Abstract
The current study aimed to enhance the efficacy of peripheral nerve regeneration using a hydroxyapatite nanoparticle-containing collagen type I hydrogel. A solution of type I collagen, extracted from the rat tails, was incorporated with hydroxyapatite nanoparticles (with the average diameter of ~212 nm) and crosslinked with 1-ethyl-3-(3-dimethylaminopropyl)-carbodiimide (EDC) to prepare the hydrogel. The Schwann cell cultivation on the prepared hydrogel demonstrated a significantly higher cell proliferation than the tissue culture plate, as positive control, after 48 h (n = 3, P < 0.005) and 72 h (n = 3, P < 0.01). For in vivo evaluation, the prepared hydrogel was administrated on the sciatic nerve crush injury in Wistar rats. Four groups were studied: negative control (with injury but without interventions), positive control (without injury), collagen hydrogel and hydroxyapatite nanoparticle-containing collagen hydrogel. After 12 weeks, the administration of hydroxyapatite nanoparticle-containing collagen significantly (n = 4, P < 0.005) enhanced the functional behavior of the rats compared with the collagen hydrogel and negative control groups as evidenced by the sciatic functional index, hot plate latency and compound muscle action potential amplitude measurements. The overall results demonstrated the applicability of the produced hydrogel for the regeneration of peripheral nerve injuries.
Similar content being viewed by others
Introduction
Treating peripheral nerve injuries often requires sophisticated surgical procedures followed by a rarely satisfactory functional recovery [1]. Peripheral nerve defects have been treated by a variety of methods, including nerve autografts, artificial neural guidance conduits and end-to-end cooptation of the impaired nerve stumps, but the obtained results have been rarely satisfactory [2, 3]. Recent studies indicated that the local treatment of peripheral nervous system damaged sites with signaling factors could enhance the outgrowth of axons and increase the survival of injured neurons [4, 5]. One agent that has been recognized as an important signaling factor for the appropriate regeneration of nerves is calcium [6]. Studies have shown that the calcium ions play a pivotal role in the formation of functional connections of the nervous system and development of individual nerve cells [6]. Calcium-mediated signaling pathways take part in the regulation of axonal outgrowth, the specification of neurotransmitter subtype and axonal migration and extension [7, 8]. Hydroxyapatite (HAP) is a known calcium ion supply with a slow-release pattern, which has excellent bioactivity, biocompatibility and desirable biologic properties [9, 10].
Collagen type I is the most expressed collagen in the human body and is widely dispersed in the peripheral nervous system [11]. It plays an important role in the formation of sheaths surrounding the axons and nerve fascicles [12]. The sciatic nerve crush injury followed by Wallerian degeneration results in the Schwann cell and fibroblast migration into the injured site and partial degradation of collagen [13]. Collagen type I administration has been shown to enhance the axonal regeneration following the peripheral nerve injuries [14,15,16,17].
The aim of current study was to treat the sciatic nerve crush injury with a collagen type I hydrogel containing hydroxyapatite nanoparticles (nHAP). The collagen matrix was enriched with hydroxyapatite nanoparticles and investigated in terms of in vitro biocompatibility and effectiveness for the nerve regeneration in vivo.
Materials and methods
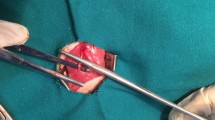
In vivo studies
Animal experiments were approved by the ethics committee of Tehran University of Medical Sciences and were carried out in accordance with the university’s guidelines. Sixteen healthy adult male Wistar rats (3 months old, weighing 250–270 g) were purchased from the Pasteur Institute (Tehran, Iran). The rats were randomly divided into four groups (4 rats per group): positive control (without injury), negative control (with injury but without interventions), collagen hydrogel and collagen + nHAP hydrogel. For the surgical procedure, the animals were anesthetized by intraperitoneal injection of ketamine 5%/xylazine 2% [(Alfasan Co., Woerden, Netherlands), 25% (v/v), 0.10 mL/100 g body weight]. The sciatic nerve crush was performed following the protocol reported by Beer et al. [18]. Briefly, a skin incision was made at the left lower limb of the rats, and a 3-mm-long crush injury, 10 mm above the bifurcation into the tibial and common peroneal nerves, was created by exerting a constant force using a non-serrated clamp for a period of 30 s. Each rat in both hydrogel groups was treated by the local injection of 0.50 mL of a single batch of each hydrogel to the site of crush injury using a 16-gauge needle. The muscle and skin were closed using no. 3-0 polyglycolic acid and silk sutures (SUPA Medical Devices, Tehran, Iran), respectively.
