Abstract
Sarcopenia and frailty are highly prevalent conditions in older hospitalized patients, which are associated with a myriad of adverse clinical outcomes. This paper, prepared by a multidisciplinary expert working group from the Australian and New Zealand Society for Sarcopenia and Frailty Research (ANZSSFR), provides an up-to-date overview of current evidence and recommendations based on a narrative review of the literature for the screening, diagnosis, and management of sarcopenia and frailty in older patients within the hospital setting. It also includes suggestions on potential pathways to implement change to encourage widespread adoption of these evidence-informed recommendations within hospital settings. The expert working group concluded there was insufficient evidence to support any specific screening tool for sarcopenia and recommends an assessment of probable sarcopenia/sarcopenia using established criteria for all older (≥65 years) hospitalized patients or in younger patients with conditions (e.g., comorbidities) that may increase their risk of sarcopenia. Diagnosis of probable sarcopenia should be based on an assessment of low muscle strength (grip strength or five times sit-to-stand) with sarcopenia diagnosis including low muscle mass quantified from dual energy X-ray absorptiometry, bioelectrical impedance analysis or in the absence of diagnostic devices, calf circumference as a proxy measure. Severe sarcopenia is represented by the addition of impaired physical performance (slow gait speed). All patients with probable sarcopenia or sarcopenia should be investigated for causes (e.g., chronic/acute disease or malnutrition), and treated accordingly. For frailty, it is recommended that all hospitalized patients aged 70 years and older be screened using a validated tool [Clinical Frailty Scale (CFS), Hospital Frailty Risk Score, the FRAIL scale or the Frailty Index]. Patients screened as positive for frailty should undergo further clinical assessment using the Frailty Phenotype, Frailty Index or information collected from a Comprehensive Geriatric Assessment (CGA). All patients identified as frail should receive follow up by a health practitioner(s) for an individualized care plan. To treat older hospitalized patients with probable sarcopenia, sarcopenia, or frailty, it is recommended that a structured and supervised multi-component exercise program incorporating elements of resistance (muscle strengthening), challenging balance, and functional mobility training be prescribed as early as possible combined with nutritional support to optimize energy and protein intake and correct any deficiencies. There is insufficient evidence to recommend pharmacological agents for the treatment of sarcopenia or frailty. Finally, to facilitate integration of these recommendations into hospital settings organization-wide approaches are needed, with the Spread and Sustain framework recommended to facilitate organizational culture change, with the help of ‘champions’ to drive these changes. A multidisciplinary team approach incorporating awareness and education initiatives for healthcare professionals is recommended to ensure that screening, diagnosis and management approaches for sarcopenia and frailty are embedded and sustained within hospital settings. Finally, patients and caregivers’ education should be integrated into the care pathway to facilitate adherence to prescribed management approaches for sarcopenia and frailty.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hospitalization rates are highest in older adults, with those aged >65 years accounting for 42% of hospitalizations and 48% of patient days (1, 2). Amongst these hospitalized older adults, the prevalence of sarcopenia and frailty has been reported to be 37% and 47%, respectively (3). Both sarcopenia and frailty are associated with longer hospital stays (4, 5), readmissions (6, 7), institutionalization (8–10), lower quality of life (QoL) (11) and higher mortality (6). Sarcopenia and frailty often co-occur with malnutrition, which has been reported in 66% of older inpatients (3). The risk of malnutrition is 4.1-fold higher if a patient has sarcopenia and 5.8-fold higher if a patient is frail (3). Moreover, older adults with two or more conditions of either sarcopenia, frailty, or malnutrition are more likely to be hospitalized, and are disproportionally represented in hospitals (3). The high prevalence of sarcopenia and frailty, with or without malnutrition, and their implications for adverse clinical outcomes in hospitalized older adults highlights the need for routine screening and/or assessment and subsequent management of these conditions during hospitalization using best practice, evidence-based approaches. However, there are currently no evidence-informed recommendations based on the available literature related to the screening, assessment and management of both sarcopenia and frailty in older adults within hospital settings. Therefore, the purpose of this paper, prepared by a multidisciplinary expert working group on sarcopenia and frailty from the Australian and New Zealand Society for Sarcopenia and Frailty Research (ANZSSFR), is to provide an up-to-date overview for clinicians and healthcare professionals on the current evidence and provide recommendations for the screening, assessment, and management of sarcopenia and frailty within the hospital setting. It also highlights barriers and potential pathways to implement change to encourage widespread adoption of these evidence-informed recommendations related to sarcopenia and frailty within hospital settings.
Methods
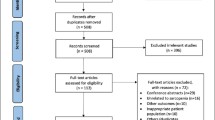
This manuscript was prepared by a group of 15 clinicians and researchers with expertise in geriatrics, gerontology, dietetics, exercise physiology, occupational therapy, and intensive care. In September 2020, expressions of interest were sought from Australian-based experts within the fields of sarcopenia, frailty and malnutrition to join an ANZSSFR working group to develop recommendations on the screening, diagnosis and management of sarcopenia and frailty for older adults within hospital settings. Those that registered an interest were asked to provide written feedback via email on the proposed aims and structure of the manuscript developed by authors RMD and SI. This was followed by ongoing dialogue (via email) until the aims and structure were finalized, after which three working groups were established. Each working group was asked to provide a narrative review of the available evidence on their topic area, focusing on randomized controlled trials and systematic reviews and meta-analysis where possible, and to draft specific recommendations for further discussion. This was done in an iterative manner over an 8-month period. A complete draft of the manuscript was then sent to all authors for review (multiple rounds of email correspondence over 3–4 months) until 100% agreement (consensus) was achieved for all the recommendations.
Screening and diagnosis of sarcopenia within the hospital setting
Definition(s) of sarcopenia, prevalence, and consequences in the hospital setting
Sarcopenia is defined as a progressive and generalized skeletal muscle disease that is characterised by an accelerated loss of muscle mass, strength, and/or function (12–14). Sarcopenia is a strong predictor of a myriad of adverse outcomes, such as frailty (14), falls and fractures (15) and mortality (16). In hospitalized older adults, sarcopenia is associated with longer hospital stays, higher healthcare costs, greater risk of hospital readmission and mortality (17, 18). In Australia, sarcopenia was formally recognized as a disease in 2019 with an International Classification of Diseases (ICD) code (19). However, since no international consensus has been reached for an operational definition of sarcopenia, the reported prevalence in hospital settings is variable, ranging from 10% to 35% (17, 19–22), and up to over 50% in post-acute inpatient rehabilitation (23, 24). Sarcopenia often occurs as a comorbid disease in hospitalized older adults (25), which is associated with an even higher risk of institutionalization and mortality (26). Extended periods of bed rest during hospitalization may further contribute to loss of muscle mass and strength (27). In fact, up to 15% of older adults without sarcopenia at hospital admission may meet the criteria for sarcopenia at discharge (28). Furthermore, muscle mass and strength decline may continue even after discharge from acute hospitalization (29), highlighting the need for sarcopenia screening and/or assessment to be included as part of routine care for older hospitalized patients to optimize management.
Sarcopenia screening tools within the hospital setting
Screening hospitalized older patients for sarcopenia may be useful to help identify those with, or at risk of sarcopenia. One tool that is available and recommended by several key expert groups [European Working Group on Sarcopenia in Older People (EWGSOP) (30), Society on Sarcopenia, Cachexia and Wasting Disorders (SCWD) (31); International Conference on Sarcopenia and Frailty Research (ICFSR) (32)] is the Strength, Assistance in walking, Rise from a chair, Climbing stairs and Falls history (SARC-F) questionnaire, with score of ≥4 predictive of sarcopenia (33). However, a review evaluating SARC-F as a screening tool for sarcopenia from 29 studies (n=21,855 participants) from a range of settings [community-dwelling, geriatric inpatient and outpatient, nursing homes, and long-term care populations], found that SARC-F had low to moderate sensitivity (29–55%) and moderate to high specificity (69–89%), independent of the sarcopenia definition used and population studied (34). Two recent studies involving hospitalized older adults with hip fracture or in geriatric rehabilitation reported mixed findings regarding the sensitivity and specificity of SARC-F for predicting sarcopenia (35, 36). Modified SARC-F versions that include calf circumference (SARC-Calf) (37), thigh circumference (SARC-F+TC), both calf and thigh measures (SARC-F+CC+TC) (38), or age and BMI (SARC-F+EBM) (39), may improve the sensitivity and diagnostic accuracy of the SARC-F, but most available data are based on older adults in the community and not hospitalized older adults. Alternative screening methods are suggested, such as the Mini Sarcopenia Risk Assessment (MSRA) questionnaire, which has two forms, the 5- or 7-items questionnaire, and includes questions related to age, number of hospitalizations in past year, physical activity level, weight loss and regularity of meals (MSRA-5) plus consumption of milk and dairy products and the number of daily meals (MSRA-7) (40). The MSRA-5 has a higher sensitivity (80–90%) compared to SARC-F, but lower specificity (60–80%) based on data from 384 community-dwelling Asian older adults aged 60+ years (40). Collectively, there is currently limited evidence available to inform whether SARC-F, modified versions of this, or other tools, represent a valid screening approach for sarcopenia in hospitalized patients. Thus, screening for sarcopenia in hospitalized older patients is not advisable at this time based on the available data.
Assessment and diagnosis of sarcopenia in the hospital setting
Most current guidelines recommend the assessment and diagnosis of sarcopenia be based on measurements related to muscle mass, strength, and/or physical function. Although there are multiple operational definitions of sarcopenia, each requires an assessment of at least two or more of these measurements, as summarized in Table 1. In 2019, the ANZSSFR recommended the EWGSOP definition to diagnose sarcopenia in Australia and New Zealand (41). However, this is currently being updated following the introduction of several new definitions of sarcopenia and a recent expert Delphi consensus process by ANZSSFR has recommended that the use of the updated EWGSOP2 definition be used in Australia and New Zealand (42).
Currently, the assessment of sarcopenia is not routinely performed in patients within clinical/hospital settings (45, 46), despite the willingness of older adults and hospitalized patients to counteract sarcopenia (47). Some common barriers to diagnosing sarcopenia in hospital settings (48–51) are outlined in Table 2 and include the presence of musculoskeletal disorders, acute illness, unmanaged pain or being bed bound. Furthermore, the status of acutely admitted patients often change during hospitalization, which can impact the feasibility, reliability, and ultimately the predictive value of measurements taken upon admission (52).
Feasibility studies in acute hospital settings suggest that many patients, except for the critically ill and some neurological/trauma patients, can complete muscle strength and physical performance measurements (48–51). However, assessment of muscle mass has the lowest completion rate (50), likely due to a lack of appropriate equipment available to measure muscle (lean) mass or its surrogates (46). EWGSOP2 recommends that those with confirmed low muscle strength be classified as probable sarcopenia (30), and the Sarcopenia Definition on Outcome Consortium (SDOC) (44) recommends only assessment of muscle strength and physical performance for sarcopenia diagnosis. In the absence of a measure of muscle mass or its surrogates, a diagnosis of probable sarcopenia can be made based on muscle strength alone (30). To diagnose sarcopenia in settings where no muscle mass diagnostic methods are available, EWGSOP2 (30) and consensus recommendations from Singapore (53) recommend that calf circumference may be used as a diagnostic proxy. Although a specific diagnostic calf circumference cut-point(s) to define low muscle mass was not defined by the EWGSOP2, they reported that a cut-off of <31 cm can predict performance and survival in older adults (30). However, when calf circumference measures were validated against DXA measures of appendicular lean mass (54–56) and assessed in a large cohort (n=17,789) of healthy adults aged ≥18 years (56), cut-offs of ≤33 cm for women and ≤34 cm for men were recommended to define low muscle mass. In older hospitalized patients, low muscle mass identified by calf circumference was associated with hospital readmissions (57), nutritional risk (58, 59) and mortality (60). However, caution is required when measuring calf circumference in patients with oedema or obesity as it may led to false-negative results (53).
