Abstract
Purpose
The ability to assess the brain-at-risk during carotid endarterectomy (CEA) under general anesthesia remains a major clinical problem. Point-of-care monitoring can potentially dictate changes to management intraoperatively. In this observational study, we examined the correlation between a series of point-of-care monitors and lactate flux during CEA.
Methods
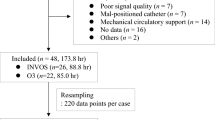
Both neurosurgeons and vascular surgeons participated in the study. The patients underwent arterial-jugular venous blood sampling for oxygen, carbon dioxide, glucose, and lactate, n = 26; bispectral index (BIS) monitoring ipsilateral to side of surgery, n = 26; raw and processed electroencephalogram (EEG), n = 22; and bi-frontal cerebral oximetry using the Fore-Sight monitor, n = 20.
Results
One patient experienced a new neurological deficit when assessed at 24 hr following surgery. Lactate flux into the brain was correlated with the greatest decrease in cerebral oximetry with carotid cross-clamping; lactate efflux was correlated with the least. The most noticeable changes in processed EEG (density spectral analysis) were also seen with lactate influx, but at a slower time resolution than cerebral oximetry. Loss of autoregulatory behaviour was demonstrated with lactate influx; however, no correlation was seen between lactate flux and BIS monitoring.
Conclusion
There was a correlation between cerebral oximetry and lactate flux during carotid cross-clamping. The Fore-Sight monitor may be of value as a point-of-care monitor during CEA under general anesthesia. A novel finding of this study is lactate flux into the brain in the presence of a large difference in cerebral oxygenation during cross-clamping of the carotid artery.
Registered at clinicaltrials.gov: NCT000737334.
Résumé
Objectif
La capacité d’évaluer le cerveau à risque pendant une endartériectomie carotidienne (EC) sous anesthésie générale demeure un problème clinique important. Le monitorage au chevet pourrait potentiellement conduire à des modifications de la prise en charge peropératoire. Dans cette étude observationnelle, nous avons exploré la corrélation entre une série de moniteurs au chevet et le flux de lactate pendant une EC.
Méthode
Des neurochirurgiens et des chirurgiens vasculaires ont pris part à cette étude. Les patients ont subi un échantillonnage du sang veineux artériel jugulaire pour détecter les concentrations d’oxygène, de dioxyde de carbone, de glucose et de lactate, n = 26; monitorage par index bispectral (BIS) ipsilatéral au côté de la chirurgie, n = 26; électroencéphalogramme (EEG) brut et après analyse, n = 22; et oxymétrie cérébrale bifrontale à l’aide du moniteur Fore-Sight, n = 20.
Résultats
Un patient a subi un nouveau déficit neurologique lorsqu’il a été évalué à 24 h après la chirurgie. Le flux entrant de lactate (vers le cerveau) a été corrélé à la réduction maximum de l’oxymétrie cérébrale lors du clampage carotidien; le flux sortant de lactate a été corrélé à la réduction minimum. Les changements les plus remarquables à l’EEG après analyse (analyse de la densité spectrale) ont également été observés avec un débit entrant de lactate, mais à une résolution temporelle plus lente que l’oxymétrie cérébrale. La perte d’autorégulation a été démontrée lors d’un flux entrant de lactate; toutefois, aucune corrélation n’a été observée entre le flux de lactate et le monitorage par BIS.
Conclusion
Une corrélation a été observée entre l’oxymétrie cérébrale et le flux de lactate pendant le clampage carotidien. Le moniteur Fore-Sight pourrait être utile comme moniteur au chevet pendant les EC sous anesthésie générale. Une autre découverte innovante de cette étude est le flux entrant de lactate vers le cerveau en présence d’une différence importante d’oxygénation cérébrale pendant le clampage de la carotide.
Enregistré à clinicaltrials.gov: NCT000737334.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Optimal anesthetic management to prevent cerebral injury during carotid endarterectomy (CEA) remains a challenge.1 The challenge is perhaps most trying for the patient who undergoes the procedure with general anesthesia.2 In this context, a monitor that could warn the anesthesiologist in real-time of the potential for ipsilateral cerebral injury during the period of cross-clamping of the carotid artery would be of considerable value to enhance the safety of this procedure. Advocates of regional anesthesia for CEA already have such a monitor – the awake patient – to permit real-time assessment of level of consciousness and the appearance of dysarthria or hemiparesis.3 Clearly, such assessments are not possible with induction of general anesthesia.
