indicator means between measurement points, and a structural similarity model with equal indicator means. To review the two models, a χ2 difference test using the maximum likelihood estimator (MLR) with Satorra-Bentler scaling correction was performed, and both BIC and aBIC were compared (Morin, Meyer, Creusier, & Biétry, 2016b; Olivera-Aguilar & Rikoon, 2018). Secondly, on a more specific level, an indicator of structural stability (SSi) was calculated by averaging squared Euclidian distance between two patterns. The lower the value, the more similar the considered patterns (Bergman et al., 2003). Thirdly, individual stability was investigated by estimating transitional probabilities, reflecting the probability of exhibiting a particular pattern at T2 given a particular pattern at T1.
To investigate the association between change in patterns and change in subjective health indicators (research question 3) on a global level, χ2 tests were used. Effect sizes (Cramer’s V) of the examined relationships were calculated. To investigate the association on a local level, a configural frequency analysis was performed using the χ2 approximation to the z‑test. This analysis allows us to test whether an individual cell in the cross table (see Table 3) comes with an observed frequency that is discrepant from the frequency that was expected for this cell (Wiedermann & von Eye, 2016). Due to estimation problems, the analyses for research question 3 were performed on a manifest level.
Analyses for research questions 1 and 2 were carried out in Mplus Version 7.4 (Muthén & Muthén, Los Angeles, CA, USA, 1998–2017) using maximum likelihood estimation with robust standard errors (MLR). Missing data (0.6% missing data points and 3.8% incomplete cases) were accommodated via full-information maximum likelihood (FIML). Analyses for research question 3 were run with SPSS Version 26 (IBM, New York, NY, USA) and the configural frequency analysis program Version 2000 (von Eye, 2001). The significance level was set at α = 0.05.
Data preparation
Since the analyses focussed on change in PAHCO patterns and in subjective health (research question 3), new variables were formed. On the one hand, individuals were classified regarding change in patterns between T1 and T2. Based on the findings of the latent transition analysis, they were categorised as: (1) Stayers if they remained in the same pattern over time, (2) upward movers if they transitioned to a pattern with higher competence scores or (3) downward movers if they transitioned to a pattern with lower competence scores. On the other hand, individuals were also classified regarding change in subjective vitality and perceived fitness over time. Initially, change scores were calculated separately for each health variable (T2 values—T1 values). Building on this, participants were categorised according to whether they experienced: (1) A decline, (2) no change or (3) an improvement in subjective health. No change was operationalised as 0 ± pooled standard deviation multiplied by 0.2, which represents a small effect (Sawilowsky, 2009).
Results
Identifying PAHCO patterns
Eight different latent-pattern solutions were tested and reported separately for T1 and T2 (see the electronic supplementary material Table 3). In general, BIC, aBIC and AIC improved considerably from one to two patterns. However, the indicators flattened out when more patterns were added, suggesting that these are only slightly better fitting models. All BLRTs were significant, which indicates that each model fitted the data better than a “one less” pattern model. However, entropy values of T1 pointed to a solution between six to eight patterns, meaning that the classification is precise enough in these models. In contrast, entropy values of T2 were less differentiated. An inspection of the content-related indicators revealed the seven-pattern solution as the most favoured model for both T1 and T2. They were theoretically meaningful, interpretable and relatively parsimonious (one pattern each was small, with <5% of all cases). Furthermore, the seven-pattern solution was replicated with the full sample (N = 1374; see the electronic supplementary material Fig. 1), whereas the six-pattern and eight-pattern solutions were not.
