Abstract
Introduction
Obstructive sleep apnea (OSA) may increase the incidence of postoperative complications when undiagnosed. The purpose of this study was to evaluate the perspectives of Canadian anesthesiologists regarding the perioperative management of patients with diagnosed or suspected OSA.
Methods
This study was conducted as a survey of Canadian anesthesiologists using a self-administered scenario-based questionnaire. We initially mailed the survey questionnaire and then mailed it again to non-respondents six weeks later. Subsequently, we e-mailed the online version of our survey to active members of the Canadian Anesthesiologists’ Society.
Results
The response rates were 35% and 26% for the postal and online modes of administration, respectively. About 50% of the respondents relied on clinical suspicion rather than on a systematic screening to identify patients who may have undiagnosed OSA preoperatively. Forty-seven percent of all respondents either did not know of any institutional policy to guide their perioperative management of patients with OSA or reported an absence of an institutional policy. Fifteen percent of the respondents would discharge diagnosed OSA inpatients with compliant use of continuous positive airway pressure (CPAP) to the ward without monitoring. Nevertheless, a more conservative approach was observed for CPAP non-compliant inpatients. We indeed observed that more than 40% of respondents would send an ambulatory OSA patient home, while another 60% would favour hospital admission.
Conclusions
The majority of anesthesiologists continue to rely on clinical suspicion alone to identify OSA. Moreover, the lack of institutional policy is concerning. A concerted effort to develop an evidence-based guideline may be the next step to assist institutions.
Résumé
Introduction
L’apnée obstructive du sommeil (AOS), si elle n’est pas dépistée, peut augmenter l’incidence de complications postopératoires. L’objectif de cette étude était d’évaluer les perspectives des anesthésiologistes canadiens quant à la prise en charge périopératoire des patients atteints d’AOS reconnue ou soupçonnée.
Méthode
Cette étude a été réalisée sous forme de sondage auprès des anesthésiologistes canadiens à l’aide d’un questionnaire auto-administré basé sur des scénarios cliniques. Nous avons envoyé le questionnaire par la poste, puis l’avons renvoyé six semaines plus tard aux personnes n’ayant pas répondu. Par la suite, nous avons envoyé une version en ligne par courriel aux membres actifs de la Société canadienne des anesthésiologistes.
Résultats
Les taux de réponse étaient de 35 % et 26 % aux questionnaires envoyés par la poste et par courriel, respectivement. Environ 50 % des répondants affirment se fonder sur une suspicion clinique plutôt que sur un dépistage méthodique pour identifier les patients potentiellement atteints d’AOS non diagnostiquée en période préopératoire. En tout, 47 % des répondants ne savaient pas s’il existait une quelconque politique institutionnelle orientant leur prise en charge périopératoire des patients atteints d’AOS ou rapportaient l’absence d’une telle politique institutionnelle. Quinze pour cent des répondants transfèreraient à l’étage des patients hospitalisés souffrant d’AOS diagnostiquée avec une prescription générale pour leur dispositif de ventilation à pression positive continue (CPAP) et n’installeraient pas de monitorage. Toutefois, une approche plus conservatrice a été observée en matière de prise en charge des patients hospitalisés qui hésitent à utiliser un CPAP. En effet, nous avons observé que plus de 40 % des répondants donneraient le congé à un patient atteint d’AOS en clinique d’un jour, alors que 60 % favoriseraient une admission à l’hôpital.
Conclusion
La majorité des anesthésiologistes continuent de s’appuyer sur leur seule suspicion clinique pour identifier l’AOS. De plus, l’absence de politique institutionnelle est préoccupante. Un effort concerté visant à mettre au point une recommandation fondée sur des données probantes devrait constituer la prochaine étape pour soutenir les institutions.