Key recommendations for screening and assessment of sarcopenia in hospital settings
-
1.
There is currently insufficient evidence to support the use of any specific screening tool for sarcopenia within the hospital setting, and thus the assessment of sarcopenia (without screening) is recommended.
-
2.
Hospitalized patients aged 65 years and older, or those with conditions or circumstances (e.g., comorbidities) that may increase the risk of sarcopenia at a younger age, should be assessed for probable sarcopenia and/or sarcopenia during hospital admission.
-
3.
Probable sarcopenia and sarcopenia should be diagnosed based on an assessment of muscle strength and appendicular lean (muscle) mass. An expert Delphi consensus process by ANZSSFR currently recommends using the EWGSOP2 revised definition (42). These guidelines firstly recommend an assessment of muscle strength, which if low indicates probable sarcopenia, followed by an assessment of muscle quantity (mass) quantified by DXA or BIA, which if low confirms sarcopenia. An assessment of physical function, which if impaired, can be used to indicate severe sarcopenia.
-
4.
In the absence of availability of muscle mass quantification techniques such as DXA and BIA, calf circumference may be used as a surrogate estimate of muscle mass in patients without oedema or obesity, with cut-offs of ≤33 cm for women and ≤34 cm for men to be considered to define low muscle mass.
-
5.
Patients who meet the criteria for probable sarcopenia, sarcopenia or severe sarcopenia should be investigated for causes of low muscle strength, mass and/or function (e.g., chronic/acute disease or malnutrition), and treated accordingly.
Screening and diagnosis of frailty within hospital settings
Definition(s) of frailty, prevalence and consequences in the hospital setting
Frailty is a complex geriatric condition often defined as a diminished physiological reserve across several organ systems that results in increased vulnerability to stressors (61, 62). Frailty in hospitalized older adults is associated with falls, delirium, prolonged and recurrent hospitalization, decreased quality of life (QoL), malnutrition, functional decline, admission to residential aged care, and mortality (62–64). Various tools exist to either screen or diagnose frailty in the hospital setting, but their validity and feasibility depend on several factors, such as the population of interest (e.g., elective or acute admission) and the timing of assessment (e.g., immediately upon admission or at discharge) (65, 66).
Frailty identification within the hospital setting
The frailty status of older patients at admission is predictive of a range of adverse outcomes including inpatient mortality, length of stay, and discharge to residential aged care (7, 67). Thus, the identification of frailty in hospitalized older adults is recommended to guide clinical judgement and to prioritize care (61). There are several validated frailty screening tools available; however the Clinical Frailty Scale (CFS) (68), the Frailty Index (70) and the Hospital Frailty Risk Score (HFRS) are the most commonly used in acute settings (71) (Table 3), whilst the simpler to use FRAIL scale (69) is applied in the community setting and perhaps useful prior to discharge. The CFS, a clinical judgement-based tool that evaluates specific domains (e.g., comorbidity, function, and cognition) to generate a frailty score ranging from 1 (very fit) to 9 (terminally ill), has been identified as one of the most feasible frailty screening tools for use in acute settings (68, 72). More recently, a classification tree has been proposed to enable more reliable classification of the CFS and enable the wide translation of the CFS into clinical practice (73). The FRAIL scale is a short frailty screening instrument based on patient self-reporting and has a good predictive validity for mortality but studies in hospital settings are rare (69, 74). The HFRS, which is demonstrated to relate to increased mortality risk (75), is estimated by deriving a score among 109 diagnostic codes of the International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10) that have been assigned a score based on how well each code predicts frailty (71). Finally, the Frailty Index which assesses frailty in relation to the accumulation of health deficits, is predominantly an assessment tool derived from a comprehensive geriatric assessment (CGA), however it may be used for screening as some electronic medical records automatically generate a Frailty Index score as demonstrated in primary care in England (70, 76) Therefore, based on the available evidence routine screening for frailty is recommended for all adults aged 70 years and over within the hospital setting utilizing one of the above validated tools. Importantly, all health practitioners undertaking frailty screening should first receive appropriate training (61).
Assessment and diagnosis of frailty in the hospital setting
Frailty assessments include the Frailty Phenotype or the abovementioned Frailty Index (accumulation of deficits) (70, 77, 78). The Frailty Phenotype defines frailty as the presence of three or more of the following: weakness, slow gait speed, low physical activity, exhaustion, and unintentional weight loss (77, 79). Pre-frailty is defined when only one or two of these physical characteristics are present. The Frailty Index accounts for the cumulative deficits present in an individual across a range of physical and psychological variables (70, 78), with deficits of >21% (80) or >25% (81) (of at least 30) commonly used to represent frailty. While the prevalence of frailty is influenced by the assessment tool used (ranging from 9% to 48%), there is evidence that the Frailty Index (cumulative deficit model) typically classifies more individuals as frail compared with the Frailty Phenotype approach (82). Nevertheless, older people admitted to hospital are more likely to be frail, with frailty phenotype estimated between 40% and 66% (80, 83, 84), highlighting the need for frailty screening and assessment to become part of routine clinical practice.
Comprehensive geriatric assessment (CGA) and management is a critical process in addressing frailty in hospitalized older adults (32, 85). CGA is a personalized process covering a range of health and functional domains and, in hospital, is typically carried out by a multidisciplinary team who works collaboratively in the development and implementation of a treatment plan (85). The involvement of patients and carers in setting goals is an important part of this approach. Despite a definitive scope and content of a CGA, the World Health Organisation’s (WHO) Integrated Care for Older People (ICOPE) offers a useful framework for approaching the screening, assessment, and management of older people, with the aim of reversing or slowing losses in intrinsic capacity, defined as the composite of all the physical and mental capacities of the person (86). This approach recognizes that conditions are often interrelated and require an integrated approach to management. Regular review of frailty and associated conditions is important as the recency of assessment is prognostically most useful, reflecting the dynamic nature of frailty (87). Some of the key domains and associated conditions that should be reflected in a biopsychosocial CGA include cognitive decline, limited mobility, sarcopenia, malnutrition, visual impairment, hearing loss, depressive symptoms, social care and support, caregiver support, delirium, polypharmacy, and chronic conditions (88).
The CGA is aimed at identifying a range of reversible factors that can be prioritized and addressed to optimize care during admission. For severely frail individuals, this may include consideration of palliative options. While the full implementation of a personalized care plan may not be achievable in the acute setting, a detailed assessment and management plan, developed by a multidisciplinary hospital team, can be carried over to the primary care setting for longer term follow-up as well as through referrals for aged care support. The key to successful reablement is compliance with ongoing therapy be it physical, nutritional, or a combination of treatments. The available evidence indicates that good compliance is achieved when ongoing support and monitoring is provided so ideally contact with the patient is continued after discharge until the desired goal it reached (89, 90).
Key recommendations for screening and assessment of frailty in hospital settings
-
All hospitalized patients aged 70 years and older, or those with conditions (e.g., comorbidities) that may increase the risk of frailty at a younger age, should be screened for frailty using the Clinical Frailty Scale (CFS), the FRAIL scale, the Hospital Frailty Risk Score or the Frailty Index, depending on the resources available and objectives for each specific clinical setting.
-
Patients screened as positive for frailty (or pre-frailty) should undergo further clinical assessment for frailty using the Frailty Phenotype, Frailty Index or by using information collected from a Comprehensive Geriatric Assessment (CGA).
-
Patients identified as frail should receive follow-up by a health practitioner(s) for a multi-disciplinary CGA and development of an individualized care plan that is reviewed and revised as required.
The following sections will provide an overview of the latest evidence related to the role of nutrition, exercise and multifaceted and pharmacological interventions for the management of sarcopenia and frailty in the hospital setting.
Nutritional management strategies for sarcopenia and frailty in the hospital setting
The aim of nutritional management for sarcopenia and frailty in hospitalized older adults is to stabilize their condition during the acute phase and optimize nutritional status through the recovery phase. The primary focus is to prevent loss of muscle mass and maintain physical function and health-related QoL (91). Best practice guidelines recommend routine screening for malnutrition and implementing supportive measures, such as providing a pleasant eating environment, assistance at mealtimes, and providing energy-dense and high-quality protein rich foods (91–93). However, when such measures are insufficient in the hospital setting, and where a patient’s nutritional needs are not met, food modification, dietetic counselling, oral or enteral nutrition feeding/supplementation (especially if nutritional support is <75% of requirements over one week), or parenteral nutrition (in the case of gastrointestinal dysfunction) all need to be considered (91). For malnourished patients, nutritional interventions that include a food-first approach with oral nutrition support, and/or enteral nutrition were found to be associated with increased energy and protein intakes, reduced mortality, fewer hospital readmissions and greater weight gain (94, 95). With regards to sarcopenia and frailty, the following section will provide an overview of the current evidence for the role of nutrition for the management of these conditions within hospital settings.
The cornerstone to nutritional interventions for older hospitalized patients with or at risk of sarcopenia or frailty and/or with malnutrition is the provision of adequate energy and protein (92, 96). The European Society of Parenteral and Enteral Nutrition (ESPEN) guidelines for clinical nutrition in geriatrics recommend the provision of daily oral nutrition supplements containing 400 kcal and 30 g of protein to older hospitalized patients with or at risk of malnutrition and with chronic conditions (92). Indirect calorimetry is the gold standard to determine energy expenditure; however, it is not routinely available nor practical in hospital settings (97, 98). In that case, validated equations, such as the Schofield equation, with appropriate stress and activity factors (99), or weight-based equations can be used (97). For hospitalized geriatric patients, the ESPEN guidelines recommend an energy intake of at least 30 kcal/kg body weight, however this may be as high as 38 kcal/kg body weight in underweight older patients (92). These values are intended as a guide only and should be individualized based on regular monitoring of the patient’s weight, fluid status, and acceptance and tolerance of nutritional support. At times of critical illness, energy requirements should not exceed this value, as this may cause additional catabolic stress (98, 100). In addition, it is recommended that in the first 3–5 days upon admission, energy provision does not exceed 70% of measured energy expenditure or 20–25 kcal/kg body weight (98).
Adequate protein intake is essential to promote muscle protein synthesis (MPS), which is central to prevent or minimize loss of muscle that typically occurs during hospitalization and/or with disuse (101, 102). For older hospitalized patients, current guidelines recommend a protein intake of 1.2–1.5 g/kg body weight per day (91, 93, 103), or up to 2 g/kg body weight per day for those with critical illness or clinical conditions (e.g., burns, multi-trauma, and obesity) (98, 103, 104). Daily protein provision should be calculated using the patient’s actual body weight or adjusted body weight for obese individuals [ideal body weight + 25% excess weight (actual body weight − ideal body weight] (98, 105). Despite these recommendations, evidence to support the benefits of protein alone or as part of a ONS to prevent or attenuate muscle loss in older hospitalized patients with or at risk of sarcopenia or frailty is limited. The most comprehensive summary of the evidence to date was reported in a 2019 systematic review of randomized controlled trials (RCTs) which identified six nutrition interventions targeting markers of sarcopenia in older (>65 years) adults in hospital, three of which included an enhanced exercise program (96). The nutrition interventions ranged from two weeks to 12 months and provided an additional 10–40 g/d of protein plus varying doses of energy and other macro- and micro-nutrients (96). Meta-analysis of five studies showed that the nutritional interventions had a positive effect on grip strength (mean difference 1.97 kg) compared to controls (96). There was insufficient data for meta-analysis on muscle mass or function, but two of the four studies that measured lean mass reported a preservation compared to controls (96). In critically ill patients there is some evidence that protein supplementation to current recommendations may attenuate loss of muscle mass compared to standard care (102, 106), but further research is needed to determine if provision of dietary protein alone or as part of an ONS (and at what dose and frequency) may be effective to attenuate (or prevent) loss of muscle in hospitalized older adults with sarcopenia or frailty. In non-hospitalized older adults, it has been recommended that daily protein intake should be divided evenly across the three main meals at a dose of 0.4 g/kg/meal to promote MPS throughout the day (53, 103). However, the limited short-term trials examining the effects of the frequency of protein consumption and per-meal dose on muscle-based outcomes in older hospitalized patient have reported mixed findings (107, 108).