Cell culture studies
Primary rat Schwann cells were isolated from the sciatic nerves of adult male Wistar rats according to Terraf et al. [19]. The cells were cultured in Dulbecco’s modified Eagle’s medium: nutrient mixture F-12 (Gibco, Grand Island, NY, USA) supplemented with 10% (v/v) fetal bovine serum (Gibco, Grand Island, USA), 100 unit/mL of penicillin and 100 mg/mL of streptomycin in a humidified incubator at 37 °C with 5% CO2. The proliferation of Schwann cells on the hydrogels was assessed by a 3-(4, 5-dimethylthiazol-2-yl)-2, 5-diphenyltetrazolium bromide assay kit (Sigma-Aldrich, St. Louis, MO, USA) according to the manufacturer’s instructions. The hydrogels in a 96-well tissue culture plate were seeded with 5 × 103 Schwann cells. The cells in the wells of the plate without hydrogels were treated as positive control. All experiments were performed in triplicate, and the absorbance values were read at 570 nm by an Awareness Technology microplate reader (Palm City, FL, USA).
Chemicals
The materials and solvents were purchased from Sigma-Aldrich (St. Louis, MO, USA) and Merck (Darmstadt, Germany), respectively, unless otherwise noted.
Preparation of hydroxyapatite nanoparticles
The nHAP were synthesized following the protocol described by Ragu et al. [20]. At 33 °C, 7.48 g of Ca(OH)2 was dissolved in 100 mL of an ethanol-water mixture (1:1, v/v) and stirred for 3 h. A solution of 6.70 g NH4H2PO4 in 100 mL water was added to the Ca(OH)2 solution over a period of 24 h. The pH of the resulting slurry was adjusted to 11 by adding NaOH 1 M. The slurry finally was frozen at −80 °C for 24 h and freeze-dried (Telstar, Terrassa, Spain) for 48 h. The average diameter of the nHAP was determined after three runs using a dynamic light-scattering device (K-One, Seoul, South Korea).
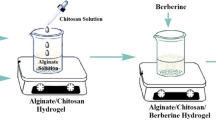
Preparation of hydrogels
Type I collagen was extracted from the rat tails (purchased from Pasteur Institute, Tehran, Iran) using the modified method described by Techatanawat et al. [21]. The sterilized extracted collagen was dissolved in an autoclaved 0.60% acetic acid in phosphate-buffered saline at a final concentration of 2 mg/mL. The pH of resulting solution was adjusted to 7 by adding autoclaved 1 M NaOH. The collagen + nHAP hydrogel was prepared by adding the autoclaved nHAP to the collagen solution at the weight ratio of 1:3 (nHAP: collagen) according to Shen et al. [22]. The collagen and nHAP-containing collagen solutions were crosslinked with 1-ethyl-3-(3-dimethylaminopropyl)-carbodiimide powder (EDC; 0.10 mM) 5 min before use.
Functional analysis
Walking-footprint analysis
Four, 8 and 12 weeks post-surgery, the rats’ footprints were recorded for the analysis of the sciatic functional index. The rats’ hind paws were soaked in the ink, and they were placed inside an acrylic corridor (43 cm length, 8.70 cm width and 5.50 cm height) lined with a millimeter paper and ended with a darkened goal box. The sciatic functional index was calculated using the following equation where PL is the distance from the heel to the top of the third toe, TS is the distance between the first and the fifth toe, and IT is the distance from the second to the fourth toe. NPL, NTS and NIT were the measures from the non-operated foot, and OPL, OTS and OIT were from the operated one [23]. In the positive control, the measures for the right foot were compared with those from the left foot. An index of 0 represented the normal function while -100 represented the complete loss of function. The sciatic functional index values for four rats in each group were averaged.
Hot plate latency test
Twelve weeks post-surgery, the rats were evaluated for the hot plate latency by placing their injured limb on a hot plate (56 °C) and recording the time until they jumped or licked their paws [24]. Following the response, the rats were removed from the plate. The cutoff time for their reaction was set at 12 s. Latencies from four rats in each group were averaged.