Similar content being viewed by others
Obstructive sleep apnea (OSA), the most prevalent sleep-disordered breathing condition, is defined by repetitive partial or complete upper airway obstruction leading to episodes of breathing cessation during sleep. The prevalence of OSA among the general population aged 30-70 yr is 5% in females and 14% in males.1
Undiagnosed OSA may increase the incidence of postoperative complications.2,3 A significant proportion of patients with a diagnosis of OSA are not identified by surgeons and anesthesiologists prior to surgery.4–7 Although screening questionnaires and clinical screening models have been developed to identify patients with OSA prior to their surgery,8–10 careful screening is frequently not implemented before surgery.4–7 It is recommended that additional monitoring of patients with known or suspected OSA be carried out in the postoperative period, but the degree to which this occurs and the nature of the additional monitoring required have not been well characterized.11–14 A protocol for the perioperative management of OSA patients based on the experience of Canadian and US centres was recently published.12 Prior to the publication of these guidelines and protocol, a survey of Canadian anesthesiologists on postoperative management of OSA patients was conducted and published in the Journal.15 Nevertheless, it is not known whether either of these publications have had an impact on the perioperative management of OSA patients.16
The purpose of this study was to evaluate the perspectives of Canadian anesthesiologists regarding the perioperative management of patients with diagnosed or suspected OSA. The primary objective was to evaluate the screening procedure, preparation for surgery, mode of postoperative monitoring, and disposition of diagnosed OSA patients.
A secondary objective was to determine if management of patients with OSA varied dependent upon whether they were treated with continuous positive airway pressure (CPAP) or with an inpatient/outpatient model of care. Finally, we sought to determine if anesthesiologists’ preferred management strategies were constrained by hospital resources.
Methods
Study design
This study was conducted as a survey of clinicians using a formal self-administered questionnaire. The design of this study followed suggested recommendations for conducting healthcare surveys.17
Study population and sampling frame
The target population included anesthesiologists providing anesthesia in healthcare facilities in Canada. Eligible physicians were initially identified using a mailing list provided by Cornerstone List Brokerage, a commercial list broker. The Cornerstone list was compiled by the publisher of the Canadian Medical Directory, one of the most comprehensive sources for contact information on doctors across Canada and officially endorsed by the Canadian Medical Association. The list yielded a sampling frame of 2,734 certified anesthesiologists. This sampling frame was used for the postal survey. We then approached the Canadian Anesthesiologists’ Society (CAS) for permission to survey its active members. The Society’s membership list yielded a sampling frame of 1,782 active members for the online survey. Some names in the sampling frame of 2,734 certified anesthesiologists could be included in the sampling frame of 1,782 active members of the CAS for the online survey.
Survey development
Item generation
Experts in perioperative anesthesia management (F.C., A.F.T., R.H., P.T.C., and G.L.B.) identified potential important key categories and themes to evaluate. A list of items was generated and expanded with input from all of the investigators.
Domains and items reduction
The importance of each domain and item was ranked by all content experts. At the end of the process, the following domains emerged: type of patient, type of surgical scenario, screening procedure, preparation for surgery, level and duration of monitoring, and discharge location after anesthesia.
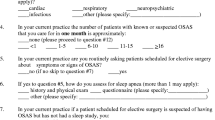
Questionnaire formatting
We developed the questionnaire using scenario-based questions (Appendix in Supplementary Material). Two scenarios were used: an inpatient scenario of an open right hemicolectomy (Section 1) and an outpatient scenario of a laparoscopic cholecystectomy (Section 2). For each scenario, we modified the same patient with three possible OSA states: diagnosed OSA with compliant use of nocturnal continuous positive airway pressure (CPAP), diagnosed OSA with non-compliant use of nocturnal CPAP, and suspected OSA. The two initial scenarios and three OSA states generated six final possible scenarios. For all six scenarios, four questions were posed regarding the postoperative period, the level and duration of monitoring, and the discharge location after anesthesia. For the scenarios involving diagnosed OSA with non-compliant use of CPAP or suspected OSA, an additional question was posed regarding the preparation for surgery. Each question focused on a single construct. We used a closed nominal format with or without indeterminate options (depending on the question) for the responses. Specifically, we sought to answer the following questions:
-
1.