The seven-pattern solution for T1 and T2 is illustrated in Table 2 and in Fig. 1. Patterns 2, 5 and 7 have a level pattern with overall low, average and high values in all studied indicators. In contrast, patterns 1, 3, 4 and 6 have a shape pattern. Pattern 1 can be characterised with low levels in control competence for physical training, self-determined motivation and PA-specific self-control. What is striking about this pattern, however, is the very low PA-specific affect regulation. Pattern 3 has a similar shape to pattern 1, but at a higher level: average or slightly below average values for control competence for physical training, self-determined motivation and PA-specific self-control, but low PA-specific affect regulation. Pattern 4 can be characterised by low levels in control competence for physical training, PA-specific self-control and self-determined motivation, but an average level in PA-specific affect regulation. Pattern 6 has a somewhat horizontally-mirrored shape of pattern 3, i.e. average values for control competence for physical training, self-determined motivation and PA-specific self-control, but a high level in PA-specific affect regulation.
Wald tests revealed significant differences in exercise behaviour between patterns for both T1 (W = 194.47, p < 0.005) and T2 (W = 127.75, p < 0.005). Overall, the following results were apparent for both cross-sectional and longitudinal analysis: the more competent a pattern is, the more exercise activities are reported. In particular, patterns with a relatively high level of PA-specific self-control seem to be very active (see for instance pattern 5 vs. pattern 6, Table 2).
Structural and individual stability of the PAHCO patterns over time
To check the seven patterns for structural stability over time, the configural and structural similarity models were compared. The detailed results of this measurement invariance check are reported in the electronic supplementary material Table 4. The χ2 difference test indicated no significant worsening of fit if indicator means between measurement points were held equal [χ2 (28) = 35.89, p = 0.15]. Furthermore, the structural similarity model resulted in slightly lower values in BIC and aBIC. Both results indicate that the seven patterns remain stable overall and can be interpreted in the same way over time. However, if one looks on a more specific level by comparing the average squared Euclidian distances between patterns, slight differences in structural stability are noticeable: the structural stability of pattern 1, for instance, was lower (SSi = 0.11) than that of pattern 7 (SSi < 0.005; see Fig. 1).
Fig. 2 shows the transitional probabilities with which individual stability over time can be assessed. Given that the patterns observed are consistent across T1 and T2, this model was estimated with structural measurement invariance (Morin & Wang, 2016). It is noteworthy, however, that this procedure did not impose any restriction on pattern size. As a whole, the analysis revealed that most individuals remain within the same pattern over time. This seems to be particularly true for individuals in a pattern with relatively high competence scores at T1 (e.g. pattern 7). Nevertheless, it is important to point out that some individuals changed PAHCO patterns. For instance, individuals from pattern 1 were quite likely to move to pattern 2 (transitional probability = 0.38). Similarly, individuals from pattern 3, with 0.39, had a relatively high probability of changing to pattern 5. Consequently, individuals in these groups are relatively likely to improve their competence over time.
Associations of changes in PAHCO patterns and changes in subjective health indicators over time
To investigate associations between change in PAHCO patterns and change in subjective health, individuals were first categorised based on their transition between patterns across time. A total of 552 individuals (71.8%) were identified as stayers, 158 individuals (20.5%) as upward movers, and 59 individuals (7.7%) as downward movers. Overall, the χ2 test revealed that these changes in the PAHCO patterns were associated with changes in subjective vitality [χ2 (4) = 12.39, p = 0.02]. However, the effect was small (V = 0.09). The frequency distribution and the local z-test reported in Table 3 allow a more differentiated view of the relationship between the two variables. Particularly noticeable is that individuals who moved in a pattern with lower competence scores perceived lower vitality more often than expected (z = 2.320, p = 0.01). They also perceived stable vitality less often over time than expected (z = −1.820, p = 0.03). Furthermore, changes in patterns overall were related to changes in perceived fitness [χ2 (4) = 16.87, p < 0.005]. This effect was also small (V = 0.11). When looking at the frequency distribution, the upward movers stand out: they reported an improvement in perceived fitness more often than expected (z = 1.995, p = 0.02) and a decline in perceived fitness less often than expected (z = −1.865, p = 0.03). The opposite pattern of results was found in the case of the downward movers (declined: z = 2.289, p = 0.01; improved: z = −1.839, p = 0.03).