The role of specific nutrients including essential amino acids (EAAs), particularly the branched chain amino acid leucine which acts as the ‘trigger’ for MPS, beta-hydroxy beta-methylbutyrate (HMB), a metabolite of leucine that can promote MPS and inhibit muscle protein breakdown, vitamin D, creatine and omega-3 fatty acids for the management of sarcopenia and frailty has not been well studied in hospitalized older patients, with the limited evidence inconclusive (109–113). However, there is evidence from several RCTs the multi-nutrient oral supplemental nutrition which includes high quality protein, HMB, vitamin D and/or other macro- and micro-nutrients may play a role in reducing the risk of sarcopenia and other related hospital complications in older hospitalized patients with or at risk of sarcopenia or frailty, recovering from hip fracture and/or with malnutrition (114–117). For instance, the NOURISH (Nutrition effect On Unplanned Readmissions and Survival in Hospitalized patients) trial involving 652 malnourished older hospitalized adults (mean age 78 years), randomized to either multi-nutrient supplementation (twice daily, 350kcal, 20g protein, 160IU vitamin D and 1.5g HMB) or placebo during hospital stay and following discharge, observed a reduction in 90-day mortality (RR 0.49, 95%CI 0.27–0.90) and improved nutritional status (OR 2.04, 95%CI 1.28–3.25), but no difference in hospital readmission (114). Further analysis showed that this multi-nutrient supplement also had a positive effect on handgrip strength (115). Several other RCTs in older patients (including those who were malnourished and sarcopenic) recovering from hip fracture also found that oral nutritional supplementation with protein, HMB and vitamin D was associated with greater muscle strength, a shorter immobilization period, accelerated wound healing and a maintenance of appendicular lean mass (114–117). The EFFORT (Effect of early nutritional support on Frailty, Functional Outcomes, and Recovery of malnourished medical inpatients) clinical trial in over 2000 patients (mean age 72 years) at risk of malnutrition demonstrated that individualized nutrition therapy to achieve energy, protein and micronutrient requirements compared to standard hospital food significantly reduced adverse clinical outcomes (defined as a composite of all-cause mortality, admission to intensive care, non-elective hospital readmission, major complications, and decline in functional status at 30 days) as well as mortality, functional decline at day 30 and activities of daily living (ADL) (118). In this study the intervention group achieved a modest daily increase of 290 kcal in energy and 10 g protein compared to controls. While further research is required to determine the effectiveness of high protein, multi-nutrient oral nutritional supplements on sarcopenia and frailty related outcomes in older hospitalized patients, it is important that all older patients are screened or assessed for malnutrition and micronutrient deficiencies (e.g., vitamin D deficiency) and treated appropriately. When oral nutrition support is inadequate (<75% of requirements over one week) or not feasible, enteral nutrition support and/or parenteral nutrition should be considered (92, 98, 119).
Exercise and mobility interventions for managing sarcopenia and frailty in hospitalized older adults
High-level evidence from RCTs (120–123) and meta-analyses (124, 125) indicate that in-hospital exercise interventions for older adults, including patients with sarcopenia and/or frailty, involving progressive resistance training (PRT) or multicomponent programs incorporating PRT with balance/gait training, are safe, feasible, and effective for preventing functional decline during hospitalization (122, 124, 126). For instance, a meta-analysis of seven RCTs examining the effects of resistance exercise interventions [typically 20–40 minutes per session, 5–7 days per week and often twice daily (morning and evening)] in 2498 acute hospitalized older adults reported significant increases in muscle strength (mean difference: grip strength 2.5 kg; leg press one-repetition maximum 19.3 kg), muscle power (mean difference: leg press, 29.5 watts) and function (mean difference: timed-up-and-go 3.4 seconds; SPPB 1.29 points) at discharge compared to usual hospital care (125). There is some evidence that combining PRT with targeted balance training for 12 weeks led to greater improvements in ADL, gait speed, grip strength and SPPB scores compared to PRT alone (121). A systematic review of 10 RCTs among older adults aged >75 years with prefrailty or frailty also reported that exercise interventions combining resistance and balance exercises improved physical symptoms of frailty (including poor mobility, balance, strength, and/or muscle mass) in primary and secondary care units (127). Collectively, these findings indicate that hospital-based resistance-based and multicomponent exercise programs are effective for improving muscle strength and physical function in hospitalized older patients.
Various hospital-based initiatives have aimed to improve in-hospital patient mobility levels by getting patients out of bed, standing, and ambulating to limit disuse-related functional decline during hospitalization. These include the End PJ Paralysis (128) and the MOVE ON (Outcomes of Mobilisation of Vulnerable Elders in Ontario) interventions that focus on early mobility assessment (within 24 hours of admission) and progressive mobilization (129), but the effectiveness of these and similar interventions (130) has been inconclusive. Other interventions using information booklets together with physiotherapy-led advice (131) or programs involving regular walking combined with rising from a chair (1–3 times per day, ∼20 minutes per session) (123) have reported positive effects by limiting functional decline or disability associated with hospitalization. However, systematic reviews examining interventions aimed at alleviating decline in physical performance (132) or muscle loss (133) in hospitalized older adults reported limited effectiveness of in-hospital mobility programs alone so are unlikely sufficient for preventing and/or treating sarcopenia. To date, there is no intervention of this type that is specifically targeted at older patients living with frailty. Nonetheless, early and regular mobilization during hospitalization (134) should be encouraged for older patients due to its potential benefits for limiting functional decline. However, there is insufficient evidence currently to support mobilization initiatives as a standalone intervention to counter loss in muscle mass and strength during hospitalization.
Multifaceted interventions combining exercise and nutrition in hospitalized older people
Clinical guidelines by the International Clinical Practice Guidelines for Sarcopenia (ICFSR) for the management of sarcopenia (32) and frailty (61) recommend high protein nutritional interventions in combination with exercise training (resistance with or without other exercise modalities). Despite some inconsistencies in the findings from studies evaluating the effectiveness of multifaceted exercise and nutrition approaches (32, 96, 111, 135–138), an 8-week, double-blinded, RCT in 140 older (≥ 65 years) hospitalized sarcopenic adults demonstrated that the consumption of a multi-nutrient drink (twice daily, 20 g whey protein, 2.8 g leucine, 800 IU vitamin D, vitamins, minerals, and fibres) enhanced the effects of a supervised multicomponent exercise (rehabilitation) program (5 days per week, 20–30 minutes, resistance, gait and balance training) on gait speed, whole-body and appendicular muscle mass, grip strength, physical function (SPPB, timed-up-and-go, chair stand), ADLs, and cognitive function (139). Several systematic reviews and meta-analyses of interventions in prefrail/frail, malnourished, and/or sarcopenic older individuals hospitalized with acute and chronic conditions (96, 111, 135–137, 140) have also found some evidence for a positive effect of protein/essential amino acid or other oral nutritional supplementation combined with exercise/rehabilitation for improving muscle mass, strength and function, and reducing frailty and frailty-related indicators. Based on the available evidence, it is recommended that multifaceted exercise and nutrition approaches be adopted for the management of sarcopenia and frailty in hospitalized older patients.
Pharmacological interventions for the management of sarcopenia and frailty
Few pharmacotherapies have been developed specifically for sarcopenia, with most being used to attenuate muscle wasting and weakness associated with conditions such as muscle trauma, metabolic and neuromuscular disease(s) and cancer. Available reviews include results from trials on anabolic approaches to increase muscle (lean) mass and improve muscle strength, such as testosterone replacement, targeting myostatin with neutralizing antibodies, targeting the activin receptor with an antagonist, or treating with selective androgen receptor modulators (141). Despite preclinical studies showing potential of these approaches for attenuating muscle loss or enhancing lean mass, translation to clinical trials is modest and fails to meet clinically relevant outcomes related to muscle strength and physical performance or frailty (142, 143). In addition, for many pharmacotherapies for sarcopenia, especially testosterone or growth hormone replacement to promote skeletal muscle anabolism, the relative risk-to-benefit ratio of these approaches must be considered and may preclude widespread application (144, 145). For example, although testosterone treatment may improve muscle strength in community dwelling older adults (146), long-term effects on disease susceptibility such as prostate cancer and cardiovascular events must be considered. These effects may be offset through consideration of co-treatments to address off-target effects or modifying the duration of treatments.
Other pharmacotherapies for sarcopenia include non-steroidal anti-inflammatory drugs (NSAIDs) to target inflammatory cytokine signalling, drugs such as mTOR inhibitors, and BIO101 or metformin, to address age-related metabolic dysfunction (142). Approaches targeting components of antiapoptotic pathways using senolytic drugs or ‘senotherapeutics’ that kill senescent cells or inhibit the senescence-associated secretory phenotype, have received considerable attention over the last decade for their potential application to treat age-related diseases (147). Despite promising therapeutic benefits, side effects of senolytics have been identified in some studies, including potential mitochondrial impairments (148) and potential cardiotoxicity (149). Furthermore, the evidence regarding the role of cellular senescence in human muscle and disease processes is limited compared to other organ systems (150).
At present, there are no safe and effective drugs recommended (or available) as frontline pharmacological therapy for sarcopenia and frailty (143). While we must await the outcome of future clinical trials, a consensus of the conduct of clinical trials for sarcopenia has been formulated (151).
Key recommendations related to nutrition, exercise, multifaceted and pharmacological interventions for hospitalized older patients with or at risk of sarcopenia or frailty
-
Older hospitalized patient identified as having probable sarcopenia, sarcopenia or frailty, with or without malnutrition, should be assessed and monitored by a dietitian to determine the most appropriate nutritional support and correct any deficiencies. Nutrition support interventions should be escalated in patients who do not meet nutritional goals during the first 3–5 days of admission.
-
Nutritional interventions delivered via whole foods that incorporate additional energy and/or protein or high protein, multi-nutrient ONS should aim to provide at least 30 kcal/kg energy and 1.2–1.5 g/kg protein per day to hospitalized patients with malnutrition, sarcopenia or frailty; however, these should be adjusted according to the patient (e.g., obesity, critical illness) and the clinical setting (e.g., ICU).
-
Multicomponent exercise programs prescribed and supervised by qualified healthcare professionals incorporating elements of resistance, challenging balance, and functional training mimicking ADLs should be implemented as early as possible following hospital admission to limit functional decline and for management of sarcopenia or frailty.
-
To optimize muscle health and function a multicomponent exercise program combined with high protein, multi-nutrient nutritional support to ensure sufficient energy, protein, and other macro/micro-nutrient is recommended.
-
There is insufficient evidence to recommend any pharmacological agents for the treatment of sarcopenia or frailty.
Pathway to change for the management of sarcopenia and frailty for healthcare professionals working within hospital settings
Translation of evidence into person-centred hospital care is a ubiquitous challenge in healthcare globally (152). Despite significant advances in knowledge in the fields of sarcopenia and frailty over the past two decades, organisational, political and cultural resistance to change can create a challenging environment for clinicians, allied healthcare professionals and researchers aiming to translate evidence into best practice in hospitals. The following section highlights some of the key barriers to change and offers potential solutions when implementing a sustainable best practice for sarcopenia and frailty management in hospitals.