For patients with suspected OSA, how are they identified (screening procedure)?
-
2.
For patients with suspected OSA or diagnosed OSA non-compliant with CPAP, how are they managed preoperatively (preparation for surgery and mode of postoperative monitoring)?
-
3.
For patients with suspected OSA or diagnosed OSA compliant with CPAP, how are they managed preoperatively (preparation for surgery and mode of postoperative monitoring)?
-
4.
For patients with suspected OSA or diagnosed OSA, in what location is the postoperative monitoring occurring? What is the duration of additional monitoring provided?
-
5.
For patients with suspected OSA or diagnosed OSA, are the anesthesiologists’ preferred management strategies constrained by hospital resources?
Questionnaire testing
Pretesting
The Perioperative Anesthesia Clinical TrialsFootnote 1 group members then distributed the full draft questionnaire and cover letter to collaborators. The collaborators analyzed the study instrument focusing on clarity, interpretation, and the objectives of the questions.
Clinical sensibility testing
We asked 15 anesthesiologists to assess the comprehensiveness, clarity, and face validity of the questionnaire using a one-page assessment sheet with Likert scale responses.
Reliability
To assess reliability, ten anesthesiology residents / fellows were asked to complete the survey twice with a two-week interval between the two surveys. Test-retest reliability was calculated based on generalizability theory. The questionnaire was considered adequately reliable if r was 0.4 or higher (Pearson correlation).
Administration
We administered the survey questionnaire using two methods. First, we mailed the survey questionnaire (along with a cover letter explaining the objective of the study and a pre-stamped envelope for return) to anesthesiologists randomly identified by Cornerstone List Brokerage. All the questionnaires were coded with a unique identification number to allow for a second mailing to non-respondents. The identities of respondents remained confidential. For non-respondents, we sent a cover letter and the questionnaire again six weeks later. Subsequently, the CAS e-mailed all of its active members with a link to the online version of our survey, which was administered using FluidSurveys™. To avoid duplication of responses, the online survey prevented individuals from responding if they indicated that they had submitted responses to the survey by mail. The survey modalities were mutually exclusive, but it is possible that duplications of surveys can occur, as it is self-reporting. The postal survey used the English questionnaire only. For the online survey, a French translated version of the questionnaire was also sent along with the English version.
Statistical considerations
Response rate and sample size
Based on the sample size formula for cross-sectional descriptive survey design described by Dillman,18 assuming maximal variability in the responses (P = 0.5), a precision within 3%, and a 95% two-sided confidence interval, 1,505 recipients were needed for an approximate response rate of 51%.
Data analysis
Test-retest reliability was calculated using G String IV version 6.11 (McMaster University, Hamilton, ON, Canada). The response data were analyzed using Stata® 10 (StataCorp LP, TX, USA). We defined the response rate for each mode of survey administration as the percentage of questionnaires that were returned from each mode of administration. We limited our analysis of responses from each section to questionnaires with answers to at least 11 of 14 questions in Section 1, at least six of eight questions in Section 2, and at least five of six questions in the practice demographics section. We described the respondents’ choices to each question using percentages. No inferential statistics were performed.
Results
The final survey questionnaire consisted of 28 questions (Appendix in Supplementary Material). Test-retest reliability was moderate (r = 0.65). In the spring of 2012, 1,500 of the 2,734 anesthesiologists identified by the Cornerstone List Brokerage received our survey questionnaire by mail. In the autumn of 2012, all active members of the CAS with e-mail addresses (1,730 of 1,782) were invited to participate in the online survey. The response rates were 35% (534 / 1,500) and 26% (458 / 1,730) for the postal and online modes of administration, respectively. Ten of the 1,002 questionnaires were excluded due to inadequate responses as defined in the methods. Of the 992 questionnaires included in the analysis, 773 contained responses to at least 11 of 14 questions in Section 1; 743 contained responses to at least six of eight questions in Section 2, and 773 contained responses to at least five of six questions in the practice demographics section.