To initiate rational intervention strategies in a timely manner, point-of-care monitoring is essential during carotid endarterectomy under general anesthesia. The monitors that are readily available include raw and processed electroencephalogram (EEG) analysis,4 somatosensory evoked potentials (SSEPs),5 Doppler flowmetry,6 cerebral oximetry,7 cerebral blood flow,4,8 and assessment of measureable arterial to jugular venous differences (e.g., partial pressure of oxygen, carbon dioxide, glucose, lactate, and derived indices such as oxygen content).9 Jugular venous blood sampling is a simple intervention during carotid endarterectomy, as the jugular vein is in the surgical field and direct retrograde cannulation is easily feasible. Recent work examining arterial-jugular venous sampling in patients undergoing awake CEA revealed that arterial-venous lactate difference was the most sensitive index of cerebral ischemia.10 This finding correlated with new ischemia (confusion, hemiparesis, or dysarthria) with cross-clamping in patients under regional anesthesia. If applicable under general anesthesia, lactate flux could suggest brain-at-risk and guide therapeutic intervention when patients are unable to serve as their own monitors of cerebral wellbeing. A robust surrogate to lactate flux using other available non-invasive point-of-care monitors during general anesthesia would be advantageous to avoid jugular venous cannulation. However, there is an anticipated low risk of jugular venous cannulation under direct vision. Point-of-care measurement of arterial-venous lactate flux can be obtained with properly configured blood gas machines available in many operating room settings. Other arterial-venous concentration differences have been shown to be more sensitive than lactate difference (adenosine and hypoxantine), however, not as a point-of-care measurement.11
Alterations in cerebral oximetry with carotid cross-clamping would appear to be a promising monitoring approach. However, studies have been both positive and negative regarding the value of cerebral oximetry to aid management during CEA (see reviews).12,13A newer cerebral oximeter – the Fore-Sight monitor is now commercially available. This monitor is deemed to be superior to devices previously available and claims to be an absolute measure of cerebral oxygenation.14 Using four tuned lasers (in the near infrared range), it interrogates the frontal cortex to determine the saturation of cortical tissue (SctO2).
In this study, we examined patients undergoing CEA with general anesthesia and undertook point-of-care arterial-jugular venous blood sampling correlated with processed EEG analysis, including bispectral index (BIS), EEGo15 and density spectral analysis (DSA), and cerebral oximetry using the Fore-Sight oximeter (CASMed Medical Systems, Branford, CT, USA). It was our objective to determine if one monitor was best correlated with lactate flux across the brain to serve as its surrogate during CEA under general anesthesia.
Methods
The Biomedical Research Ethics Board at the University of Manitoba approved this study. All patients scheduled for elective CEA were approached in the Pre-Anesthetic Clinic at the Health Sciences Centre in Winnipeg, Manitoba. Exclusion criteria included failure to understand the presented protocol, a history of asthma requiring bronchodilators (because the study protocol used desflurane as the volatile agent), pregnancy, non-elective carotid endarterectomy, and patient refusal. A total of 38 patients were approached in the Pre-Anesthetic Clinic. Three patients refused participation. The remaining 35 patients provided witnessed informed consent.
Operating room preparation
On presentation to the operating room on the day of surgery, those patients who remained in agreement with participation were enrolled in the study. Routine monitoring was placed, including five-lead electrocardiogram, non-invasive blood pressure sphygmomanometry, and pulse oximetry. Midazolam 1 mg iv was administered prior to placement of a 20-gauge radial artery cannula inserted on the side opposite to the operative site. A BIS monitor strip (Aspect Medical Systems, Newton, MA, USA) was placed on the patient’s forehead per manufacturer’s instructions ipslilateral to the site of the proposed surgery. Forehead sensors were placed bilaterally in patients monitored with the Fore-Sight cerebral oximeter and then covered with the provided black plastic shroud to block ambient light. The attending anesthesiologist was informed of the normal values expected for the Fore-Sight monitor output, i.e., an SctO2 of 60-80%. Following pre-oxygenation, the patient had anesthesia induced with a 1 μg·kg−1 bolus of remifentanil, propofol 1.0-2.0 mg·kg−1, and rocuronium 0.6-1 mg·kg−1 for muscle relaxation to facilitate intubation of the trachea. Following intubation, the patients were placed on an inspired oxygen concentration of 50% in air, and desflurane was administered to an end-tidal concentration resulting in a BIS value of 40-60 arbitrary BIS units. Remifentanil was infused at 0.03-0.1 μg·kg−1·min−1 during the procedure. The mean arterial pressure (MAP) was increased, if deemed appropriate, by bolus administration of phenylephrine 100 μg or, if needed, infusion at 0.1-0.5 μg·kg−1·min−1. Needle electrodes were placed using the international 10:20 system over the frontal region bilaterally to enable bipolar EEG recordings of both frontal cortices.15 These signals were processed to provide an EEGo output as previously described.16 If patients were treated by a neurosurgeon, they underwent raw EEG, DSA, and SSEP monitoring per standard procedure by a neurophysiologist.