Barriers to change practice within hospital settings
A range of institutional, professional, and patient/caregiver factors may be potential barriers to sarcopenia and frailty screening, diagnosis and management within hospitals (43). These include hospital guidelines and practices which may result in conflicting priorities, inadequate resourcing, and challenges in coordinating a multidisciplinary team response (43). A lack of professional awareness, education/training and knowledge about sarcopenia and frailty screening, diagnosis and its management (46, 153), and a narrow focus on the acute presenting condition, can also make change more challenging (43). In addition, issues related to availability of equipment, time constraints and lack of collaboration have also been identified as barriers that can hinder the diagnosis and management of sarcopenia (45). Finally, poor knowledge and adherence from patients and caregivers due to a lack of understanding about sarcopenia and frailty and how these conditions can be managed, and their involvement in care planning can pose a barrier to change and implementation of evidence-based practice (43).
Structural characteristics can also serve as barriers to change, and include i) dysfunctional characteristics found in most organizations, such as societal norms and values that provide stability and stasis; ii) dysfunction specific to the healthcare sector, such as the roles and responsibilities of healthcare professionals in actioning change while simultaneously being the core employees in the hospital, and iii) dysfunctional dimensions of politically managed organizations, such as non-optimizing and non-rational actions resulting from decision-making in all sectors of public policy (154). Contextual sources of resistance to change, or internal characteristics of hospitals, also need to be considered by hospital leaders in the context of structural characteristics. Firstly, it is important to acknowledge that organizing and providing high-quality care is complex. Within a hospital system, coordinating best care for patients with sarcopenia or frailty requires a synchrony of the multidisciplinary clinical team, managers, logistics staff, and service delivery staff (particularly food services). Secondly, privatisation within hospitals, such as privately contracting the delivery of public services (e.g., food services, cleaning, pathology), have not been proven to lead to improved outcomes (155). Finally, staff anxiety (both managerial and clinical) may be generalized or specific due to competing priorities when caring for patients. Anxiety may arise due to a lack of clinical knowledge or clear guidelines coupled with low levels of perceived importance (154). This is understandable in the context of an ever-changing evidence base alongside a lack of consensus regarding definitions, screening and assessment methods and management recommendations for sarcopenia and frailty.
Potential solutions for implementing change within hospital settings
Each healthcare setting and network has a unique culture with variable willingness and ability to adapt to change. However, three main components for overcoming barriers to change and successful implementation of sarcopenia and frailty diagnostics and interventions can be considered: i) initial success; ii) sustaining, and iii) spreading the change. The initial success of practice change requires an engagement from all stakeholders and knowledge of the barriers to change within the organizational context (156). Stakeholders include all members of the multidisciplinary team, operational staff, logistics, and patients, who through education and involvement in the process, may assist in supporting the rationale for change. Sufficient time should be dedicated to developing and testing practice strategies in partnership with key personnel before imbedding change into practise. Overcoming these barriers will require healthcare professional and patient/caregiver education/training and awareness initiatives on the importance of sarcopenia and frailty as a key component in acute care. There is also a need for system modification so that patients are screened and/or diagnosed for sarcopenia and frailty and educated on how best to manage their condition. Furthermore, identification of responsibility for screening, assessment and management that includes a multidisciplinary team approach involving clinicians, nurses, allied health professionals (dietitians, exercise physiologists, physiotherapists) and other relevant healthcare professionals is needed (43, 53). It is of upmost importance that frailty and sarcopenia assessment and interventions are integrated in key components of care models, such as the CGA (32, 85). Frailty and sarcopenia assessment and interventions should also be an integrated part of care models such as the ‘Hospital Elder Life Program’ (HELP) (157), ‘Nurses Improving Care for Health System Elders’ (NICHE) (158) and the ‘Acute Care for Elders (ACE) unit’, which was the first Senior Friendly Hospital (SFH) program developed in the USA in 1990 (159). Older patients treated in ACE units have improved physical function, and shorter lengths of stay and costs compared to usual care (160). Feasibility is also a critical consideration in addition to validity and reliability when selecting a tool(s) for the screening and/or diagnosis of sarcopenia and frailty. Once success is observed, plans for ongoing monitoring should be implemented with continual strategic review to ensure flexible adaptation to organizational needs (156).
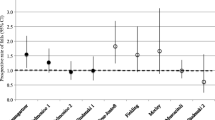
Sustainability of practice improvements is core to enhancing patient care long-term (156). When sustainable practices are spread, organization-wide culture change can flourish (156). The Sustain and Spread model, examined in Canada, has shown effectiveness in fostering culture change in nutrition care leading to positive impacts on patients (156). This model may also apply to the implementation of sarcopenia and frailty best practice. Figure 1 illustrates the Spread and Sustain model designed to lead to organisational culture change.
The Sustain and Spread Framework: Once there is initial implementation success, strategies are used to sustain and spread the successful change
Taken from Laur C et al. (156)
Change Champions — interested staff members whose role is to educate, motivate, and implement change, (161) are key for a sustainable change. An example may be a Champion nurse who provides formal/informal education to team members about the need for applying the frailty screening tool to inpatients, using improved patient care and outcomes as the motivator. While barriers to change in hospital settings are complex and extensive, by adopting a strategic approach that capitalizes on existing human resources, recognizes barriers, and employs a sustain and spread strategy, culture change aiming to improve patient care is possible.
Key recommendations related to implementing change for the management of sarcopenia and frailty for hospitals and healthcare professional working within a hospital setting
-
Organization-wide approaches within hospitals are needed to support strategies to identify, prevent, or manage sarcopenia and frailty. The Sustain and Spread model can be used to steer organisational culture change, with the help of champions within the hospital setting to strive for the routine screening, assessment and management of sarcopenia and frailty.
-
A multidisciplinary team approach incorporating clinicians, nurses, allied health professionals (dietitians, exercise physiologists, physiotherapists, occupational therapists) and other relevant healthcare professionals is recommended to ensure that screening, diagnosis and management approaches for sarcopenia and frailty are embedded and sustained within hospital settings.
-
Awareness and education initiatives are needed to upskill relevant healthcare professionals working with older hospitalized patient on screening, diagnosis and management approaches for sarcopenia and frailty.
-
Patients and caregivers’ education should be integrated into the care pathway to facilitate uptake and adherence to prescribed management approaches for sarcopenia and frailty.
Concluding Remarks
Sarcopenia and frailty are highly prevalent in older hospitalized patients, which are associated with a myriad of adverse clinical outcomes, highlighting the need for routine screening and/or assessment and subsequent management using best practice, evidence-based approaches. Our evidence-informed recommendations are intended to serve as a platform to provide guidance and facilitate change within hospital settings with regards to the uptake, dissemination and implementing of best practice screening, assessment and management approaches for sarcopenia and frailty in older hospitalized patients. This paper also intends to stimulate further research in this area to address current gaps in knowledge with the aim to provide the necessary evidence to ensure that sarcopenia and frailty screening, diagnosis and management become embedded into routine clinical practice in all hospitals. It is acknowledged however, that the multidisciplinary panel of experts from the ANZSSFR expert working group on sarcopenia and frailty developed their consensus recommendations based on a narrative review of the latest evidence from RCTs, systematic reviews and meta-analyses and current international guidelines.
References
Australian Institute of Health and Welfare 2018. Australia’s hospitals 2016–17 at a glance. Health services series no. 85. Cat. no. HSE 204. Canberra: AIHW.
Australian Institute of Health and Welfare 2018. Older Australia at a glance. Cat. no. AGE 87. Canberra: AIHW.
Ligthart-Melis GC, Luiking YC, Kakourou A, Cederholm T, Maier AB, de van der Schueren MAE. Frailty, Sarcopenia, and Malnutrition Frequently (Co-)occur in Hospitalized Older Adults: A Systematic Review and Meta-analysis. J Am Med Dir Assoc 2020;21(9):1216–28. doi: https://doi.org/10.1016/j.jamda.2020.03.006