Nerve conduction test
Twelve weeks post-surgery, the amplitudes of the compound muscle action potential of the sciatic nerves were measured. The animals were anesthetized by intraperitoneal injection of ketamine 5%/xylazine 2% [25% (v/v), 0.10 mL/100 g body weight]. The sciatic nerve proximal to the site of the injury was stimulated with an electric stimulus (3-5 mA) using needle electrodes. The compound muscle action potential amplitudes were recorded from the needle and cap electrodes placed on the gastrocnemius muscle (filtering frequency of 10 Hz to 10 kHz, the sensitivity of 2 mV/division and sweep speed of 1 ms/division) using an electromyographic recorder (Negarandishegan, Tehran, Iran). The measurements for four rats in each group were averaged.
Gastrocnemius muscle wet weight-loss
At the end of 12th week post-surgery, the animals were sacrificed under anesthesia, and the posterior gastrocnemius muscles on the injured and uninjured hind limbs were harvested and immediately weighed to determine the wet weight-loss of muscles using the following equation [25]. The percentages for four rats in each group were averaged.
Histopathologic examination
The rats’ sciatic nerves and gastrocnemius muscles at the end of 12th-week post-surgery were fixed in 10% buffered formalin and after processing and embedding in paraffin were cross-sectioned and stained with hematoxylin-eosin (H&E). The prepared samples were examined under a light microscope (Carl Zeiss, Thornwood, NY, USA) with a digital camera (Olympus, Tokyo, Japan).
Statistical Analysis
The results were statistically analyzed by Minitab 17 software (Minitab Inc., State College, PA, USA) using one-way ANOVA, with Tukey’s post hoc test, and the data were expressed as the mean ± standard deviation (SD). In all evaluations, P < 0.05 was considered as statistically significant.
Results
The synthesized nHAP had an average diameter of 212.33 ± 33.02 nm with the polydispersity index of 0.02. The injectable hydrogels were obtained after crosslinking their solutions with EDC at room temperature (Fig. 1). The concentration of 0.10 mM EDC was chosen according to the previous study by Priyadarshani et al. [26], in which they demonstrated that this concentration is optimal for maximal cytocompatibility. Since the positive effect of obtained hydrogels on the physiology of Schwann cells, as the major cells to support the repair and regeneration of injured peripheral nerves, is desirable [27, 28], the effect of hydrogels on the proliferation of Schwann cells was investigated in vitro. Incorporation of nHAP not only did not induce any toxic effect toward Schwann cells, it enhanced their proliferation (Fig. 2). The collagen + nHAP hydrogel displayed significantly higher absorbance values than the positive control (tissue culture plate) and collagen hydrogel after 48 h (P < 0.005) and 72 h (P < 0.05).
Figure 3 displays the average sciatic functional index (SFI) values of all study groups. The positive control had an average SFI value of −4.80 ± 0.49 after 12 weeks. The average SFI values for the negative control had very little improvement and increased from −93.73 ± 2.15 after 4 weeks to −84.37 ± 2.12 and −79.44 ± 0.56 at the end of 8th and 12th weeks, respectively. The collagen + nHAP hydrogel treatment considerably enhanced the SFI value from −71.55 ± 0.48 at the end of 4th week to −54.41 ± 6.44 and −20.03 ± 0.72 after 8 and 12 weeks, respectively. These values for the collagen hydrogel group were −76.77 ± 0.92, −62.20 ± 1.81 and −31.24 ± 2.76 after 4, 8 and 12 weeks, respectively. The SFI values for the collagen + nHAP hydrogel were significantly (P < 0.005) higher than those of the collagen hydrogel at the end of 4th and 12th weeks and negative control in all time points.
The hot plate latency test was carried out to evaluate the nociceptive function of the injured limb, and the results are presented in Fig. 4. The rats in the negative control group did not withdraw their paws from the hot plate within 12 s. The positive control had the smallest hot plate latency (3.25 ± 0.50 s), and its time was significantly (P < 0.005) smaller than those of other groups. The latency for the collagen + nHAP hydrogel was recorded to be 6.25 ± 0.50 s, which was significantly (P < 0.005) smaller than the latency of the collagen hydrogel (8.75 ± 0.50 s) and negative control group.