Discussion
The present study aimed to: 1) Identify PAHCO patterns, 2) examine how structurally and individually stable these patterns are over 4 months and 3) test how changes in patterns are associated with changes in subjective health indicators. This study extends previous variable-oriented research by looking at the interplays of PAHCO within an individual rather than examining isolated variables on an aggregated group-level. With this person-oriented approach, a method was pursuided that has recently been identified as a promising field for future competence research (Cairney et al., 2019).
Regarding control competence for physical training, PA-specific affect regulation (as facets for PA control competence), self-determined motivation for exercise and PA-specific self-control (as facets of PA-specific self-regulation competence), a model with seven patterns proved to be the most optimal solution. Four of the seven patterns have a shape pattern with differing ratings across the PAHCO areas and/or facets (Morin et al., 2016a). Thus, such interactions of variables within individuals would have remained undetected had a variable-oriented approach been applied. A closer look at the four patterns reveals that it is often the two facets of PA control competence which contrast with each other. For instance, people with pattern 6 (T1/T2: 18% of the sample) have an average value in control competence for physical training, but a high level in PA-specific affect regulation. One might speculate that these individuals usually engage in stress-reducing or recreational activities (e.g. walking, yoga; Asztalos et al., 2012). In contrast to the aforementioned result, the facets of self-regulation competence were parallel: self-determined motivation for exercise and PA-specific self-control did not have different levels in any of the identified patterns. This result is in line with the study by Grimm and Krämer (2014), who also showed that motivational and volitional factors are often equally pronounced within individuals. These findings raise the question of whether the phenomenon of the intention–behaviour gap can also be found using a person-oriented method (Rhodes & De Bruijn, 2013). In addition, the hypothesised link between PAHCO patterns and exercise behaviour was found. The highest amounts of exercise activities were observed for people with a pattern of high levels in PA-specific self-regulation competence. This longitudinal result is consistent with existing cross-sectional research about PAHCO (Sudeck & Pfeifer, 2016) and with the more general literature about social cognitive models of health behaviour (e.g. Biddle & Fuchs, 2009).
The identified patterns proved to be structurally stable over 4 months, meaning that they were very similar on a group level. Results on the individual level showed that around 70% of the sample stayed in the same pattern, whereas the remaining 30% moved to another pattern. However, moving to a more competent pattern was much more likely than changing to a less competent pattern. Only 7.7% of the individuals were classified as downward movers and no specific transition downwards was disproportionately frequent (see Fig. 2). This finding could be related to the fact that people took part in supervised exercise courses for several months. However, it should be clearly stressed that individuals did not receive a target intervention aimed at promoting PAHCO. Against this background, the results on individual stability are remarkable. The increase in PAHCO was relatively high in some subgroups. For instance, individuals that moved from pattern 3 to pattern 5 improved their PAHCO by around 0.24 ≤ MDiff ≤ 0.86. If, in contrast, one looks only (in a variable-oriented manner) at the development of the overall sample, hardly any change can be observed (0.03 ≤ MDiff ≤ 0.13; see the electronic supplementary material Table 1). This comparison illustrates once again how beneficial the differential view of the person-oriented approach can be.
Change in PAHCO patterns overall was associated with change in subjective health indicators. The hypothesised effects were confirmed for both perceived fitness and subjective vitality. The authors analysed the association between change in patterns and change in subjective health on a comparatively general level, by dividing people into stayers, upward movers and downward movers. A consequence of using such broad categories is that information about PAHCO change is lost. It therefore remains unclear whether specific changes in PAHCO have specific health effects. For example, it can be assumed that individuals who moved from a pattern with low PA-specific affect regulation to a pattern with a higher value in this competence facet might profit particularly in vitality (Sudeck et al., 2018; Sudeck & Pfeifer, 2016). Furthermore, it remains unanswered whether moving from a low to a medium competent pattern has the same effect on subjective health as moving from a medium to a high competent pattern.