Data collection
Data streams of selected output from the Philips Intellivue monitor (Philips Healthcare, Andover, MA, USA) were downloaded in real-time to a laptop computer running Trendface Solo software (iXellence GmBH, Wildau, Germany), permitting data dumps with resolution of one Hertz. The EEGo processed EEG signal was downloaded to a second laptop running specific software. For patients monitored with the Fore-Sight oximeter, data were stored internally on the device at a resolution of 0.5 Hertz. These data were downloaded to an Intellistick™ at the end of the experiment. All data streams from the various monitoring devices were sequenced for date and time at the start of the experiment by sequencing the clocks of the intraoperative monitors and laptop computers to the second.
Surgical procedure and blood gas measurements
Both neurosurgeons and vascular surgeons participated in the study. None of the surgeons used a shunt intraoperatively. Upon exposure of the carotid sheath, the jugular vein was dissected free and cannulated with a 16-gauge intravenous catheter in a retrograde fashion. A multi-ported Portex epidural catheter was threaded into the jugular vein under direct vision, advanced in a cephalad direction until resistance was met, withdrawn slightly, then fixed in place with a purse-string suture. The epidural catheter was attached to sterile arterial pressure tubing, and the distal end was handed off to the anesthesiologist who verified that unobstructed blood withdrawal could be obtained. A baseline sample of jugular venous blood was withdrawn after placement of the cannula. When the dead space of the tubing was full, a further 5 mL of blood was withdrawn before the jugular venous sample was taken. Blood withdrawal occurred over a one-minute period. A simultaneous arterial sample was obtained from the radial artery cannula. To ensure matched samples at each withdrawal period, the measured hemoglobin of each sample had to correspond within 4 g·L−1. All blood samples were drawn into pre-labelled blood gas syringes that contained lyophilized lithium heparin. Upon withdrawal, the samples were placed immediately on crushed ice prior to measurement in a Radiometer ABL 800 blood gas machine that was calibrated at the start of each day. At three minutes prior to carotid cross-clamping, 5,000 international units of heparin was administered to the patient. The timing of cross-clamp application was noted. Simultaneous arterial and jugular venous blood sampling was obtained at two minutes and ten minutes after carotid cross-clamping, two minutes prior to cross-clamp release, and then two and five minutes after cross-clamp release. The time of cross-clamp release was noted. The jugular venous cannula was removed, and the purse string suture was cinched and tied. During the conduct of the procedure, the simultaneous blood gases were analyzed immediately after withdrawal, and results were made available to the attending anesthesiologist. Alterations in patient management were at the discretion of the attending anesthesiologist, with customary management being an increase in MAP co-incident with cross-clamp application, increase in FIO2 in some cases, and more rarely, small alterations in end-tidal carbon dioxide tension by decreasing minute ventilation.
Hemodynamics, anesthetic agent, BIS output, and ventilator variables were collected to the laptop computer at selected time periods: pre-induction, stable post-induction, pre-cross-clamp, two and ten minutes after cross-clamp, pre-reperfusion, cross-clamp released for two and five minutes, anesthetic vapour off, emergence (remifentanil off), and with extubation.
Post-hoc arterial-jugular venous blood gas differences were examined in oxygen saturation, glucose, and lactate concentration. Lactate differences were normalized based on arterial concentration, i.e., an index was reported based on arterial-jugular venous concentration/arterial concentration. The hyperglycolytic index17 was determined by calculation of Δarterial-jugular venous O2 content (mmoL·L−1)/Δ arterial-jugular venous glucose concentration (mmoL·L−1).
Statistical analysis
Tests to compare various parameters over time entailed repeated measures analysis of variance for continuous data. Bonferroni’s correction was applied for multiple comparisons within groups following examination of least squares means test matrices. Regression correlations were examined between normalized lactate flux and changes in oximetry output with onset and offset of cross-clamping and changes in processed EEG with BIS, EEGo, and DSA. Primary outcomes were considered statistically significant if the P value was ≤ 0.05. Secondary outcomes were considered significant at P ≤ 0.025.
A comparison of the incidence of hyperglycolysis between the lactate flux states was undertaken by Chi square analysis using a 2 × 3 contingency table with P < 0.025 considered significant.