Respondents and practice demographics
Table 1 summarizes the practice demographics of the respondents. Regarding the presence of an institutional policy to guide the management of patients with OSA, 53% (413/773) of the respondents indicated the presence of a policy, 34% (259/773) of the respondents specified that no policy was present in their institution, and the remainder (13%; 101/773) did not know. Regarding access to different types of clinical units in their institutions, 89% (685/773) of the respondents had access to intensive care units, 57% (439/773) had access to stepdown units with continuous monitoring, 48% (374/773) had access to ward beds with telemetry (oximetry and/or echocardiogram and/or end-tidal CO2), 79% (609/773) had access to ward beds with intermittent oximetry monitoring, and 59% (455/773) had access to noninvasive ventilation on regular surgical wards.
Open hemicolectomy scenario
Table 2 summarizes the various monitoring locations after discharge from the postanesthetic care unit.
For a patient with a documented history of OSA and compliant with CPAP therapy, 65% (507/772) of the respondents would monitor such a patient after surgery in the postanesthetic care unit (PACU) for the same duration as someone without OSA, 30% (232/772) would monitor the patient for up to an additional six hours in the PACU, 2% (15/772) would transfer the patient directly to another unit from the operating room, and the remainder would monitor the patient for over six to 12 hr (0.8%; 6/772), over 12-24 hr (0.8%; 6/772), or over 24 hr (0.8%; 6/772) in the PACU. After discharge to a regular ward without telemetry, 35% (273/770) of the respondents would measure vital signs every four hours, 19% (145/770) every hour, 16% (124/770) every two hours, and 8% (63/770) every eight hours. Sixteen percent (125/770) did not know.
For a patient with documented OSA and non-compliance with CPAP therapy, 89% (691/772) of the respondents would proceed with anesthesia with OSA precautions (avoiding premedication, preparing for a possible difficult airway, minimizing the use of opioids), 6% (46/772) would proceed with anesthesia without further actions, and 2% (21/772) would defer surgery and refer the patient to a sleep physician or respirologist. After surgery, 44% (343/769) of the respondents would monitor such a patient for the same duration as someone without OSA in the PACU, 42% (325/769) would monitor the patient for up to an additional six hours in the PACU, 5% (37/769) would monitor the patient for over six to 12 hr, 4% (30/769) would monitor the patient for over 12-24 hr, 3% (24/769) would transfer the patient directly to another unit from the operating room, and 1% (10/769) would monitor the patient for over 24 hr in the PACU. After discharge to a regular ward without telemetry, 30% (234/770) of the respondents would measure vital signs every hour, 28% (219/770) every four hours, 17% (134/770) every two hours, and 7% (52/770) every eight hours. Nine percent (68/770) did not know.
To identify patients who may have undiagnosed OSA preoperatively, 50% (385/772) of the respondents specified relying on clinical suspicion alone, 30% (231/772) specified using a screening questionnaire in cases where OSA is clinically suspected, 18% (139/772) specified using a screening questionnaire for all patients, and 2% (18/772) specified not screening for OSA at all. If OSA is suspected in a patient but not diagnosed, 80% (617/772) of the respondents would proceed with anesthesia with OSA precautions, 12% (94/772) would defer surgery and refer the patient to a sleep physician or respirologist, and 5% (38/772) would proceed with anesthesia without further actions. After discharge to a regular ward without telemetry, 29% (219/751) of respondents would measure vital signs every hour, 29% (215/751) every four hours, 15% (116/751) every two hours, and 7% (53/751) every eight hours. Fourteen percent (107/751) had no clear opinion.