The compound muscle action potential amplitudes as the indirect assessment of regenerated motor neurons [29] were reported in Fig. 5. The collagen + nHAP hydrogel group possessed significantly (P < 0.005) higher amplitude (19.09 ± 1.49 mV) than the collagen hydrogel (10.04 ± 2.55 mV) and negative control (5.98 ± 0.06 mV). The amplitude of the positive control (31.50 ± 0.41 mV) was significantly (P < 0.005) higher than those of the other groups.
Finally, the gastrocnemius muscle wet weight-loss as an indirect assessment of sciatic nerve regeneration efficacy [30] was assessed. As Fig. 6 shows, the treatment with both hydrogels significantly (P < 0.005) prevented the muscle weight-loss compared with the negative control group. The difference between the weight-loss percentages of collagen + nHAP hydrogel (8.45 ± 2.45%) and collagen hydrogel (15.69 ± 2.80%) were not statistically significant. The negative control had the highest weight-loss percentage (48.44 ± 6.59%) after 12 weeks.
Figure 7 illustrates the histopathologic examination of the sciatic nerves and the gastrocnemius muscles of all study groups after 12 weeks. Examination of the sciatic nerve sections of positive control showed well-arranged myelinated fibers without any histopathologic changes. In the negative control, the arrangement of fibers was disturbed, and they had swollen or missing axons with various degrees of edema and vacuolation. Severe histopathologic damages were seen in this group, including disintegration of the myelin sheath, degenerated nerve fibers, axonopathy and notable edema of the nerve fibers. The histopathologic examination of the collagen hydrogel group showed severe vacuolation, perineural fibrosis and mild edema. In the collagen + nHAP hydrogel group, the arrangement of fibers was the most similar to that of the positive control; however, there was a mild vacuolation in this group. The myelin sheath and fibers were well arranged, and there was no sign of fibrosis or inflammatory cell infiltration in this group.
Histopathologic examination of the sciatic nerve and gastrocnemius muscle cross-sections stained by hematoxylin-eosin (H&E) at the end of the 12th week post-surgery. Arrowheads vacuolation, asterisks collagen hyperplasia, thick arrows atrophied muscle fiber, thin arrows edema, double-head arrow hyalinization. The magnification for muscle cross-sections: ×400, the magnification for nerve cross-sections: ×200
Twelve weeks after sciatic nerve injury, the muscle fibers in the negative control group were shrunk, broken and wiggly. In addition, the striation of myocytes disappeared, the shrinkage of muscle fibers was evident, and the fibrosis considerably increased between the muscular cells. Hyalinization of the muscle bundles was also observed in this group. In the collagen hydrogel group, the muscular cells were disorganized, and collagen fibers proliferated between the muscular fibers. Muscular atrophy also existed in this group, but its severity was less than in the negative control. Muscular fibers in the collagen + nHAP hydrogel group were considerably regenerated with reduced fibrosis and muscular shrinkage. In the positive control group, muscle fibers were plump and red in color, which indicated an intact gastrocnemius muscle. The cross-sectional area of the gastrocnemius muscle was analyzed by Image-Pro Plus software (version 6.0, Media Cybernetics, Rockville, MD, USA), and the results are depicted in Fig. 8. Treating the sciatic nerve injury with collagen + nHAP hydrogel significantly (P < 0.005) increased the cross-sectional area compared with the collagen hydrogel and negative control groups. The positive control had the highest cross-sectional area, and its value was significantly (P < 0.005) higher than those of the other groups.
Discussion
The enhanced Schwann cell proliferation on both collagen hydrogels compared with the tissue culture plate was in contrast with the result obtained by Alberti et al. [31]. They claimed that the collagen hydrogel hydrates over time and loses its cell anchoring sites. However, we hypothesize that the higher proliferation of cells on the collagen hydrogel can be attributed to the most physiologic and biomimetic environment that it provided for the Schwann cells [32]. Incorporation of nHAP enhanced the proliferation of Schwann cells cultured on the collagen hydrogel even further. We hypothesize that the following reasons are behind this observation: first, the expected increase of the collagen + nHAP hydrogel roughness as a result of nHAP incorporation [33]. A rougher surface normally has more area for the cell attachment and consequently better proliferation [34]. Second, the internalized nHAP could be partially dissolved during the lysosomal digestion and release the calcium ions into the cytoplasm and consequently enhance the proliferation of cultured Schwann cells [35, 36]. It is worth mentioning that treating the cancer cells with nHAP led to their apoptosis [37,38,39]. This observation was mainly attributed to their high endocytosis and consequently accumulation of nHAP in them, inhibiting the synthesis of key proteins for the cell cycle progression [40].