Results
Thirty-five patients were enrolled in the study from September 17, 2008 to April 21, 2010. We report our findings from 26 patients. In seven patients, difficulties were encountered with consistent sampling of jugular venous blood (seen in the first five patients and sporadically thereafter). One patient was found to have an occluded carotid on examination, so the vessel was tied off. In one case, the study was terminated because we could not place the oximeter sensors over both frontal cortices due to the small surface area available on this patient’s forehead. Data from these nine patients are not reported. We obtained BIS recordings from all 26 of the patients reported; EEGo recordings from 22; intraoperative monitoring by a neurophysiologist from 16; and cerebral oximetry from 20 patients.
Overall demographics
Table 1 indicates the demographics for the 26 patients reported. One patient had a neurologic deficit (left upper limb paresis) that waxed and waned for more than 24 hr. Ultimately, the patient stabilized with no new deficit. This patient demonstrated lactate influx on four occasions intraoperatively. Postoperatively, there was evidence that the patient suffered a non-ST-segment elevation myocardial infarction.
Hemodynamics, arterial – jugular venous differences, and respiratory data
Table 2 shows a series of intraoperative parameters recorded during the conduct of the experiment. Mean arterial blood pressure was increased approximately 10-15 mmHg by the time the cross-clamp was applied until cross-clamp release. End-tidal desflurane concentration was essentially stable during the period of cross-clamping and markedly decreased at end-experiment, as planned, prior to extubation. Arterial PCO2 was stable over the course of cross-clamping. Glucose flux increased with cross-clamping, more than doubling by ten minutes of clamp application from baseline, and it elevated persistently up to the period of cross-clamp release at two minutes. Alterations in arterial–jugular venous PCO2 were stable during clamping. The fraction of inspired O2 did not differ over any time period.
Lactate flux during surgical procedure
The pattern of lactate flux over the course of the surgical procedure is shown in Fig. 1. Some patients demonstrated all three patterns at some time during the procedure – no net flux, a lactate influx into the brain, and a net efflux from the brain.
Percent of total for the three different lactate flux states for the various measurement periods in the experiment (n = 26). Open diamond designates no lactate flux; solid triangle designates positive lactate flux (influx into the brain), and the solid square designates negative lactate flux (efflux from the brain). The time periods are as follows: T2 – immediately before carotid cross-clamping; T3 – two minutes after clamp application; T4 – ten minutes after clamp application; T5 – immediately prior to cross-clamp removal; T6 – two minutes after cross-clamp release; T7 – five minutes after cross-clamp release
Correlations of other point-of-care monitors to lactate flux during surgical procedure
Table 3 gives a brief overview of the behaviour of each point-of-care monitor correlated with alterations in lactate flux. A fuller description of the behaviour of each monitor in relation to lactate flux is highlighted below.
Cerebral oximetry during CEA and lactate flux
A correlation was seen between cross-clamping and the ipsilateral magnitude of change in SctO2 with lactate flux (Fig. 2). Patients that manifested with net lactate influx, especially during the period of cross-clamping (times 3-5 in the figure), had the greatest net decrease in SctO2 with cross-clamping. Patients with net lactate efflux demonstrated the smallest decrease in SctO2. An inverse linear relationship (R2 = 0.423 with P = 0.003) between net lactate flux (normalized to individual arterial lactate concentration) is shown in Fig. 2 over the time periods immediately before carotid cross-clamping to two minutes after cross-clamp application. In nearly all cases following cross-clamping, there was a very rapid change in SctO2 in the ipsilateral hemisphere, usually manifesting within seconds. Rapid changes were also seen with cross-clamp release (see Fig. 3A for a reconstruction of the anesthetic course during one study where lactate influx occurred during the period of cross-clamping). Fig. 4A-D shows the time course of alterations in SctO2 between hemispheres in one study with lactate influx. Prior to cross-clamping, there was no correlation between SctO2 and MAP. With cross-clamping, autoregulation was lost with a negative correlation between SctO2 and MAP. Restoration of autoregulation occurred with cross-clamp removal and resolution of lactate influx. The correlation between SctO2 and jugular venous oxygen saturation (SjvO2) is shown in Fig. 5. Of interest is the very close correlation with SctO2 less than SjvO2 in this clinical situation. Fig. 6 shows the decreased ratio of arterial-jugular venous O2 utilization to arterial-jugular venous glucose utilization (termed the hyperglycolytic index if the ratio is < 3.44).17
Relationship between percentage change in ipsilateral cerebral oxygen saturation from T2 to T3 (immediately before cross-clamping and two minutes after cross-clamp application) vs change in normalized lactate flux ([arterial – jugular venous lactate]/[arterial lactate]; for T2-T3). Thus, increased lactate influx over this time period is negative in this context. A strong inverse correlation was seen for increasing the difference in saturation of cortical tissue between hemispheres manifesting with a large negative lactate flux