Laparoscopic cholecystectomy scenario
Following PACU discharge of a patient with a documented history of OSA and CPAP compliance, 40% (298/743) of the respondents would send the patient home in current practice; 25% (188/739) would do the same if hospital resources were unlimited. The remainder of the respondents would keep the patient in hospital. For a patient with documented OSA and non-compliant with CPAP therapy, 82% (612/742) of the respondents would proceed with anesthesia with OSA precautions, 10% (76/742) would proceed with anesthesia without further actions, and 5% (39/742) would defer surgery and refer the patient to a sleep physician or respirologist. Following discharge from the PACU, 17% (128/739) of the respondents would send the patient home in current practice; 6% (48/739) would do the same if hospital resources were unlimited. The remainder of the respondents would keep the patient in hospital. If OSA is suspected in a patient but not diagnosed, 64% (472/741) of the respondents would proceed with anesthesia with OSA precautions, 24% (180/741) would defer surgery and refer the patient to a sleep physician or respirologist, and 10% (73/741) would proceed with anesthesia without further actions. Following discharge from the PACU, 20% (154/739) of the respondents would send the patient home in current practice; 12% (92/740) would do the same if hospital resources were unlimited. The remainder of the respondents would keep the patient in hospital.
Discussion
Despite the recommendations by the American Society of Anesthesiologists for development of institutional policies and the publication of a Canadian protocol,11,12 nearly half of the respondents either were not aware of an institutional policy to guide their perioperative management of patients with OSA or reported an absence of an institutional policy. This proportion is greater than the one reported in a previous survey of Canadian anesthesiologists in which one-quarter of the respondents followed an institutional policy.15 Nevertheless, the frequency of OSA diagnosis has increased, and the number of OSA patients seen by Canadian anesthesiologists has also increased. Indeed, about 10% of the Canadian anesthesiologists indicated that, ten years ago, they cared for six to ten patients with OSA per month. In contrast, 40% of respondents in our survey mentioned seeing such numbers of OSA patients in their practice. It is unclear whether this increase reflects an increased prevalence of OSA in the population, increased clinician awareness and diagnosis, or both. Our survey illustrated that about 50% of the respondents rely on clinical suspicion alone to identify patients who may have undiagnosed OSA preoperatively. About 30% of respondents indicated using a screening questionnaire for patients in whom OSA is clinically suspected, and 18% indicated using a questionnaire for all patients. This is concerning considering the importance of identifying the OSA patient prior to surgery so as to enable their optimal and safe perioperative care. In the recent literature, there is evidence that a diagnosis of OSA and appropriate monitoring and management may prevent postoperative adverse events.19 On the other hand, compared with the results of previous surveys of anesthesiologists from Canada and from the US, respondents seemed more prone to use a cautious approach. For example, up to 25% of the respondents preferred to defer surgery and refer the patient to a sleep physician or respirologist.15,20 The difference between these observations may be related to changes in anesthesia practice. Anesthesiologists are increasingly aware of the prevalence of OSA in the surgical population, the postoperative complications associated with OSA,21–23 and the potential treatments that may prevent such complications.3
The disposition of OSA patients to a monitored bed or ward after their stay in the PACU highlights a disparity between practices among Canadian anesthesiologists. For inpatients with OSA and compliant with CPAP, although most respondents would discharge these patients to the ward with intermittent monitoring, 15% of the respondents would discharge the patients to the ward without monitoring. These differences may be reflective of the uncertainty regarding whether the additional monitoring of patients treated with CPAP at home is associated with improved perioperative outcome and/or is cost-effective. In contrast, respondents mentioned that they would transfer CPAP non-compliant patients to a stepdown unit, and a limited number mentioned using a more conservative approach without monitoring. These observations highlight Canadian anesthesiologists’ awareness of OSA but also their concerns and a certain level of uncertainty surrounding postoperative monitoring.