The walking-footprint analysis, hot plate latency, nerve conduction and gastrocnemius muscle wet weight-loss are the most popular postoperative tests to assess sciatic nerve regeneration [41, 42]. Both collagen hydrogel groups significantly enhanced the nerve regeneration in all postoperative tests. The regenerative activity of collagen in neural injury treatment has been demonstrated previously [43,44,45,46]. The collagen can act as a tropic factor and guides the elongation of growth cones [47]. Calcium-mediated signaling pathways have been shown to be responsible for the axonal and dendritic outgrowth in neural cells, as well as the angiogenesis in the endothelial cells [6, 48]. Increased angiogenesis is crucial for the repair and regeneration of neural injuries [49]. The calcium ions released from the collagen + nHAP hydrogel could be easily accepted by the membranes of cells [50]. The accepted calcium ions may enhance the neural injury by enhancing the axonal outgrowth and angiogenesis in the defective area [6, 48]. Liu et al. [51] also demonstrated that the nHAP can induce axonal outgrowth by upregulating the netrin-1 expression. Netrin-1 is a protein that regulates the neuronal migration, axon guidance and synaptogenesis [52]. Madison et al. [53] showed that following the peripheral nerve injury, the netrin-1 gene is overexpressed in the Schwann cells and induces their migration [54], and proliferation [55].
Conclusion
In this study, we successfully prepared and examined a hydroxyapatite nanoparticle-containing collagen type I hydrogel for the treatment of sciatic nerve crush injury in rats. Our results revealed that the prepared hydrogel significantly enhanced the regeneration of the created defect. However, it was unsuccessful in fully restoring the complete function, indicating the need for further optimization of the produced hydrogel.
References
Ducatman BS, Scheithauer BW, Piepgras DG et al (1986) Malignant peripheral nerve sheath tumors. A clinicopathologic study of 120 cases. Cancer 57:2006–2021
Tos P, Artiaco S, Papalia I et al (2009) End-to-side nerve regeneration: from the laboratory bench to clinical applications. Int Rev Neurobiol 87:281–294
Ichihara S, Inada Y, Nakamura T (2008) Artificial nerve tubes and their application for repair of peripheral nerve injury: an update of current concepts. Injury 39:29–39
Tajdaran K, Gordon T, Wood MD et al (2016) A glial cell line-derived neurotrophic factor delivery system enhances nerve regeneration across acellular nerve allografts. Acta Biomater 29:62–70
Liu Q, Huang J, Shao H et al (2016) Dual-factor loaded functional silk fibroin scaffolds for peripheral nerve regeneration with the aid of neovascularization. RSC Adv 6:7683–7691
Henley J, M-m Poo (2004) Guiding neuronal growth cones using Ca 2 + signals. Trends Cell Biol 14:320–330
Liu M, Zhou G, Song W et al (2012) Effect of nano-hydroxyapatite on the axonal guidance growth of rat cortical neurons. Nanoscale 4:3201–3207
Akita T, Kumada T, S-i Yoshihara et al (2016) Ion channels, guidance molecules, intracellular signaling and transcription factors regulating nervous and vascular system development. J Physiol Sci 66:175–188
Xing R, Liu K, Jiao T et al (2016) An injectable self-assembling collagen-gold hybrid hydrogel for combinatorial antitumor photothermal/photodynamic therapy. Adv Mater 28:3669–3676
Wei G, Ma PX (2004) Structure and properties of nano-hydroxyapatite/polymer composite scaffolds for bone tissue engineering. Biomaterials 25:4749–4757
Longo FM, Hayman EG, Davis GE et al (1984) Neurite-promoting factors and extracellular matrix components accumulating in vivo within nerve regeneration chambers. Brain Res 309:105–117