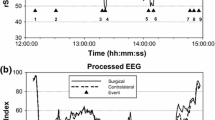
A - D In the analysis of monitoring modalities, one patient demonstrated multiple episodes of lactate influx during the course of the study. A - shows the mean difference in saturation of cortical tissue (SctO2) between hemispheres over the period of cross-clamping. A very prompt decrease in SctO2 is seen with clamp application in the ipsilateral hemisphere, and the converse is seen with clamp release. The lactate flux (in mmoL·L−1) is listed at the bottom for each of the time periods – a positive number represents lactate influx and a negative number indicates lactate efflux. B - shows the electroencephalogram (EEG) processed by density spectral analysis using fast Fourier transform. There is marked attenuation of α-wave activity (output in region of 8 - 12 cycles·sec−1) in the temporal and frontal regions. If coloured purple, the power was 0 pico-Watts. The decreased α-wave activity correlated with the time the carotid cross-clamp was applied, defined between the red hash marks on the left axis. This processed EEG output corresponded with a difference in SctO2 of > 18% between hemispheres. C - shows the bispectral index (BIS) output in arbitrary units. Over the period of cross-clamp application there is little noticeable change in BIS output. Above is the end-tidal desflurane concentration demonstrating its stability over this time period. D – the change in EEGo output (another processed EEG signal using three-dimensional time delay plots to show changes in EEG output graphically) shows attenuation of signal with momentary burst suppression at T5. Quantitation of this signal is not readily possible with this device
A-D: A - shows the time course of saturation of cortical tissue (SctO2) and mean arterial pressure (MAP) for one patient with lactate influx. B - at four minutes preceding clamp application with a mean difference in SctO2 signal of 3% between hemispheres, there was no correlation between SctO2 and alteration in MAP. C - at one minute following cross-clamp application, the difference in SctO2 between hemispheres is > 12%. At this time, there is an inverse relationship in the difference between MAP and SctO2, suggesting loss of metabolic autoregulation. At this time, the hemisphere was demonstrating lactate influx into the brain. D - at one minute following cross-clamp release, with a mean difference in SctO2 of 4.0% between hemispheres, again there was no relationship between MAP and SctO2, suggesting restored autoregulation
(and inset) Time course of saturation of cortical tissue (SctO2) and jugular venous oxygen saturation (SjvO2) for the previously described time points for the study (each time point comprises 18-20 measurements). The close relationship between the two measurements is evident. The linear correlation is shown in the inset with R2 = 0.870; P = 0.007; with y = 1.07 x −11.5. Thus, there was an offset of 11.5%, with SjvO2 being greater than SctO2. See text for further discussion
The relationship between the ratio of the difference in arterial-jugular venous O2 content to the difference in arterial-jugular venous glucose concentration vs normalized lactate flux. A negative flux is defined as lactate efflux; no net flux is on the y-axis, and a positive flux is defined as lactate influx into the brain. Above the figure is a contingency table of the incidence of each flux state for values for the ΔO2 content to Δglucose ratio of < 3.44 (defined as hyperglycolysis).17
Density spectral analysis during CEA and lactate flux
When carotid cross-clamping was associated with evidence of more than a single demonstration of lactate influx with carotid cross-clamping, diminution of high frequency EEG signals could be demonstrated (see Fig. 3B for such a patient). Little evidence of diminished EEG high frequency power was seen with no net flux or efflux of lactate. Density spectral analysis alterations were seen over a longer time frame for onset than for oximetry (in the range of minutes rather than seconds).
BIS output during CEA and lacate flux
There was no discernable relationship between the BIS output and changes in lactate flux during the procedure. No significant change in BIS output was seen over the conduct of the procedure as demonstrated in Fig. 3C. As the BIS is designed specifically to demonstrate changes in depth of anesthesia, the concurrent end-tidal concentrations are shown in this figure as well.
EEGo during CEA and lactate flux
The EEGo is another form of processed EEG with a three-dimensional time delay plot of the EEG signal; results were published previously in the Journal.15 The same patient as seen for DSA output from above is shown in Fig. 3D. There is evidence of greater simplicity of the three-dimensional plot indicating less complexity of the EEG signal. It is difficult to quantify this change, however, and it required a dedicated observer to make such alterations known.
Discussion
This study represents a single-arm prospective cohort study comparing a number of point-of-care intraoperative monitors with observed lactate flux, as measured by arterial to jugular venous concentration differences perioperatively during carotid endarterectomy under general anesthesia.