The domain that has raised the most important clinical equipoise is the management of OSA patients undergoing ambulatory surgery. For patients with a documented history of OSA and compliant with CPAP therapy, we observed that more than 40% of respondents would send the patient home. In the ideal situation, 75% would favour hospital admission. Interestingly, it is a more conservative viewpoint than the approach suggested in the 2012 Society for Ambulatory Anesthesia (SAMBA) consensus statement on preoperative selection of adult patients with obstructive sleep apnea scheduled for ambulatory surgery.24
There are limitations to the results of our survey. First, although we aimed to describe current practices, a survey study is designed to evaluate opinions of respondents. Responses may thus represent what respondents think they should be doing and may not reflect their true current practices. Second, we used two different administrative databases to identify potential respondents, and thus, we may not have targeted the whole population of Canadian anesthesiologists. Third, only the web (online) questionnaire was sent in both official languages in Canada (English and French), and therefore, we may not have reached French-speaking Canadian anesthesiologists. There may have been duplicate responses as anesthesiologists may respond to the survey more than once. Lastly, there is no differentiation between mild, moderate, and severe OSA. The responses to the questionnaire may therefore have been different if we had asked respondents about the management of patients with differences in the severity of OSA.
Conclusions
We developed this survey of practicing Canadian anesthesiologists to determine the current perspectives on the perioperative management of patients with diagnosed or suspected OSA undergoing general anesthesia. Our study illustrates that the majority of anesthesiologists continue to identify OSA by relying on clinical suspicion alone, which suggests that most do not rely on systematic screening tools. Despite the accumulated evidence of the relationship between OSA and postoperative complications, it is concerning that 50% of the respondents are lacking an institutional policy. It is apparent that the preferred management strategies of anesthesiologists were constrained by hospital resources. A concerted effort to develop and implement evidence-based guidelines may be the next step to assist institutions and clinicians in the management of this “at-risk” population.
Notes
Perioperative Anesthesia Clinical Trials (PACT). Available from URL: http://canadianpact.ca/ (accessed September 2015).
References
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 2013; 177: 1006-14.
Chung F, Yegneswaran B, Liao P, et al. Validation of the Berlin questionnaire and American Society of Anesthesiologists checklist as screening tools for obstructive sleep apnea in surgical patients. Anesthesiology 2008; 108: 822-30.
Mutter TC, Chateau D, Moffatt M, Ramsey C, Roos LL, Kryger M. A matched cohort study of postoperative outcomes in obstructive sleep apnea: could preoperative diagnosis and treatment prevent complications? Anesthesiology 2014; 121: 707-18.
Singh M, Liao P, Kobah S, Wijeysundera DN, Shapiro C, Chung F. Proportion of surgical patients with undiagnosed obstructive sleep apnoea. Br J Anaesth 2013; 110: 629-36.
Finkel KJ, Searleman AC, Tymkew H, et al. Prevalence of undiagnosed obstructive sleep apnea among adult surgical patients in an academic medical center. Sleep Med 2009; 10: 753-8.
Stierer TL, Wright C, George A, Thompson RE, Wu CL, Collop N. Risk assessment of obstructive sleep apnea in a population of patients undergoing ambulatory surgery. J Clin Sleep Med 2010; 6: 467-72.
Chung F, Ward B, Ho J, Yuan H, Kayumov L, Shapiro C. Preoperative identification of sleep apnea risk in elective surgical patients, using the Berlin questionnaire. J Clin Anesth 2007; 19: 130-4.
Chung F, Yegneswaran B, Liao P, et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology 2008; 108: 812-21.
Abrishami A, Khajehdehi A, Chung F. A systematic review of screening questionnaires for obstructive sleep apnea. Can J Anesth 2010; 57: 423-38.
Ramachandran SK, Josephs LA. A meta-analysis of clinical screening tests for obstructive sleep apnea. Anesthesiology 2009; 110: 928-39.
American Society of Anesthesiologists Task Force on Perioperative. Management of Patients with Obstructive Sleep Apnea. Practice Guidelines for the perioperative management of patients with obstructive sleep apnea: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Management of Patients with Obstructive Sleep Apnea. Anesthesiology 2014; 120: 268-86.
Seet E, Chung F. Management of sleep apnea in adults—functional algorithms for the perioperative period. Can J Anesth 2010; 57: 849-64.
Adesanya AO, Lee W, Greilich NB, Joshi GP. Perioperative management of obstructive sleep apnea. Chest 2010; 138: 1489-98.