Khandelwal D, Goel A, Kumar U, Gulati V, Narang R, Dey AB. Frailty is associated with longer hospital stay and increased mortality in hospitalized older patients. J Nutr Health Aging 2012;16(8):732–5. doi: https://doi.org/10.1007/s12603-012-0369-5
Sousa AS, Guerra RS, Fonseca I, Pichel F, Amaral TF. Sarcopenia and length of hospital stay. Eur J Clin Nutr 2016;70(5):595–601. doi: https://doi.org/10.1038/ejcn.2015.207
Yang M, Hu X, Wang H, Zhang L, Hao Q, Dong B. Sarcopenia predicts readmission and mortality in elderly patients in acute care wards: a prospective study. J Cachexia Sarcopenia Muscle 2017;8(2):251–8. doi: https://doi.org/10.1002/jcsm.12163
Hatcher VH, Galet C, Lilienthal M, Skeete DA, Romanowski KS. Association of Clinical Frailty Scores With Hospital Readmission for Falls After Index Admission for Trauma-Related Injury. JAMA Netw Open 2019;2(10):e1912409. doi: https://doi.org/10.1001/jamanetworkopen.2019.12409
O’Shea E, Trawley S, Manning E, Barrett A, Browne V, Timmons S. Malnutrition in Hospitalised Older Adults: A Multicentre Observational Study of Prevalence, Associations and Outcomes. J Nutr Health Aging 2017;21(7):830–6. doi: https://doi.org/10.1007/s12603-016-0831-x
Hirani V, Blyth F, Naganathan V, Le Couteur DG, Seibel MJ, Waite LM, Handelsman DJ, Cumming RG. Sarcopenia Is Associated With Incident Disability, Institutionalization, and Mortality in Community-Dwelling Older Men: The Concord Health and Ageing in Men Project. J Am Med Dir Assoc 2015;16(7):607–13. doi: https://doi.org/10.1016/j.jamda.2015.02.006
Robinson TN, Wallace JI, Wu DS, Wiktor A, Pointer LF, Pfister SM, Sharp TJ, Buckley MJ, Moss M. Accumulated frailty characteristics predict postoperative discharge institutionalization in the geriatric patient. J Am Coll Surg 2011;213(1):37–42. doi: https://doi.org/10.1016/j.jamcollsurg.2011.01.056
Bagshaw SM, Stelfox HT, Johnson JA, McDermid RC, Rolfson DB, Tsuyuki RT, Ibrahim Q, Majumdar SR. Long-term association between frailty and health-related quality of life among survivors of critical illness: a prospective multicenter cohort study. Crit Care Med 2015;43(5):973–82. doi: https://doi.org/10.1097/CCM.0000000000000860
Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE, Newman AB, Abellan van Kan G, Andrieu S, Bauer J, Breuille D, et al. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc 2011;12(4):249–56. doi: https://doi.org/10.1016/j.jamda.2011.01.003
Rosenberg IH. Sarcopenia: origins and clinical relevance. Clin Geriatr Med 2011;27(3):337–9. doi: https://doi.org/10.1016/j.cger.2011.03.003
Cruz-Jentoft AJ, Sayer AA. Sarcopenia. The Lancet 2019;393(10191):2636–46. doi: https://doi.org/10.1016/S0140-6736(19)31138-9
Yeung SSY, Reijnierse EM, Pham VK, Trappenburg MC, Lim WK, Meskers CGM, Maier AB. Sarcopenia and its association with falls and fractures in older adults: A systematic review and meta-analysis. J Cachexia Sarcopenia Muscle 2019;10(3):485–500. doi: https://doi.org/10.1002/jcsm.12411
Xu J, Wan CS, Ktoris K, Reijnierse EM, Maier AB. Sarcopenia Is Associated with Mortality in Adults: A Systematic Review and Meta-Analysis. Gerontology 2021:1–16. doi: https://doi.org/10.1159/000517099
Gariballa S, Alessa A. Sarcopenia: Prevalence and prognostic significance in hospitalized patients. Clinical Nutrition 2013;32(5):772–6. doi: https://doi.org/10.1016/j.clnu.2013.01.010
Antunes AC, Araújo DA, Veríssimo MT, Amaral TF. Sarcopenia and hospitalisation costs in older adults: a cross-sectional study. Nutrition & Dietetics 2017;74(1):46–50. doi: https://doi.org/10.1111/1747-0080.12287
Zanker J, Scott D, Brennan-Olsen SL, Duque G. Sarcopenia: a deserving recipient of an Australian ICD-10-AM code. Medical Journal of Australia 2020;212(1). doi: https://doi.org/10.5694/mja2.50432
Smoliner C, Sieber CC, Wirth R. Prevalence of Sarcopenia in Geriatric Hospitalized Patients. J Am Med Direct Assoc 2014;15(4):267–72. doi: https://doi.org/10.1016/j.jamda.2013.11.027
Hao Q, Hu X, Xie L, Chen J, Jiang J, Dong B, Yang M. Prevalence of sarcopenia and associated factors in hospitalised older patients: A cross-sectional study. Australas J Ageing 2018;37(1):62–7. doi: https://doi.org/10.1111/ajag.12492
Bianchi L, Abete P, Bellelli G, Bo M, Cherubini A, Corica F, Di Bari M, Maggio M, Manca GM, Rizzo MR, et al. Prevalence and Clinical Correlates of Sarcopenia, Identified According to the EWGSOP Definition and Diagnostic Algorithm, in Hospitalized Older People: The GLISTEN Study. J Gerontol A Biol Sci Med Sci 2017;72(11):1575–81. doi: https://doi.org/10.1093/gerona/glw343
Churilov I, Churilov L, MacIsaac RJ, Ekinci EI. Systematic review and meta-analysis of prevalence of sarcopenia in post acute inpatient rehabilitation. Osteoporos Int 2018;29(4):805–12. doi: https://doi.org/10.1007/s00198-018-4381-4
Van Ancum JM, Alcazar J, Meskers CGM, Nielsen BR, Suetta C, Maier AB. Impact of using the updated EWGSOP2 definition in diagnosing sarcopenia: A clinical perspective. Arch Gerontol Geriatr 2020;90:104125. doi: https://doi.org/10.1016/j.archger.2020.104125
Pacifico J, Geerlings MAJ, Reijnierse EM, Phassouliotis C, Lim WK, Maier AB. Prevalence of sarcopenia as a comorbid disease: A systematic review and meta-analysis. Exp Gerontol 2020;131:110801. doi: https://doi.org/10.1016/j.exger.2019.110801
Pacifico J, Reijnierse EM, Lim WK, Maier AB. The Association between Sarcopenia as a Comorbid Disease and Incidence of Institutionalisation and Mortality in Geriatric Rehabilitation Inpatients: REStORing health of acutely unwell adulTs (RESORT). Gerontology 2021:1–11. doi: https://doi.org/10.1159/000517461
Van Ancum JM, Scheerman K, Jonkman NH, Smeenk HE, Kruizinga RC, Meskers CGM, Maier AB. Change in muscle strength and muscle mass in older hospitalized patients: A systematic review and meta-analysis. Exp Gerontol 2017;92:34–41. doi: https://doi.org/10.1016/j.exger.2017.03.006
Martone AM, Bianchi L, Abete P, Bellelli G, Bo M, Cherubini A, Corica F, Bari MD, Maggio M, Manca GM, et al. The incidence of sarcopenia among hospitalized older patients: results from the Glisten study. Journal of Cachexia, Sarcopenia and Muscle 2017;8(6):907–14. doi: https://doi.org/10.1002/jcsm.12224
Aarden JJ, Reijnierse EM, van der Schaaf M, van der Esch M, Reichardt LA, van Seben R, Bosch JA, Twisk JWR, Maier AB, Engelbert RHH, et al. Longitudinal Changes in Muscle Mass, Muscle Strength, and Physical Performance in Acutely Hospitalized Older Adults. J Am Med Dir Assoc 2021;22(4):839–45 e1. doi: https://doi.org/10.1016/j.jamda.2020.12.006
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, Cooper C, Landi F, Rolland Y, Sayer AA, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age and Ageing 2019;48(1):16–31. doi: https://doi.org/10.1093/ageing/afy169
Bauer J, Morley JE, Schols A, Ferrucci L, Cruz-Jentoft AJ, Dent E, Baracos VE, Crawford JA, Doehner W, Heymsfield SB, et al. Sarcopenia: A Time for Action. An SCWD Position Paper. J Cachexia Sarcopenia Muscle 2019;10(5):956–61. doi: https://doi.org/10.1002/jcsm.12483
Dent E, Morley JE, Cruz-Jentoft AJ, Arai H, Kritchevsky SB, Guralnik J, Bauer JM, Pahor M, Clark BC, Cesari M, et al. International Clinical Practice Guidelines for Sarcopenia (ICFSR): Screening, Diagnosis and Management. J Nutr Health Aging 2018;22(10):1148–61. doi: https://doi.org/10.1007/s12603-018-1139-9
Malmstrom TK, Morley JE. SARC-F: a simple questionnaire to rapidly diagnose sarcopenia. J Am Med Dir Assoc 2013;14(8):531–2. doi: https://doi.org/10.1016/j.jamda.2013.05.018
Voelker SN, Michalopoulos N, Maier AB, Reijnierse EM. Reliability and Concurrent Validity of the SARC-F and Its Modified Versions: A Systematic Review and Meta-Analysis. J Am Med Dir Assoc 2021. doi: https://doi.org/10.1016/j.jamda.2021.05.011
Dedeyne L, Reijnierse EM, Pacifico J, Kay JE, Maggs P, Verschueren S, Tournoy J, Gielen E, Lim WK, Maier AB. SARC-F Is Inaccurate to Identify Geriatric Rehabilitation Inpatients at Risk for Sarcopenia: RESORT. Gerontology 2021:1–9. doi: https://doi.org/10.1159/000516117
Ha YC, Won Won C, Kim M, Chun KJ, Yoo JI. SARC-F as a Useful Tool for Screening Sarcopenia in Elderly Patients with Hip Fractures. J Nutr Health Aging 2020;24(1):78–82. doi: https://doi.org/10.1007/s12603-019-1307-6
Barbosa-Silva TG, Menezes AM, Bielemann RM, Malmstrom TK, Gonzalez MC, Grupo de Estudos em Composicao Corporal e N. Enhancing SARC-F: Improving sarcopenia screening in the clinical practice. J Am Med Dir Assoc 2016;17(12):1136–41. doi: https://doi.org/10.1016/j.jamda.2016.08.004
Mienche M, Setiati S, Setyohadi B, Kurniawan J, Laksmi PW, Ariane A, Tirtarahardja G. Diagnostic Performance of Calf Circumference, Thigh Circumference, and SARC-F Questionnaire to Identify Sarcopenia in Elderly Compared to Asian Working Group for Sarcopenia’s Diagnostic Standard. Acta Med Indones 2019;51(2):117–27. doi
Kurita N, Wakita T, Kamitani T, Wada O, Mizuno K. SARC-F Validation and SARC-F+EBM Derivation in Musculoskeletal Disease: The SPSS-OK Study. J Nutr Health Aging 2019;23(8):732–8. doi: https://doi.org/10.1007/s12603-019-1222-x
Yang M, Hu X, Xie L, Zhang L, Zhou J, Lin J, Wang Y, Li Y, Han Z, Zhang D, et al. Validation of the Chinese version of the Mini Sarcopenia Risk Assessment questionnaire in community-dwelling older adults. Medicine (Baltimore) 2018;97(37):e12426. doi: https://doi.org/10.1097/MD.0000000000012426
Zanker J, Scott D, Reijnierse EM, Brennan-Olsen SL, Daly RM, Girgis CM, Grossmann M, Hayes A, Henwood T, Hirani V, et al. Establishing an Operational Definition of Sarcopenia in Australia and New Zealand: Delphi Method Based Consensus Statement. J Nutr Health Aging 2019;23(1):105–10. doi: https://doi.org/10.1007/s12603-018-1113-6
Zanker J, Sim M, Brennan-Olsen SL, Duque G, Hayes A, Henwood T, Hirani V, Iuliano S, Keogh J, Lewis JR, et al. The Australian and New Zealand Society for Sarcopenia and Frailty Research (ANZSSFR) Sarcopenia Diagnosis and Management Task Force: Findings from the expert Delphi process. Australas J Ageing 2021;40:56–7.