An influx of lactate into the brain under general anesthesia is a novel observation of our study. Review of the available literature documents the efflux of lactate with CEA or during cerebral injury as being potentially important to indicate brain-at-risk – but not the converse.9,17-19 Our findings are controversial, but new work strongly suggests that lactate may well be the preferred substrate for cerebral metabolism both anerobically and aerobically.20-23 Thus, in the face of diminished oxygen supply, as with carotid cross-clamping in patients at risk, influx of lactate may be critically important to serve as a fuel for cerebral metabolism. Our study suggests that such may be the case.
Lactate influx into the brain has definitively been shown in a number of situations. A growing body of work demonstrates that during physical stress (marked exercise load) the brain shows lactate influx.24 Other clear-cut episodes occur with severe traumatic brain injury,25 cerebral vasospasm,19 and during resuscitation following cardiac arrest.26 It would thus appear that the brain will use lactate as a fuel when stressed. In our study, the single patient with a new postoperative deficit had episodes of measured lactate influx (0.2 mmoL·L−1) during the operative course.
In patients following subarachnoid hemorrhage, a decreased ratio of oxygen utilization to glucose utilization has been demonstrated with poor outcome. Oertel et al.17 showed that there was nearly a 50% mortality rate if this ratio was < 3.44 (termed hyperglycolysis). Fig. 6 shows the incidence of hyperglycolysis in the three different lactate flux states during the periods of cross-clamping and two minutes following clamp release. A hyperglycolytic state was seen with lactate influx over 60% of the time, suggesting the brain was under metabolic stress.
This study has demonstrated that the measurement of lactate flux is not difficult. The internal jugular venous catheter is placed retrograde under direct vision by the surgeon (with no complications in our cohort). The venous withdrawal, correlated with simultaneous arterial sampling, can be measured readily if a lactate sensor module is available on the operating room blood gas machine. Our work suggests that lactate influx during cross-clamping may be most indicative of cortical ischemia under general anesthesia and could suggest intraoperative interventions to diminish the influx. This study indicates that large changes in SctO2 following cross-clamping may provide a surrogate for lactate influx following clamping. Our findings, Fig. 5, are in the same range for the Δ between SctO2 and SjvO2 (−5 to −10% during cardiac catheterization or cardiopulmonary bypass when SjvO2 was in the range of 70-80%).27 In the context of CEA, it may be of greater importance to note the difference from baseline following cross-clamping to track brain-at-risk. In addition, the impact of alterations in MAP could be tracked in real-time by the Fore-Sight monitor to diminish favourably the decreases in SctO2 seen with cross-clamping (see Fig. 4).
The ideal point-of-care monitor specific to anesthesia can accurately predict when an organ is at risk during an operative procedure so that a therapeutic intervention can be initiated to prevent further or permanent damage to that organ. To date, no such monitor exists for the brain in the context of CEA conducted under general anesthesia. Since a monitor with this description does not exist, many practitioners have advocated regional anesthesia for CEA so that the awake patient can be assessed in real-time for changes in cognition or contralateral deterioration in cerebral function (paresthesias or hemiparesis with cross-clamp application). The general anesthesia vs local anesthesia for carotid surgery (GALA) trial indicates that there is no advantage of regional anesthesia over general anesthesia for CEA.2 A potential outcome of the GALA trial is that general anesthesia could be made safer with improved point-of-care monitoring. Moritz et al. have studied the transferability of neuromonitoring from the awake patient to patients under sevoflurane/fentanyl anesthesia, and they found good concordance for stump pressure and similar relative changes with cross-clamping for transcranial Doppler sonography, cerebral oximetry, and SSEPs.28
Another recent study by Moritz et al. 10 suggested that an arterial-jugular venous lactate concentration efflux was a particularly sensitive marker of cerebral dysfunction during awake CEA. Unfortunately, the transferability of arterial-jugular venous lactate to management under general anesthesia was not assessed.28 We have extended these observations to management of CEA under general anesthesia. Importantly, alterations in SctO2 would appear to be a surrogate for lactate flux in this context, suggesting that this point-of-care monitor may aid management during CEA under general anesthesia.
Processed EEG, either by EEGo or BIS, were not quantitative enough or sensitive enough, respectively, to indicate patients at risk. The BIS output did not correlate with lactate flux or demonstrate an appreciable signal with sizeable changes in SctO2 signal. The EEGo, a three-dimensional time-delayed processed EEG signal with a rapid response time (50 msec), appeared, on occasion, to indicate changes, such as increased bursts of isoelectricity with cross-clamping of the carotid artery, but the changes were not in an easily quantifiable manner.15 A post-hoc inspection of raw EEG data using density spectral analysis showed loss of α-wave activity that correlated with lactate influx (Fig. 3B). Such a processed EEG signal can be point-of-care in configured intraoperative monitor consoles.