Meoli AL, Rosen CL, Kristo D, et al. Upper airway management of the adult patient with obstructive sleep apnea in the perioperative period–avoiding complications. Sleep 2003; 26: 1060-5.
Turner K, VanDenkerkhof E, Lam M, Mackillop W. Perioperative care of patients with obstructive sleep apnea - a survey of Canadian anesthesiologists. Can J Anesth 2006; 53: 299-304.
Chung S, Yuan H, Chung F. A systemic review of obstructive sleep apnea and its implications for anesthesiologists. Anesth Analg 2008; 107: 1543-63.
Burns KE, Duffett M, Kho ME, et al. A guide for the design and conduct of self-administered surveys of clinicians. CMAJ 2008; 179: 245-52.
Dillman DA. Mail and Internet Surveys: The Tailored Design Method. 2nd ed. NY: John Wiley & Sons; 2000 .
Nagappa M, Mokhlesi B, Wong J, Wong DT, Kaw R, Chung F. Effects of continuous positive airway pressure on postoperative outcomes in obstructive sleep apnea patients undergoing surgery: a systematic review and meta-analysis. Anesth Analg 2015; 120: 1013-23.
Auckley D, Cox R, Bolden N, Thornton JD. Attitudes regarding perioperative care of patients with OSA: a survey study of four specialties in the United States. Sleep Breath 2015; 19: 315-25.
Memtsoudis SG, Stundner O, Rasul R, et al. The impact of sleep apnea on postoperative utilization of resources and adverse outcomes. Anesth Analg 2014; 118: 407-18.
Mokhlesi B, Hovda MD, Vekhter B, Arora VM, Chung F, Meltzer DO. Sleep-disordered breathing and postoperative outcomes after elective surgery: analysis of the nationwide inpatient sample. Chest 2013; 144: 903-14.
Kaw R, Chung F, Pasupuleti V, Mehta J, Gay PC, Hernandez AV. Meta-analysis of the association between obstructive sleep apnoea and postoperative outcome. Br J Anaesth 2012; 109: 897-906.
Joshi GP, Ankichetty SP, Gan TJ, Chung F. Society for Ambulatory Anesthesia consensus statement on preoperative selection of adult patients with obstructive sleep apnea scheduled for ambulatory surgery. Anesth Analg 2012; 115: 1060-8.
Acknowledgements
The authors thank the residents and fellows who participated in the test-retest phase of the survey development. We also thank Yiliang Yang MD, Toronto Western Hospital, for his help in compiling the data from the postal survey and the Canadian Anesthesiologists’ Society for their assistance in contacting active members.
Conflicts of interest
None declared.
Funding
The University Health Network Foundation provided funding to Dr. Frances Chung for this survey. Dr. Alexis Turgeon is a recipient of a research career award from the Fonds de recherche du Québec - Santé (FRQS). Dr. Bryson receives support from the Ottawa Hospital Anesthesia Alternate Funds Association.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
This article is accompanied by an editorial. Please see Can J Anesth 2016; 63: this issue.
Author contributions
Ligia Cordovani and Frances Chung designed and conducted the study and collected the data. Ligia Cordovani, Frances Chung, and Peter T. Choi wrote the manuscript. Geneviève Germain, Alexis F. Turgeon, Richard Hall, Peter C. Gay, and Gregory L. Bryson assisted in the development of the protocol. Kim Turner assisted with writing the study proposal. Geneviève Germain, Alexis F. Turgeon, Richard Hall, Peter C. Gay, Gregory L. Bryson, and Kim Turner reviewed the manuscript. Peter T. Choi helped design the study and analyzed the data.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cordovani, L., Chung, F., Germain, G. et al. Perioperative management of patients with obstructive sleep apnea: a survey of Canadian anesthesiologists. Can J Anesth/J Can Anesth 63, 16–23 (2016). https://doi.org/10.1007/s12630-015-0512-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-015-0512-y