Chen L-K, Woo J, Assantachai P, Auyeung T-W, Chou M-Y, Iijima K, Jang HC, Kang L, Kim M, Kim S, et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J Am Med Dir Assoc 2020;21(3):300–7. doi: https://doi.org/10.1016/j.jamda.2019.12.012
Bhasin S, Travison TG, Manini TM, Patel S, Pencina KM, Fielding RA, Magaziner JM, Newman AB, Kiel DP, Cooper C, et al. Sarcopenia Definition: The Position Statements of the Sarcopenia Definition and Outcomes Consortium. J Am Geriatr Soc 2020. doi: https://doi.org/10.1111/jgs.16372
Reijnierse EM, de van der Schueren MAE, Trappenburg MC, Doves M, Meskers CGM, Maier AB. Lack of knowledge and availability of diagnostic equipment could hinder the diagnosis of sarcopenia and its management. PLoS One 2017;12(10):e0185837. doi: https://doi.org/10.1371/journal.pone.0185837
Yeung SSY, Reijnierse EM, Trappenburg MC, Meskers CGM, Maier AB. Current knowledge and practice of Australian and New Zealand health-care professionals in sarcopenia diagnosis and treatment: Time to move forward! Australas J Ageing 2020;39(2):e185–e93. doi: https://doi.org/10.1111/ajag.12730
Van Ancum JM, Meskers CGM, Reijnierse EM, Yeung SSY, Jonkman NH, Trappenburg MC, Pijnappels M, Maier AB. Lack of Knowledge Contrasts the Willingness to Counteract Sarcopenia Among Community-Dwelling Adults. J Aging Health 2020;32(7–8):787–94. doi: https://doi.org/10.1177/0898264319852840
Ibrahim K, Howson FFA, Culliford DJ, Sayer AA, Roberts HC. The feasibility of assessing frailty and sarcopenia in hospitalised older people: a comparison of commonly used tools. BMC Geriatrics 2019;19(1):42. doi: https://doi.org/10.1186/s12877-019-1053-y
Ostir GV, Berges I, Kuo YF, Goodwin JS, Ottenbacher KJ, Guralnik JM. Assessing gait speed in acutely ill older patients admitted to an acute care for elders hospital unit. Arch Intern Med 2012;172(4):353–8. doi: https://doi.org/10.1001/archinternmed.2011.1615
Bruyère O, Beaudart C, Reginster JY, Buckinx F, Schoene D, Hirani V, Cooper C, Kanis JA, Rizzoli R, McCloskey E, et al. Assessment of muscle mass, muscle strength and physical performance in clinical practice: An international survey. European Geriatric Medicine 2016;7:243–6. doi: https://doi.org/10.1016/j.eurger.2015.12.009
Cerri AP, Bellelli G, Mazzone A, Pittella F, Landi F, Zambon A, Annoni G. Sarcopenia and malnutrition in acutely ill hospitalized elderly: Prevalence and outcomes. Clin Nutr 2015;34(4):745–51. doi: https://doi.org/10.1016/j.clnu.2014.08.015
Bodilsen AC, Juul-Larsen HG, Petersen J, Beyer N, Andersen O, Bandholm T. Feasibility and inter-rater reliability of physical performance measures in acutely admitted older medical patients. PLoS One 2015;10(2):e0118248. doi: https://doi.org/10.1371/journal.pone.0118248
Chew STH, Kayambu G, Lew CCH, Ng TP, Ong F, Tan J, Tan NC, Tham SL. Singapore multidisciplinary consensus recommendations on muscle health in older adults: assessment and multimodal targeted intervention across the continuum of care. BMC Geriatr 2021;21(1):314. doi: https://doi.org/10.1186/s12877-021-02240-8
Pagotto V, Santos KFD, Malaquias SG, Bachion MM, Silveira EA. Calf circumference: clinical validation for evaluation of muscle mass in the elderly. Rev Bras Enferm 2018;71(2):322–8. doi: https://doi.org/10.1590/0034-7167-2017-0121
Barbosa-Silva TG, Bielemann RM, Gonzalez MC, Menezes AM. Prevalence of sarcopenia among community-dwelling elderly of a medium-sized South American city: results of the COMO VAI? study. J Cachexia Sarcopenia Muscle 2016;7(2):136–43. doi: https://doi.org/10.1002/jcsm.12049
Gonzalez MC, Mehrnezhad A, Razaviarab N, Barbosa-Silva TG, Heymsfield SB. Calf circumference: cutoff values from the NHANES 1999–2006. Am J Clin Nutr 2021;113(6):1679–87. doi: https://doi.org/10.1093/ajcn/nqab029
Wei J, Jiao J, Chen CL, Tao WY, Ying YJ, Zhang WW, Wu XJ, Zhang XM. The association between low calf circumference and mortality: a systematic review and meta-analysis. Eur Geriatr Med 2022. doi: https://doi.org/10.1007/s41999-021-00603-3
Leandro-Merhi VA, de Aquino JLB, Reis LO. Predictors of Nutritional Risk According to NRS-2002 and Calf Circumference in Hospitalized Older Adults with Neoplasms. Nutr Cancer 2017;69(8):1219–26. doi: https://doi.org/10.1080/01635581.2017.1367942
Tarnowski M, Stein E, Marcadenti A, Fink J, Rabito E, Silva FM. Calf Circumference Is a Good Predictor of Longer Hospital Stay and Nutritional Risk in Emergency Patients: A Prospective Cohort Study. J Am Coll Nutr 2020;39(7):645–9. doi: https://doi.org/10.1080/07315724.2020.1723452
Real GG, Fruhauf IR, Sedrez JHK, Dall’Aqua EJF, Gonzalez MC. Calf Circumference: A Marker of Muscle Mass as a Predictor of Hospital Readmission. JPEN J Parenter Enteral Nutr 2018;42(8):1272–9. doi: https://doi.org/10.1002/jpen.1170
Dent E, Morley JE, Cruz-Jentoft AJ, Woodhouse L, Rodríguez-Mañas L, Fried LP, Woo J, Aprahamian I, Sanford A, Lundy J, et al. Physical Frailty: ICFSR International Clinical Practice Guidelines for Identification and Management. J Nutr Health Aging 2019;23(9):771–87. doi: https://doi.org/10.1007/s12603-019-1273-z
Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. Lancet 2019;394(10206):1365–75. doi: https://doi.org/10.1016/s0140-6736(19)31786-6
Cesari M, Prince M, Thiyagarajan JA, De Carvalho IA, Bernabei R, Chan P, Gutierrez-Robledo LM, Michel JP, Morley JE, Ong P, et al. Frailty: An Emerging Public Health Priority. J Am Med Dir Assoc 2016;17(3):188–92. doi: https://doi.org/10.1016/j.jamda.2015.12.016
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet 2013;381(9868):752–62. doi: https://doi.org/10.1016/s0140-6736(12)62167-9
van Dam CS, Hoogendijk EO, Mooijaart SP, Smulders YM, de Vet RCW, Lucke JA, Blomaard LC, Otten RHJ, Muller M, Nanayakkara PWB, et al. A narrative review of frailty assessment in older patients at the emergency department. Eur J Emerg Med 2021;28(4):266–76. doi: https://doi.org/10.1097/MEJ.0000000000000811
Kamwa V, Seccombe A, Sapey E. The evidence for assessing frailty and sarcopenia in an acute medical unit: a systematic review. Acute Med 2021;20(1):48–67. doi
Hubbard RE, Peel NM, Samanta M, Gray LC, Mitnitski A, Rockwood K. Frailty status at admission to hospital predicts multiple adverse outcomes. Age Ageing 2017;46(5):801–6. doi: https://doi.org/10.1093/ageing/afx081
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, Mitnitski A. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005;173(5):489–95. doi: https://doi.org/10.1503/cmaj.050051
Morley JE, Malmstrom TK, Miller DK. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging 2012;16(7):601–8. doi: https://doi.org/10.1007/s12603-012-0084-2
Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci 2007;62(7):722–7. doi: https://doi.org/10.1093/gerona/62.7.722
Gilbert T, Neuburger J, Kraindler J, Keeble E, Smith P, Ariti C, Arora S, Street A, Parker S, Roberts HC, et al. Development and validation of a Hospital Frailty Risk Score focusing on older people in acute care settings using electronic hospital records: an observational study. Lancet 2018;391(10132):1775–82. doi: https://doi.org/10.1016/S0140-6736(18)30668-8
Aucoin SD, Hao M, Sohi R, Shaw J, Bentov I, Walker D, McIsaac DI. Accuracy and Feasibility of Clinically Applied Frailty Instruments before Surgery: A Systematic Review and Meta-analysis. Anesthesiology 2020;133(1):78–95. doi: https://doi.org/10.1097/aln.0000000000003257
Theou O, Perez-Zepeda MU, van der Valk AM, Searle SD, Howlett SE, Rockwood K. A classification tree to assist with routine scoring of the Clinical Frailty Scale. Age Ageing 2021;50(4):1406–11. doi: https://doi.org/10.1093/ageing/afab006
Thompson MQ, Theou O, Tucker GR, Adams RJ, Visvanathan R. FRAIL scale: Predictive validity and diagnostic test accuracy. Australa J Ageing 2020;n/a(n/a). doi: https://doi.org/10.1111/ajag.12829
Eckart A, Hauser SI, Haubitz S, Struja T, Kutz A, Koch D, Neeser O, Meier MA, Mueller B, Schuetz P. Validation of the hospital frailty risk score in a tertiary care hospital in Switzerland: results of a prospective, observational study. BMJ Open 2019;9(1):e026923. doi: https://doi.org/10.1136/bmjopen-2018-026923
Clegg A, Bates C, Young J, Ryan R, Nichols L, Ann Teale E, Mohammed MA, Parry J, Marshall T. Development and validation of an electronic frailty index using routine primary care electronic health record data. Age Ageing 2016;45(3):353–60. doi: https://doi.org/10.1093/ageing/afw039
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001;56(3):M146–56. doi: https://doi.org/10.1093/gerona/56.3.m146
Mitnitski AB, Mogilner AJ, Rockwood K. Accumulation of deficits as a proxy measure of aging. ScientificWorldJournal 2001;1:323–36. doi: https://doi.org/10.1100/tsw.2001.58
Cesari M, Landi F, Vellas B, Bernabei R, Marzetti E. Sarcopenia and physical frailty: two sides of the same coin. Front Aging Neurosci 2014;6:192. doi: https://doi.org/10.3389/fnagi.2014.00192
Thompson MQ, Theou O, Yu S, Adams RJ, Tucker GR, Visvanathan R. Frailty prevalence and factors associated with the Frailty Phenotype and Frailty Index: Findings from the North West Adelaide Health Study. Australa J Ageing 2018;37(2):120–6. doi: https://doi.org/10.1111/ajag.12487
Searle SD, Mitnitski A, Gahbauer EA, Gill TM, Rockwood K. A standard procedure for creating a frailty index. BMC Geriatr 2008;8:24. doi: https://doi.org/10.1186/1471-2318-8-24
Thompson MQ, Theou O, Adams RJ, Tucker GR, Visvanathan R. Frailty state transitions and associated factors in South Australian older adults. Geriatr Gerontol Int 2018;18(11):1549–55. doi: https://doi.org/10.1111/ggi.13522
Cunha AIL, Veronese N, de Melo Borges S, Ricci NA. Frailty as a predictor of adverse outcomes in hospitalized older adults: A systematic review and meta-analysis. Ageing Res Rev 2019;56:100960. doi: https://doi.org/10.1016/j.arr.2019.100960
Widagdo I, Pratt N, Russell M, Roughead E. How common is frailty in older Australians? Australas J Ageing 2015;34(4):247–51. doi: https://doi.org/10.1111/ajag.12184
Ellis G, Gardner M, Tsiachristas A, Langhorne P, Burke O, Harwood RH, Conroy SP, Kircher T, Somme D, Saltvedt I, et al. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database Syst Rev 2017;9(9):Cd006211. doi: https://doi.org/10.1002/14651858.CD006211.pub3
World Health Organisation (WHO). World report on ageing and health. World Health Organization. 2015. https://apps.who.int/iris/handle/10665/186463.