Limitations and future directions
The current study has various limitations which must be addressed: Firstly, dropout analysis showed that our longitudinal study sample is distorted. For example, individuals were more likely to participate in the survey twice when they had relatively high PA-specific self-control. However, effect size analyses were relatively small (d < 0.2), so the sample might be only negligibly biased. Nevertheless, future studies should investigate whether the results are replicable in a new sample with healthy adults. In addition, one could examine whether the findings can be transferred to other populations, such as adolescents or patients with chronic diseases. Of particular interest would be to investigate whether only the size of the subgroups varies, or whether other patterns are found. Secondly, due to the lack of a suitable measuring instrument, the authors did not consider movement competence in this investigation. However, the first attempts to cover this important area of PAHCO are currently being made by Carl, Sudeck, Geidl and Pfeifer (2020). Consequently, movement competence could be integrated into further research. Thirdly, in the present investigation, the authors concentrate on associations between change in PAHCO patterns and change in subjective health. However, they did not focus on the role PA behaviour may play in these relations. Future studies should examine the specific mechanism. Finally, all study variables were assessed by self-report. Therefore, individuals’ statements may not accurately represent their objective competence or health. For instance, one cannot rule out the possibility that social desirability influenced our data (e.g. people reported improved health after they participated in exercise courses due to the fact that this is viewed favourably by others).
Conclusion
In conclusion, the results presented here demonstrate the added value of a person-oriented approach to investigating development of PAHCO facets over several months. This differential approach helps to generate knowledge about distinct subgroups and provides the basis for developing tailored interventions to more efficiently promote PAHCO in a primary prevention setting (Thiel, Pfeifer, & Sudeck, 2018). Ultimately, the aim is to empower individuals to embrace an active lifestyle that leads to optimal effects on health and well-being.
Notes
The sample described here is identical to sample B in the study by Sudeck and Pfeifer (2016).
References
Asztalos, M., Wijndaele, K., de Bourdeaudhuij, I., Philippaerts, R., Matton, L., Duvigneaud, N., Cardon, G., et al. (2012). Sport participation and stress among women and men. Psychology of Sport and Exercise, 13(4), 466–483. https://doi.org/10.1016/j.psychsport.2012.01.003.
Baecke, J. A., Burema, J., & Frijters, J. E. (1982). A short questionnaire for the measurement of habitual physical activity in epidemiological studies. The American Journal of Clinical Nutrition, 36(5), 936–942. https://doi.org/10.1093/ajcn/36.5.936.
Beauchamp, M. R., Puterman, E., & Lubans, D. R. (2018). Physical inactivity and mental health in late adolescence. Journal of the American Medical Association Psychiatry,, 75(6), 543–544. https://doi.org/10.1001/jamapsychiatry.2018.0385.
Bergman, L. R., & Lundh, L.-G. (2015). Introduction. The person-oriented approach: roots and roads to the future. Journal for Person-Oriented Research, 1(1–2), 1–6. https://doi.org/10.17505/jpor.2015.01.
Bergman, L. R., & Magnusson, D. (1997). A person-oriented approach in research on developmental psychopathology. Development and Psychopathology, 9, 291–319.
Bergman, L. R., Magnusson, D., & El-Khouri, B. M. (2003). Studying individual development in an inter-individual context. A person-oriented approach. Mahwah: Erlbaum.
Biddle, S. J. H., & Fuchs, R. (2009). Exercise psychology: a view from Europe. Psychology of Sport and Exercise, 10(4), 410–419. https://doi.org/10.1016/j.psychsport.2009.02.011.
Bostic, T. J., McGartland Rubio, D., & Hood, M. (2000). A validation of the subjective vitality scale using structural equation modeling. Social Indicators Research, 52(3), 313–324. https://doi.org/10.1023/A:1007136110218.
Cairney, J., Dudley, D., Kwan, M., Bulten, R., & Kriellaars, D. (2019). Physical literacy, physical activity and health: toward an evidence-informed conceptual model. Sports Medicine, 49(3), 371–383. https://doi.org/10.1007/s40279-019-01063-3.