Yao L, de Ruiter GC, Wang H et al (2010) Controlling dispersion of axonal regeneration using a multichannel collagen nerve conduit. Biomaterials 31:5789–5797
Sun W, Sun C, Lin H et al (2009) The effect of collagen-binding NGF-β on the promotion of sciatic nerve regeneration in a rat sciatic nerve crush injury model. Biomaterials 30:4649–4656
Ceballos D, Navarro X, Dubey N et al (1999) Magnetically aligned collagen gel filling a collagen nerve guide improves peripheral nerve regeneration. Exp Neurol 158:290–300
Yoshii S, Oka M (2001) Collagen filaments as a scaffold for nerve regeneration. J Biomed Mater Res 56:400–405
Phillips JB, Bunting SC, Hall SM et al (2005) Neural tissue engineering: a self-organizing collagen guidance conduit. Tissue Eng 11:1611–1617
Kemp SW, Syed S, Walsh SK et al (2009) Collagen nerve conduits promote enhanced axonal regeneration, Schwann cell association, and neovascularization compared to silicone conduits. Tissue Eng Part A 15:1975–1988
Beer GM, Steurer J, Meyer VE (2001) Standardizing nerve crushes with a non-serrated clamp. J Reconstr Microsurg 17:531–534
Terraf P, Ai J, Kouhsari S et al (2016) Indirect Co-culture with Schwann cells as a new approach for human endometrial stem cells neural transdifferentiation. Int J Stem Cell Res Transpl 4:235–242
Ragu A, Senthilarasan K, Sakthivel P (2014) Synthesis and characterization of nano hydroxyapatite with polyurethane nano composite. Der Chem Sin 5:124–127
Techatanawat S, Surarit R, Suddhasthira T et al (2011) Type I collagen extracted from rat-tail and bovine Achilles tendon for dental application: a comparative study. Asian Biomed 5:787–798
Shen X, Ruan J, Zhou Z et al (2009) Evaluation of PLGA/chitosan/HA conduits for nerve tissue reconstruction. J Wuhan Univ Technol Mater Sci Edn 24:566–570
Dijkstra JR, Meek MF, Robinson PH et al (2000) Methods to evaluate functional nerve recovery in adult rats: walking track analysis, video analysis and the withdrawal reflex. J Neurosci Methods 96:89–96
Ozdemir E, Gursoy S, Bagcivan I (2012) The effects of serotonin/norepinephrine reuptake inhibitors and serotonin receptor agonist on morphine analgesia and tolerance in rats. J Physiol Sci 62:317–323
Naseri-Nosar M, Salehi M, Hojjati-Emami S (2017) Cellulose acetate/poly lactic acid coaxial wet-electrospun scaffold containing citalopram-loaded gelatin nanocarriers for neural tissue engineering applications. Int J Biol Macromol 103:701–708
Priyadarshani P, Li Y, Yang S et al (2016) Injectable hydrogel provides growth-permissive environment for human nucleus pulposus cells. J Biomed Mater Res Part A 104:419–426
Susuki K, Kuba H (2016) Activity-dependent regulation of excitable axonal domains. J Physiol Sci 66:99–104
Salehi M, Naseri-Nosar M, Ebrahimi-Barough S et al (2017) Sciatic nerve regeneration by transplantation of Schwann cells via erythropoietin controlled-releasing polylactic acid/multiwalled carbon nanotubes/gelatin nanofibrils neural guidance conduit. J Biomed Mater Res B Appl Biomater. doi:10.1002/jbm.b.33952
Yu W, Zhao W, Zhu C et al (2011) Sciatic nerve regeneration in rats by a promising electrospun collagen/poly(ε-caprolactone) nerve conduit with tailored degradation rate. BMC Neurosci 12:68–81
Evans PJ, Mackinnon SE, Best TJ et al (1995) Regeneration across preserved peripheral nerve grafts. Muscle Nerve 18:1128–1138
Alberti KA, Hopkins AM, Tang-Schomer MD et al (2014) The behavior of neuronal cells on tendon-derived collagen sheets as potential substrates for nerve regeneration. Biomaterials 35:3551–3557
Hadjipanayi E, Mudera V, Brown R (2009) Close dependence of fibroblast proliferation on collagen scaffold matrix stiffness. Journal Tissue Eng Regen Med 3:77–84