Thompson MQ, Theou O, Tucker GR, Adams RJ, Visvanathan R. Recurrent Measurement of Frailty Is Important for Mortality Prediction: Findings from the North West Adelaide Health Study. J Am Geriatr Soc 2019;67(11):2311–7. doi: https://doi.org/10.1111/jgs.16066
Parker SG, McCue P, Phelps K, McCleod A, Arora S, Nockels K, Kennedy S, Roberts H, Conroy S. What is Comprehensive Geriatric Assessment (CGA)? An umbrella review. Age Ageing 2018;47(1):149–55. doi: https://doi.org/10.1093/ageing/afx166
McMurdo ME, Price RJ, Shields M, Potter J, Stott DJ. Should oral nutritional supplementation be given to undernourished older people upon hospital discharge? A controlled trial. J Am Geriatr Soc 2009;57(12):2239–45. doi: https://doi.org/10.1111/j.1532-5415.2009.02568.x
Neelemaat F, Lips P, Bosmans JE, Thijs A, Seidell JC, van Bokhorst-de van der Schueren MA. Short-term oral nutritional intervention with protein and vitamin D decreases falls in malnourished older adults. J Am Geriatr Soc 2012;60(4):691–9. doi: https://doi.org/10.1111/j.1532-5415.2011.03888.x
Volkert D, Beck AM, Cederholm T, Cereda E, Cruz-Jentoft A, Goisser S, de Groot L, Grosshauser F, Kiesswetter E, Norman K, et al. Management of Malnutrition in Older Patients-Current Approaches, Evidence and Open Questions. J Clin Med 2019;8(7). doi: https://doi.org/10.3390/jcm8070974
Volkert D, Beck AM, Cederholm T, Cruz-Jentoft A, Goisser S, Hooper L, Kiesswetter E, Maggio M, Raynaud-Simon A, Sieber CC, et al. ESPEN guideline on clinical nutrition and hydration in geriatrics. Clin Nutr 2019;38(1):10–47. doi: https://doi.org/10.1016/j.clnu.2018.05.024
Thibault R, Abbasoglu O, Ioannou E, Meija L, Ottens-Oussoren K, Pichard C, Rothenberg E, Rubin D, Siljamaki-Ojansuu U, Vaillant MF, et al. ESPEN guideline on hospital nutrition. Clin Nutr 2021;40(12):5684–709. doi: https://doi.org/10.1016/j.clnu.2021.09.039
Gomes F, Baumgartner A, Bounoure L, Bally M, Deutz NE, Greenwald JL, Stanga Z, Mueller B, Schuetz P. Association of Nutritional Support With Clinical Outcomes Among Medical Inpatients Who Are Malnourished or at Nutritional Risk: An Updated Systematic Review and Meta-analysis. JAMA Netw Open 2019;2(11):e1915138. doi: https://doi.org/10.1001/jamanetworkopen.2019.15138
Schuetz P, Seres D, Lobo DN, Gomes F, Kaegi-Braun N, Stanga Z. Management of disease-related malnutrition for patients being treated in hospital. Lancet 2021;398(10314):1927–38. doi: https://doi.org/10.1016/S0140-6736(21)01451-3
Rus GE, Porter J, Brunton A, Crocker M, Kotsimbos Z, Percic J, Polzella L, Willet N, Huggins CE. Nutrition interventions implemented in hospital to lower risk of sarcopenia in older adults: A systematic review of randomised controlled trials. Nutr Diet 2020;77(1):90–102. doi: https://doi.org/10.1111/1747-0080.12608
Kruizenga HM, Hofsteenge GH, Weijs PJ. Predicting resting energy expenditure in underweight, normal weight, overweight, and obese adult hospital patients. Nutr Metab (Lond) 2016;13:85. doi: https://doi.org/10.1186/s12986-016-0145-3
Singer P, Blaser AR, Berger MM, Alhazzani W, Calder PC, Casaer MP, Hiesmayr M, Mayer K, Montejo JC, Pichard C, et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr 2019;38(1):48–79. doi: https://doi.org/10.1016/j.clnu.2018.08.037
Schofield W. Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr 1985;39C(Supplement 1):5–96. doi
Preiser J-C, van Zanten AR, Berger MM, Biolo G, Casaer MP, Doig GS, Griffiths RD, Heyland DK, Hiesmayr M, Iapichino G, et al. Metabolic and nutritional support of critically ill patients: consensus and controversies. CritCare 2015;19(1):35. doi: https://doi.org/10.1186/s13054-015-0737-8
Liebau F, Sundstrom M, van Loon LJ, Wernerman J, Rooyackers O. Short-term amino acid infusion improves protein balance in critically ill patients. Crit Care 2015;19:106. doi: https://doi.org/10.1186/s13054-015-0844-6
Fetterplace K, Deane AM, Tierney A, Beach LJ, Knight LD, Presneill J, Rechnitzer T, Forsyth A, Gill BMT, Mourtzakis M, et al. Targeted Full Energy and Protein Delivery in Critically Ill Patients: A Pilot Randomized Controlled Trial (FEED Trial). JPEN: J Parenter Enteral Nutr 2018;42(8):1252–62. doi: https://doi.org/10.1002/jpen.1166
Bauer J, Biolo G, Cederholm T, Cesari M, Cruz-Jentoft AJ, Morley JE, Phillips S, Sieber C, Stehle P, Teta D, et al. Evidence-based recommendations for optimal dietary protein intake in older people: a position paper from the PROT-AGE Study Group. J Am Med Dir Assoc 2013;14(8):542–59. doi: https://doi.org/10.1016/j.jamda.2013.05.021
McClave SA, Taylor BE, Martindale RG, Warren MM, Johnson DR, Braunschweig C, McCarthy MS, Davanos E, Rice TW, Cresci GA, et al. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN: J Parenter Enteral Nutr 2016;40(2):159–211. doi: https://doi.org/10.1177/0148607115621863
Lambell KJ, Miller EG, Tatucu-Babet OA, Peake S, Ridley EJ. Nutrition management of obese critically ill adults: A survey of critical care dietitians in Australia and New Zealand. Aust Crit Care 2021;34(1):3–8. doi: https://doi.org/10.1016/j.aucc.2020.06.005
Ferrie S, Allman-Farinelli M, Daley M, Smith K. Protein Requirements in the Critically Ill: A Randomized Controlled Trial Using Parenteral Nutrition. JPEN J Parenter Enteral Nutr 2016;40(6):795–805. doi: https://doi.org/10.1177/0148607115618449
Bouillanne O, Curis E, Hamon-Vilcot B, Nicolis I, Chretien P, Schauer N, Vincent JP, Cynober L, Aussel C. Impact of protein pulse feeding on lean mass in malnourished and at-risk hospitalized elderly patients: a randomized controlled trial. Clin Nutr 2013;32(2):186–92. doi: https://doi.org/10.1016/j.clnu.2012.08.015
McNelly AS, Bear DE, Connolly BA, Arbane G, Allum L, Tarbhai A, Cooper JA, Hopkins PA, Wise MP, Brealey D, et al. Effect of Intermittent or Continuous Feed on Muscle Wasting in Critical Illness: A Phase 2 Clinical Trial. Chest 2020;158(1):183–94. doi: https://doi.org/10.1016/j.chest.2020.03.045
Cruz-Jentoft AJ, Landi F, Schneider SM, Zúñiga C, Arai H, Boirie Y, Chen L-K, Fielding RA, Martin FC, Michel J-P. Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing 2014;43(6):748–59. doi: https://doi.org/10.1093/ageing/afu115
Wandrag L, Brett SJ, Frost G, Hickson M. Impact of supplementation with amino acids or their metabolites on muscle wasting in patients with critical illness or other muscle wasting illness: a systematic review. J Hum Nutr Diet 2015;28(4):313–30. doi: https://doi.org/10.1111/jhn.12238
Cheng H, Kong J, Underwood C, Petocz P, Hirani V, Dawson B, O’Leary F. Systematic review and meta-analysis of the effect of protein and amino acid supplements in older adults with acute or chronic conditions. Br J Nutr 2018;119(5):527–42. doi: https://doi.org/10.1017/s0007114517003816
Gielen E, Beckwee D, Delaere A, De Breucker S, Vandewoude M, Bautmans I, Sarcopenia Guidelines Development Group of the Belgian Society of Geriatrics. Nutritional interventions to improve muscle mass, muscle strength, and physical performance in older people: an umbrella review of systematic reviews and meta-analyses. Nutr Rev 2021;79(2):121–47. doi: https://doi.org/10.1093/nutrit/nuaa011
Bird JK, Troesch B, Warnke I, Calder PC. The effect of long chain omega-3 polyunsaturated fatty acids on muscle mass and function in sarcopenia: A scoping systematic review and meta-analysis. Clin Nutr ESPEN 2021;46:73–86. doi: https://doi.org/10.1016/j.clnesp.2021.10.011
Deutz NE, Matheson EM, Matarese LE, Luo M, Baggs GE, Nelson JL, Hegazi RA, Tappenden KA, Ziegler TR, Group NS. Readmission and mortality in malnourished, older, hospitalized adults treated with a specialized oral nutritional supplement: A randomized clinical trial. Clin Nutr 2016;35(1):18–26. doi: https://doi.org/10.1016/j.clnu.2015.12.010
Matheson EM, Nelson JL, Baggs GE, Luo M, Deutz NE. Specialized oral nutritional supplement (ONS) improves handgrip strength in hospitalized, malnourished older patients with cardiovascular and pulmonary disease: A randomized clinical trial. Clin Nutr 2021;40(3):844–9. doi: https://doi.org/10.1016/j.clnu.2020.08.035
Malafarina V, Uriz-Otano F, Malafarina C, Martinez JA, Zulet MA. Effectiveness of nutritional supplementation on sarcopenia and recovery in hip fracture patients. A multi-centre randomized trial. Maturitas 2017;101:42–50. doi: https://doi.org/10.1016/j.maturitas.2017.04.010
Ekinci O, Yanik S, Terzioglu Bebitoglu B, Yilmaz Akyuz E, Dokuyucu A, Erdem S. Effect of Calcium beta-Hydroxy-beta-Methylbutyrate (CaHMB), Vitamin D, and Protein Supplementation on Postoperative Immobilization in Malnourished Older Adult Patients With Hip Fracture: A Randomized Controlled Study. Nutr Clin Pract 2016;31(6):829–35. doi: https://doi.org/10.1177/0884533616629628
Schuetz P, Fehr R, Baechli V, Geiser M, Deiss M, Gomes F, Kutz A, Tribolet P, Bregenzer T, Braun N, et al. Individualised nutritional support in medical inpatients at nutritional risk: a randomised clinical trial. Lancet 2019;393(10188):2312–21. doi: https://doi.org/10.1016/S0140-6736(18)32776-4
Fetterplace K, Gill BMT, Chapple LS, Presneill JJ, MacIsaac C, Deane AM. Systematic Review With Meta-Analysis of Patient-Centered Outcomes, Comparing International Guideline-Recommended Enteral Protein Delivery With Usual Care. JPEN J Parenter Enteral Nutr 2020;44(4):610–20. doi: https://doi.org/10.1002/jpen.1725
Wang R, Liang Y, Jiang J, Chen M, Li L, Yang H, Tan L, Yang M. Effectiveness of a Short-Term Mixed Exercise Program for Treating Sarcopenia in Hospitalized Patients Aged 80 Years and Older: A Prospective Clinical Trial. J Nutr Health Aging 2020;24(10):1087–93. doi: https://doi.org/10.1007/s12603-020-1429-x
Liang Y, Wang R, Jiang J, Tan L, Yang M. A randomized controlled trial of resistance and balance exercise for sarcopenic patients aged 80–99 years. Sci Rep 2020;10(1):18756. doi: https://doi.org/10.1038/s41598-020-75872-2
Martínez-Velilla N, Casas-Herrero A, Zambom-Ferraresi F, Sáez de Asteasu ML, Lucia A, Galbete A, García-Baztán A, Alonso-Renedo J, González-Glaría B, Gonzalo-Lázaro M, et al. Effect of Exercise Intervention on Functional Decline in Very Elderly Patients During Acute Hospitalization: A Randomized Clinical Trial. JAMA Intern Med 2019;179(1):28–36. doi: https://doi.org/10.1001/jamainternmed.2018.4869
Ortiz-Alonso J, Bustamante-Ara N, Valenzuela PL, Vidan-Astiz M, Rodriguez-Romo G, Mayordomo-Cava J, Javier-Gonzalez M, Hidalgo-Gamarra M, Lopez-Tatis M, Valades-Malagon MI, et al. Effect of a Simple Exercise Program on Hospitalization-Associated Disability in Older Patients: A Randomized Controlled Trial. J Am Med Dir Assoc 2020;21(4):531–7 e1. doi: https://doi.org/10.1016/j.jamda.2019.11.027
Valenzuela PL, Morales JS, Castillo-García A, Mayordomo-Cava J, García-Hermoso A, Izquierdo M, Serra-Rexach JA, Lucia A. Effects of exercise interventions on the functional status of acutely hospitalised older adults: A systematic review and meta-analysis. Ageing Res Rev 2020;61:101076. doi: https://doi.org/10.1016/j.arr.2020.101076
Carneiro MAS, Franco CMC, Silva AL, Castro ESP, Kunevaliki G, Izquierdo M, Cyrino ES, Padilha CS. Resistance exercise intervention on muscular strength and power, and functional capacity in acute hospitalized older adults: a systematic review and meta-analysis of 2498 patients in 7 randomized clinical trials. Geroscience 2021;43(6):2693–705. doi: https://doi.org/10.1007/s11357-021-00446-7