We believe an important observation in this study is documentation of both positive and negative flux in lactate with CEA. Our data suggest correlations between lactate influx and the brain-at-risk under general anesthesia. A more comprehensive study is warranted to document this relationship in the context of CEA with multiple blood sampling periods during and after cross-clamping. In Fig. 6, the incidence of hyperglycolysis was 61.5% with lactate influx, 30% with lactate efflux, and only 12.5% with no net flux. Transition from one state to the other was demonstrated in a number of patients (see Fig. 4A for an example) suggesting a dynamic metabolic stress during the procedure.
The review by Murkin and Arango12 suggests that a > 12% decrease in cerebral saturation is “a reliable, sensitive, and relatively specific threshold for brain ischemia secondary to internal carotid artery clamping”. Our work suggests that the Fore-Sight cerebral oximeter may provide very early notification of intraoperative cerebral compromise as assessed by a large SctO2 difference following cross-clamping of the carotid artery. As a point-of-care monitor, it correlated well with lactate flux – indicating the brain under stress. Furthermore, in some patients, decreased α-wave EEG activity co-incident with carotid clamping correlated with a large SctO2 difference (Fig. 3A and B). Our study also suggests that conventional anesthesia management during CEA (increase in MAP during cross-clamping) correlated with an increase in ipsilateral cerebral oxygen saturation. The output of the Fore-Sight monitor appears to confirm the merits of this management approach (Fig. 4).
A fundamental question is whether the Fore-Sight monitor used to assess cerebral oxygenation during CEA is cost-effective. A multicentre study would be needed to provide a definitive indication as to the advantage of such monitoring. By way of example, it would require nearly 2,500 patients to be stratified into two groups (half with monitoring and half without) to assess if cerebral oximetry could reduce the acute stroke rate to 50% of baseline, based on a one-sided significance test (an α-value of 0.05; a β of 20%; and a reduction of stroke rate from 3 to 1.5%). It remains to be seen if the advantages of potentially improved patient outcome will outweigh the costs of using cerebral oximeters, such as the Fore-Sight monitor, in this operative setting.
Finally, consideration should be given to monitoring arterial to jugular venous differences in lactate concentration during CEA. Placement of a jugular venous catheter is easy and takes little time. If point-of-care blood gas monitoring of lactate concentration is available, lactate influx may indicate that the brain is at risk during this procedure under general anesthesia.
References
Guay J. The GALA trial: answers it gives, answers it does not. Lancet 2008; 372: 2092-3.
GALA Trial Collaborative Group, Lewis SC, Warlow CP, et al. General anaesthesia versus local anaesthesia for carotid surgery (GALA): a multicentre, randomised controlled trial. Lancet 2008; 372: 2132-42.
Weber CF, Friedl H, Hueppe M, et al. Impact of general versus local anesthesia on early postoperative cognitive dysfunction following carotid endarterectomy: GALA Study Subgroup Analysis. World J Surg 2009; 33: 1526-32.
Messick JM Jr, Casement B, Sharbrough FW, Milde LN, Michenfelder JD, Sundt TM Jr. Correlation of regional cerebral blood flow (rCBF) with EEG changes during isoflurane anesthesia for carotid endarterectomy: critical rCBF. Anesthesiology 1987; 66: 344-9.
Astarci P, Guerit JM, Robert A, et al. Stump pressure and somatosensory evoked potentials for predicting the use of shunt during carotid surgery. Ann Vasc Surg 2007; 21: 312-7.
Winkler GA, Calligaro KD, Kolakowski S, et al. Comparison of intraoperative completion flowmeter versus duplex ultrasonography and contrast arteriography for carotid endarterectomy. Vasc Endovascular Surg 2006; 40: 482-6.
Pugliese F, Ruberto F, Tosi A, et al. Regional cerebral saturation versus transcranial Doppler during carotid endarterectomy under regional anaesthesia. Eur J Anaesthesiol 2009; 26: 643-7.
Waltz AG, Sundt TM Jr, Michenfelder JD. Cerebral blood flow during carotid endarterectomy. Circulation 1972; 45: 1091-6.
Wassman H, Fromm G, Nadstawek J, Bannister C, Hartmann A, Pavlidis C. The influence of barbiturates on cerebral metabolism in patients with borderline cerebrovascular reserve during intraoperative transient carotid occlusion. Br J Neurosurg 1989; 3: 429-34.