Carl, J., Sudeck, G., Geidl, W., & Pfeifer, K. (2020). Competencies for a healthy physically active lifestyle—validation of an integrative model. ResearchSquare. https://doi.org/10.21203/rs.2.20632/v1.
Deci, E. L., & Ryan, R. M. (2000). The “What” and “Why” of goal pursuits: Human needs and the self-determination of behavior. Psychological Inquiry, 11, 227–268.
Edwards, L. C., Bryant, A. S., Keegan, R. J., Morgan, K., & Jones, A. M. (2017). Definitions, foundations and associations of physical literacy: a systematic review. Sports Medicine, 47(1), 113–126. https://doi.org/10.1007/s40279-016-0560-7.
Von Eye, A. (2001). Configural frequency analysis—version 2000. A program for 32 bit windows operating systems. Methods of Psychological Research Online, 6(2), https://www.dgps.de/fachgruppen/methoden/mpr-online/issue14/index.html
Fuchs, R., Klaperski, S., Gerber, M., & Seelig, H. (2015). Messung der Bewegungs- und Sportaktivität mit dem BSA-Fragebogen: Eine methodische Zwischenbilanz [Measurement of physical activity and sport activity with the BSA questionnaire]. Zeitschrift für Gesundheitspsychologie, 23, 60–76. https://doi.org/10.1026/0943-8149/a000137.
Geidl, W., Semrau, J., Streber, R., Lehbert, N., Wingart, S., Tallner, A., Pfeifer, K., et al. (2017). Effects of a brief, pedometer-based behavioral intervention for individuals with COPD during inpatient pulmonary rehabilitation on 6‑week and 6‑month objectively measured physical activity: Study protocol for a randomized controlled trial. Trials, 18(1), 396. https://doi.org/10.1186/s13063-017-2124-z.
Giblin, S., Collins, D., & Button, C. (2014). Physical literacy: Importance, assessment and future directions. Sports Medicine, 44(9), 1177–1184. https://doi.org/10.1007/s40279-014-0205-7.
Goldbeck, F., Hautzinger, M., & Wolkenstein, L. (2019). Validation of the German version of the subjective vitality scale—a cross-sectional study and a randomized controlled trial. Journal of Well-Being Assessment, 3(1), 17–37. https://doi.org/10.1007/s41543-019-00019-8.
Gollwitzer, P., & Oettingen, G. (2016). Planning promotes goal striving. In K. D. Vohs & R. F. Baumeister (Eds.), Handbook of self-regulation: research, theory, and applications (pp. 223–244). New York, London: Guilford.
Grimm, N. C. I., & Krämer, L. V. (2014). Sportliche (In‑)Aktivität depressiver Patienten: Eine clusteranalytische Unterscheidung von motivationalen und volitionalen Typen [Physical (in)activity in depressive patients: A cluster analytic differentiation of motivational and volitional types]. Zeitschrift für Klinische Psychologie und Psychotherapie, 43(2), 104–111. https://doi.org/10.1026/1616-3443/a000255.
Haible, S., Volk, C., Demetriou, Y., Höner, O., Thiel, A., Trautwein, U., & Sudeck, G. (2019). Promotion of physical activity-related health competence in physical education: study protocol for the GEKOS cluster randomized controlled trial. BioMed Central Public Health, 19(1), 396. https://doi.org/10.1186/s12889-019-6686-4.
Kleinert, J. (2006). Adjektivliste zur Erfassung der Wahrgenommenen Körperlichen Verfassung (WKV) [Adjective list for assessing Perceived Physical State (PEPS). Scale construction and psychometric results]. Zeitschrift für Sportpsychologie, 13(4), 156–164. https://doi.org/10.1026/1612-5010.13.4.156.