Saez de Asteasu ML, Martinez-Velilla N, Zambom-Ferraresi F, Casas-Herrero A, Cadore EL, Galbete A, Izquierdo M. Assessing the impact of physical exercise on cognitive function in older medical patients during acute hospitalization: Secondary analysis of a randomized trial. PLoS Med 2019;16(7):e1002852. doi: https://doi.org/10.1371/journal.pmed.1002852
Kidd T, Mold F, Jones C, Ream E, Grosvenor W, Sund-Levander M, Tingström P, Carey N. What are the most effective interventions to improve physical performance in pre-frail and frail adults? A systematic review of randomised control trials. BMC Geriatr 2019;19(1):184. doi: https://doi.org/10.1186/s12877-019-1196-x
Crabtree A, Lane TL, Petch T, Ekegren CL. The impact of an End-PJ-paralysis quality improvement intervention in post-acute care: an interrupted time series analysis. AIMS Medical Science 2021;8:23–35. doi: https://doi.org/10.3934/medsci.202100
Liu B, Moore JE, Almaawiy U, Chan WH, Khan S, Ewusie J, Hamid JS, Straus SE, Collaboration MO. Outcomes of Mobilisation of Vulnerable Elders in Ontario (MOVE ON): a multisite interrupted time series evaluation of an implementation intervention to increase patient mobilisation. Age Ageing 2018;47(1):112–9. doi: https://doi.org/10.1093/ageing/afx128
Brown CJ, Foley KT, Lowman JD, Jr., MacLennan PA, Razjouyan J, Najafi B, Locher J, Allman RM. Comparison of Posthospitalization Function and Community Mobility in Hospital Mobility Program and Usual Care Patients: A Randomized Clinical Trial. JAMA Intern Med 2016;176(7):921–7. doi: https://doi.org/10.1001/jamainternmed.2016.1870
Moreno NA, de Aquino BG, Garcia IF, Tavares LS, Costa LF, Giacomassi IWS, Lunardi AC. Physiotherapist advice to older inpatients about the importance of staying physically active during hospitalisation reduces sedentary time, increases daily steps and preserves mobility: a randomised trial. J Physiother 2019;65(4):208–14. doi: https://doi.org/10.1016/j.jphys.2019.08.006
Scheerman K, Raaijmakers K, Otten RHJ, Meskers CGM, Maier AB. Effect of physical interventions on physical performance and physical activity in older patients during hospitalization: a systematic review. BMC Geriatr 2018;18(1):288. doi: https://doi.org/10.1186/s12877-018-0965-2
Welch C, Majid Z, Greig C, Gladman J, Masud T, Jackson T. Interventions to ameliorate reductions in muscle quantity and function in hospitalised older adults: a systematic review towards acute sarcopenia treatment. Age Ageing 2021;50(2):394–404. doi: https://doi.org/10.1093/ageing/afaa209
Ramsey KA, Loveland P, Rojer AGM, Denehy L, Goonan R, Marston C, Kay JE, Brenan J, Trappenburg MC, Lim WK, et al. Geriatric Rehabilitation Inpatients Roam at Home! A Matched Cohort Study of Objectively Measured Physical Activity and Sedentary Behavior in Home-Based and Hospital-Based Settings. J Am Med Dir Assoc 2021. doi: https://doi.org/10.1016/j.jamda.2021.04.018
Han CY, Miller M, Yaxley A, Baldwin C, Woodman R, Sharma Y. Effectiveness of combined exercise and nutrition interventions in prefrail or frail older hospitalised patients: a systematic review and meta-analysis. BMJ Open 2020;10(12):e040146. doi: https://doi.org/10.1136/bmjopen-2020-040146
Wright J, Baldwin C. Oral nutritional support with or without exercise in the management of malnutrition in nutritionally vulnerable older people: A systematic review and meta-analysis. Clin Nutr 2018;37(6 Pt A):1879–91. doi: https://doi.org/10.1016/j.clnu.2017.09.004
Wu PY, Huang KS, Chen KM, Chou CP, Tu YK. Exercise, Nutrition, and Combined Exercise and Nutrition in Older Adults with Sarcopenia: A Systematic Review and Network Meta-analysis. Maturitas 2021;145:38–48. doi: https://doi.org/10.1016/j.maturitas.2020.12.009
Kirk B, Iuliano S, Daly RM, Duque G. Effects of protein supplementation on muscle wasting disorders: A brief update of the evidence. Australas J Ageing 2020;39 Suppl 2:3–10. doi: https://doi.org/10.1111/ajag.12853
Rondanelli M, Cereda E, Klersy C, Faliva MA, Peroni G, Nichetti M, Gasparri C, Iannello G, Spadaccini D, Infantino V, et al. Improving rehabilitation in sarcopenia: a randomized-controlled trial utilizing a muscle-targeted food for special medical purposes. J Cachexia Sarcopenia Muscle 2020;11(6):1535–47. doi: https://doi.org/10.1002/jcsm.12532
Martin-Cantero A, Reijnierse EM, Gill BMT, Maier AB. Factors influencing the efficacy of nutritional interventions on muscle mass in older adults: a systematic review and meta-analysis. Nutr Rev 2021;79(3):315–30. doi: https://doi.org/10.1093/nutrit/nuaa064
Fonseca G, Dworatzek E, Ebner N, Von Haehling S. Selective androgen receptor modulators (SARMs) as pharmacological treatment for muscle wasting in ongoing clinical trials. Expert Opin Investig Drugs 2020;29(8):881–91. doi: https://doi.org/10.1080/13543784.2020.1777275
Hardee JP, Lynch GS. Current pharmacotherapies for sarcopenia. Expert Opin Pharmacother 2019;20(13):1645–57. doi: https://doi.org/10.1080/14656566.2019.1622093
Rooks D, Roubenoff R. Development of Pharmacotherapies for the Treatment of Sarcopenia. J Frailty Aging 2019;8(3):120–30. doi: https://doi.org/10.14283/jfa.2019.11
Bhasin S. Testosterone replacement in aging men: an evidence-based patient-centric perspective. J Clin Invest 2021;131(4). doi: https://doi.org/10.1172/JCI146607
Sattler FR, Castaneda-Sceppa C, Binder EF, Schroeder ET, Wang Y, Bhasin S, Kawakubo M, Stewart Y, Yarasheski KE, Ulloor J, et al. Testosterone and growth hormone improve body composition and muscle performance in older men. J Clin Endocrinol Metab 2009;94(6):1991–2001. doi: https://doi.org/10.1210/jc.2008-2338
Gharahdaghi N, Rudrappa S, Brook MS, Idris I, Crossland H, Hamrock C, Abdul Aziz MH, Kadi F, Tarum J, Greenhaff PL, et al. Testosterone therapy induces molecular programming augmenting physiological adaptations to resistance exercise in older men. J Cachexia Sarcopenia Muscle 2019;10(6):1276–94. doi: https://doi.org/10.1002/jcsm.12472
Khosla S, Farr JN, Tchkonia T, Kirkland JL. The role of cellular senescence in ageing and endocrine disease. Nat Rev Endocrinol 2020;16(5):263–75. doi: https://doi.org/10.1038/s41574-020-0335-y
Birch J, Passos JF. Targeting the SASP to combat ageing: Mitochondria as possible intracellular allies? Bioessays 2017;39(5). doi: https://doi.org/10.1002/bies.201600235
Owens WA, Walaszczyk A, Spyridopoulos I, Dookun E, Richardson GD. Senescence and senolytics in cardiovascular disease: Promise and potential pitfalls. Mech Ageing Dev 2021;198:111540. doi: https://doi.org/10.1016/j.mad.2021.111540
Tuttle CSL, Luesken SWM, Waaijer MEC, Maier AB. Senescence in tissue samples of humans with age-related diseases: A systematic review. Ageing Res Rev 2021;68:101334. doi: https://doi.org/10.1016/j.arr.2021.101334
Reginster JY, Beaudart C, Al-Daghri N, Avouac B, Bauer J, Bere N, Bruyere O, Cerreta F, Cesari M, Rosa MM, et al. Update on the ESCEO recommendation for the conduct of clinical trials for drugs aiming at the treatment of sarcopenia in older adults. Aging Clin Exp Res 2021;33(1):3–17. doi: https://doi.org/10.1007/s40520-020-01663-4
Westfall JM, Mold J, Fagnan L. Practice-based research—“Blue Highways” on the NIH roadmap. JAMA 2007;297(4):403–6. doi: https://doi.org/10.1001/jama.297.4.403
Windhaber T, Koula ML, Ntzani E, Velivasi A, Rizos E, Doumas MT, Pappas EE, Onder G, Vetrano DL, Roudriguez Laso A, et al. Educational strategies to train health care professionals across the education continuum on the process of frailty prevention and frailty management: a systematic review. Aging Clin Exp Res 2018;30(12):1409–15. doi: https://doi.org/10.1007/s40520-018-0918-9
Edwards N, Saltman RB. Re-thinking barriers to organizational change in public hospitals. Isr J Health Policy Res 2017;6:8. doi: https://doi.org/10.1186/s13584-017-0133-8
Hunter DJ. The Slow, Lingering Death of the English NHS: Comment on “Who Killed the English National Health Service?”. Int J Health Policy Manag 2015;5(1):55–7. doi: https://doi.org/10.15171/ijhpm.2015.165
Laur C, Bell J, Valaitis R, Ray S, Keller H. The Sustain and Spread Framework: strategies for sustaining and spreading nutrition care improvements in acute care based on thematic analysis from the More-2-Eat study. BMC Health Serv Res 2018;18(1):930. doi: https://doi.org/10.1186/s12913-018-3748-8
Hshieh TT, Yang T, Gartaganis SL, Yue J, Inouye SK. Hospital Elder Life Program: Systematic Review and Meta-analysis of Effectiveness. Am J Geriatr Psychiatry 2018;26(10):1015–33. doi: https://doi.org/10.1016/j.jagp.2018.06.007
Squires A, Murali KP, Greenberg SA, Herrmann LL, D’Amico C O. A Scoping Review of the Evidence About the Nurses Improving Care for Healthsystem Elders (NICHE) Program. Gerontologist 2021;61(3):e75–e84. doi: https://doi.org/10.1093/geront/gnz150
Palmer RM. The Acute Care for Elders Unit Model of Care. Geriatrics (Basel) 2018;3(3). doi: https://doi.org/10.3390/geriatrics3030059
Flood KL, Booth K, Vickers J, Simmons E, James DH, Biswal S, Deaver J, White ML, Bowman EH. Acute Care for Elders (ACE) Team Model of Care: A Clinical Overview. Geriatrics (Basel) 2018;3(3). doi: https://doi.org/10.3390/geriatrics3030050
Cullen L, Hanrahan K, Farrington M, Anderson R, Dimmer E, Miner R, Suchan T, Rod E. Evidence-Based Practice Change Champion Program Improves Quality Care. J Nurs Adm 2020;50(3):128–34. doi: https://doi.org/10.1097/NNA.0000000000000856
Funding
Funding: This article was supported by an educational grant from Abbott Australia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical standards: This manuscript complies with current laws regarding ethical standards in Australia.
Disclosures: No conflict of interest: JJF, BK, MQT, ED, ORLW, SY. RMD reports a grant form Fonterra Co-operative Group Ltd, honoraria for presentations from Abbott Australia and Nutricia Research and to serve as a member of an expert advisory committee; SI reports honoraria for presentations and to serve as a member of an expert advisory committee for Abbott Australia; DS reports a grant (fellowship) from the National Health and Medical Research Council (NHMRC); KF reports honoraria for presentations from Abbott Australia, Baxter, Avonos and Nutricia and support to attend a conference from Abbott Australia; GSL reports a grant from Nestlé Institute of Health Sciences, Lausanne; JZ reports honoraria for presentations from NW Primary Health network and is a Director of Aria Health; SK reports a grant from the National Health and Medical Research Council (NHMRC); RV reports a grant from the National Health and Medical Research Council (NHMRC), Australia Research Council (ARC) and National Institute for Healthy (Malaysia); consulting fees as a member of an expert advisory committee and honoraria for presentations and travel support from Nestle, Nutricia and Abbott Australia; ABM reports a grant from Nutricia Research and honoraria for presentations from Nutricia Research.
Rights and permissions
Open Access: This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, duplication, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
About this article
Cite this article
Daly, R.M., Iuliano, S., Fyfe, J.J. et al. Screening, Diagnosis and Management of Sarcopenia and Frailty in Hospitalized Older Adults: Recommendations from the Australian and New Zealand Society for Sarcopenia and Frailty Research (ANZSSFR) Expert Working Group. J Nutr Health Aging 26, 637–651 (2022). https://doi.org/10.1007/s12603-022-1801-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-022-1801-0