Moritz S, Kasprzak P, Woertgen C, Taeger K, Metz C. The accuracy of jugular bulb venous monitoring in detecting cerebral ischemia in awake patients undergoing carotid endarterectomy. J Neurosurg Anesthesiol 2008; 20: 8-14.
Weigand MA, Michel A, Eckstein HH, Martin E, Bardenheuer HJ. Adenosine: a sensitive indicator of cerebral ischemia during carotid endarterectomy. Anesthesiology 1999; 91: 414-21.
Murkin JM, Arango M. Near-infrared spectroscopy as an index of brain and tissue oxygenation. Br J Anaesth 2009; 103(Suppl 1): i3-13.
Pennekamp CW, Bots ML, Kappelle LJ, et al. The value of near-infrared spectroscopy measured cerebral oximetry during carotid endarterectomy in perioperative stroke prevention. A review. Eur J Vasc Endovasc Surg 2009; 38: 539-45.
Hemmerling TM, Bluteau MC, Kazan R, Bracco D. Significant decrease of cerebral oxygen saturation during single-lung ventilation measured using absolute oximetry. Br J Anaesth 2008; 101: 870-5.
Pauls RJ, Dickson TJ, Kaufmann AM, et al. A comparison of the ability of the EEGo and BIS monitors to assess emergence following neurosurgery. Can J Anesth 2009; 56: 366-73.
Walling PT, Hicks KN. Nonlinear changes in brain dynamics during emergence from sevoflurane anesthesia: preliminary exploration using new software. Anesthesiology 2006; 105: 927-35.
Oertel MF, Schwedler M, Stein M, et al. Cerebral energy failure after subarachnoid hemorrhage: the role of relative hyperglycolysis. J Clin Neurosci 2007; 14: 948-54.
Robertson CS, Narayan RK, Gokaslan ZL, et al. Cerebral arteriovenous oxygen difference as an estimate of cerebral blood flow in comatose patients. J Neurosurg 1989; 70: 222-30.
Artru F, Dailler F, Burel E, et al. Assessment of jugular blood oxygen and lactate indices for detection of cerebral ischemia and prognosis. J Neurosurg Anesthesiol 2004; 16: 226-31.
Schurr A. Lactate: the ultimate cerebral oxidative energy substrate? J Cereb Blood Flow Metab 2006; 26: 142-52.
van Hall G, Stromstad M, Rasmussen P, et al. Blood lactate is an important energy source for the human brain. J Cereb Blood Flow Metab 2009; 29: 1121-9.
Berthet C, Lei H, Thevenet J, Gruetter R, Magistretti PJ, Hirt L. Neuroprotective role of lactate after cerebral ischemia. J Cereb Blood Flow Metab 2009; 29: 1780-9.
Cater HL, Chandratheva A, Benham CD, Morrison B 3rd, Sundstrom LE. Lactate and glucose as energy substrates during, and after, oxygen deprivation in rat hippocampal acute and cultured slices. J Neurochem 2003; 87: 1381-90.
van Hall G. Lactate kinetics in human tissues at rest and during exercise. Acta Physiol 2010; DOI: 10.1111/j.1748-1716.2010.02122.x.
Holbein M, Bechir M, Ludwig S, et al. Differential influence of arterial blood glucose on cerebral metabolism following severe traumatic brain injury. Crit Care 2009; 13: R13.
Rivers EP, Paradis NA, Martin GB, et al. Cerebral lactate uptake during cardiopulmonary resuscitation in humans. J Cereb Blood Flow Metab 1991; 11: 479-84.
Daubeney PE, Pilkington SN, Janke E, Charlton GA, Smith DC, Webber SA. Cerebral oxygenation measured by near-infrared spectroscopy: comparison with jugular bulb oximetry. Ann Thorac Surg 1996; 61: 930-4.
Moritz S, Schmidt C, Bucher M, et al. Neuromonitoring in carotid surgery: are the results obtained in awake patients transferable to patients under sevoflurane/fentanyl anesthesia? J Neurosurg Anesthesiol 2010.
Funding
Academic Oversight Committee, Department of Anesthesia, University of Manitoba.
Conflict of interest
Dr. Mutch was provided the CASMed Fore-Sight Cerebral Oximeter to use in this study. The sensors for the monitor were purchased at 50% of market value. CASMed had no input into the design, interpretation, or writing of this paper. No other author has a conflict to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Espenell, A.E.G., McIntyre, I.W., Gulati, H. et al. Lactate flux during carotid endarterectomy under general anesthesia: correlation with various point-of-care monitors. Can J Anesth/J Can Anesth 57, 903–912 (2010). https://doi.org/10.1007/s12630-010-9356-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-010-9356-7