Klieme, E., Hartig, J., & Rauch, D. (2008). The concept of competence in educational contexts. In J. Hartig, E. Klieme & D. Leutner (Eds.), Assessment of Competencies in Educational Contexts (1st edn., pp. 3–22). Göttingen: Hogrefe Publishing.
Lanza, S. T., Tan, X., & Bray, B. C. (2013). Latent class analysis with distal outcomes: a flexible model-based approach. Structural Equation Modeling: a Multidisciplinary Journal, 20(1), 1–26. https://doi.org/10.1080/10705511.2013.742377.
Lubans, D. R., Richards, J., Hillman, C., Faulkner, G., Beauchamp, M. R., Nilsson, M., Biddle, S. J. H., et al. (2016). Physical activity for cognitive and mental health in youth: a systematic review of mechanisms. Pediatrics. https://doi.org/10.1542/peds.2016-1642.
Markland, D., & Tobin, V. (2004). A modification to the behavioural regulation in exercise questionnaire to include an assessment of amotivation. Journal of Sport & Exercise Psychology, 26, 191–196.
Masyn, K. E. (2013). Latent class analysis and finite mixture modeling. In T. D. Little (Ed.), The Oxford handbook of quantitative methods in psychology. Statistical analysis, (Vol. 2, pp. 551–611). New York: Oxford University Press. https://doi.org/10.1093/oxfordhb/9780199934898.013.0025.
Morin, A. J. S., & Wang, J. C. K. (2016). A gentle introduction to mixture modeling using physical fitness performance data. In N. Ntoumanis & N. D. Myers (Eds.), An introduction to intermediate and advanced statistical analyses for sport and exercise scientists (pp. 183–209). London: Wiley.
Morin, A. J. S., Boudrias, J.-S., Marsh, H. W., Madore, I., & Desrumaux, P. (2016a). Further reflections on disentangling shape and level effects in person-centered analyses: an illustration exploring the dimensionality of psychological health. Structural Equation Modeling: a Multidisciplinary Journal, 23(3), 438–454. https://doi.org/10.1080/10705511.2015.1116077.
Morin, A. J. S., Meyer, J. P., Creusier, J., & Biétry, F. (2016b). Multiple-group analysis of similarity in latent profile solutions. Organizational Research Methods, 19(2), 231–254. https://doi.org/10.1177/1094428115621148.
Muthén, L. K., & Muthén, B. O. (1998–2017). Mplus user’s guide. Los Angeles: Muthén & Muthén.
Olivera-Aguilar, M., & Rikoon, S. H. (2018). Assessing measurement invariance in multiple-group latent profile analysis. Structural Equation Modeling: a Multidisciplinary Journal, 25(3), 439–452. https://doi.org/10.1080/10705511.2017.1408015.
Pfeifer, K., Sudeck, G., Geidl, W., & Tallner, A. (2013). Bewegungsförderung und Sport in der Neurologie – Kompetenzorientierung und Nachhaltigkeit [Physical activity promotion in neurology—competence orientation and sustainability. Neurologie und Rehabilitation, 19(1), 7–19.
Rhodes, R. E., & De Bruijn, G.-J. (2013). How big is the physical activity intention-behaviour gap? A meta-analysis using the action control framework. British Journal of Health Psychology, 18(2), 296–309. https://doi.org/10.1111/bjhp.12032.
Sawilowsky, S. S. (2009). New effect size rules of thumb. Journal of Modern Applied Statistical Methods, 8(2), 597–599. https://doi.org/10.22237/jmasm/1257035100.
Seelig, H., & Fuchs, R. (2006). Messung der sport- und bewegungsbezogenen Selbstkonkordanz [Measuring sport- and exercise-related self-concordance]. Zeitschrift für Sportpsychologie, 13, 121–139. https://doi.org/10.1026/1612-5010.13.4.121.
Sheldon, K. M. (2014). Becoming oneself: the central role of self-concordant goal selection. Personality and Social Psychology Review, 18(4), 349–365. https://doi.org/10.1177/1088868314538549.
Sørensen, K., van den Broucke, S., Fullam, J., Doyle, G., Pelikan, J., Slonska, Z., & Brand, H. (2012). Health literacy and public health: a systematic review and integration of definitions and models. BioMed Central Public Health, 12, 80. https://doi.org/10.1186/1471-2458-12-80.
Sudeck, G., & Pfeifer, K. (2016). Physical activity-related health competence as an integrative objective in exercise therapy and health sports—conception and validation of a short questionnaire. Sportwissenschaft, 46(2), 74–87. https://doi.org/10.1007/s12662-016-0405-4.
Sudeck, G., Jeckel, S., & Schubert, T. (2018). Individual differences in the competence for physical-activity-related affect regulation moderate the activity-affect association in real-life situations. Journal of Sport & Exercise Psychology, 40(4), 196–205. https://doi.org/10.1123/jsep.2018-0017.
Tabachnick, B. G., & Fidell, L. S. (2013). Using multivariate statistics (6th edn.). Boston: Pearson Education.
Teixeira, P. J., Carraca, E. V., Markland, D., Silva, M. N., & Ryan, R. M. (2012). Exercise, physical activity, and self-determination theory: a systematic review. International Journal of Behavioral Nutrition and Physical Activity, 9, 78–108. https://doi.org/10.1186/1479-5868-9-78.
Thiel, C., Pfeifer, K., & Sudeck, G. (2018). Pacing and perceived exertion in endurance performance in exercise therapy and health sports. German Journal of Exercise and Sport Research, 38(3), 239. https://doi.org/10.1007/s12662-017-0489-5.
Töpfer, C., & Sygusch, R. (2014). Gesundheitskompetenz im Sportunterricht [Health competence in physical education. In S. Becker (Ed.), Aktiv und Gesund?: Interdisziplinäre Perspektiven auf den Zusammenhang zwischen Sport und Gesundheit (pp. 153–179). Wiesbaden: Springer VS.
Wagner, P., & Singer, R. (2003). Ein Fragebogen zur Erfassung der habituellen körperlichen Aktivität verschiedener Bevölkerungsgruppen [A questionnaire for the registration of the habitual physical activity of different groups of population]. Sportwissenschaft, 33, 385–397.
Warburton, D. E. R., & Bredin, S. S. D. (2017). Health benefits of physical activity: A systematic review of current systematic reviews. Current Opinion in Cardiology, 32(5), 541–556. https://doi.org/10.1097/HCO.0000000000000437.
Wiedermann, W., & von Eye, A. (2016). Local associations in latent class analysis: using configural frequency analysis for model evaluation. Journal for Person-Oriented Research. https://doi.org/10.17505/jpor.2016.15.
Wirtz, M. (2004). Über das Problem fehlender Werte: Wie der Einfluss fehlender Informationen auf Analyseergebnisse entdeckt und reduziert werden kann [On the problem of missing data: How to identify and reduce the impact of missing data on findings of data analysis]. Die Rehabilitation, 43(2), 109–115. https://doi.org/10.1055/s-2003-814839.
World Health Organization (2018). Global action plan on physical activity 2018–2030: More active people for a healthier world. Geneva: World Health Organization.
Acknowledgements
The authors would like to thank Professor M. Hautzinger and F. Goldbeck for their preparatory work in developing and validating the German version of the subjective vitality scale.
Funding
Open Access funding provided by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J. Schmid, S. Haible and G. Sudeck declare that they have no competing interests.
All procedures performed in studies involving human participants or on human tissue were in accordance with the ethical standards of the institutional and/or national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Caption Electronic Supplementary Material
Rights and permissions
Open Access. This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schmid, J., Haible, S. & Sudeck, G. Patterns of physical activity-related health competence: stability over time and associations with subjective health indicators. Ger J Exerc Sport Res 50, 218–228 (2020). https://doi.org/10.1007/s12662-020-00650-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12662-020-00650-1