Kane RJ, Roeder RK (2012) Effects of hydroxyapatite reinforcement on the architecture and mechanical properties of freeze-dried collagen scaffolds. J Mech Behav Biomed Mater 7:41–49
Cai L, Guinn AS, Wang S (2011) Exposed hydroxyapatite particles on the surface of photo-crosslinked nanocomposites for promoting MC3T3 cell proliferation and differentiation. Acta Biomater 7:2185–2199
Bauer IW, Li S-P, Han Y-C et al (2008) Internalization of hydroxyapatite nanoparticles in liver cancer cells. J Mater Sci Mater Med 19:1091–1095
Meador-Woodruff JH, Lewis BL, DeVries GH (1984) Cyclic AMP and calcium as potential mediators of stimulation of cultured Schwann cell proliferation by axolemma-enriched and myelin-enriched membrane fractions. Biochem Biophys Res Commun 122:373–380
Xu J, Xu P, Li Z et al (2012) Oxidative stress and apoptosis induced by hydroxyapatite nanoparticles in C6 cells. J Biomed Mater Res Part A 100:738–745
Meena R, Kesari KK, Rani M et al (2012) Effects of hydroxyapatite nanoparticles on proliferation and apoptosis of human breast cancer cells (MCF-7). J Nanopart Res 14:712–722
Yuan Y, Liu C, Qian J et al (2010) Size-mediated cytotoxicity and apoptosis of hydroxyapatite nanoparticles in human hepatoma HepG2 cells. Biomaterials 31:730–740
Han Y, Li S, Cao X et al (2014) Different inhibitory effect and mechanism of hydroxyapatite nanoparticles on normal cells and cancer cells in vitro and in vivo. Sci Rep 4:7134–7140
Bain J, Mackinnon S, Hunter D (1989) Functional evaluation of complete sciatic, peroneal, and posterior tibial nerve lesions in the rat. Plast Reconstr Surg 83:129–136
Gu Y, Zhu J, Xue C et al (2014) Chitosan/silk fibroin-based, Schwann cell-derived extracellular matrix-modified scaffolds for bridging rat sciatic nerve gaps. Biomaterials 35:2253–2263
Satou T, Nishida S, Hiruma S et al (1986) A morphological study on the effects of collagen gel matrix on regeneration of severed rat sciatic nerve in silicone tubes. Pathol Int 36:199–208
Chamberlain L, Yannas I, Hsu H et al (1998) Collagen-GAG substrate enhances the quality of nerve regeneration through collagen tubes up to level of autograft. Exp Neurol 154:315–329
Goto E, Mukozawa M, Mori H et al (2010) A rolled sheet of collagen gel with cultured Schwann cells: model of nerve conduit to enhance neurite growth. J Biosci Bioeng 109:512–518
Yoshii S, Oka M, Shima M et al (2002) 30 mm regeneration of rat sciatic nerve along collagen filaments. Brain Res 949:202–208
Labrador RO, Butí M, Navarro X (1998) Influence of collagen and laminin gels concentration on nerve regeneration after resection and tube repair. Exp Neurol 149:243–252
Faehling M, Kroll J, Föhr KJ et al (2002) Essential role of calcium in vascular endothelial growth factor A-induced signaling: mechanism of the antiangiogenic effect of carboxyamidotriazole. FASEB J 16:1805–1807
Sirén A-L, Fratelli M, Brines M et al (2001) Erythropoietin prevents neuronal apoptosis after cerebral ischemia and metabolic stress. Proc Natl Acad Sci 98:4044–4049
Nawrotek K, Tylman M, Rudnicka K et al (2016) Tubular electrodeposition of chitosan–carbon nanotube implants enriched with calcium ions. J Mech Behav Biomed Mater 60:256–266
Liu M, Zhou G, Hou Y et al (2015) Effect of nano-hydroxyapatite-coated magnetic nanoparticles on axonal guidance growth of rat dorsal root ganglion neurons. J Biomed Mater Res Part A 103:3066–3071
Xu K, Wu Z, Renier N et al (2014) Structures of netrin-1 bound to two receptors provide insight into its axon guidance mechanism. Science 344:1275–1279
Madison RD, Zomorodi A, Robinson GA (2000) Netrin-1 and peripheral nerve regeneration in the adult rat. Exp Neurol 161:563–570
Lv J, Sun X, Ma J et al (2015) Netrin-1 induces the migration of Schwann cells via p38 MAPK and PI3 K-Akt signaling pathway mediated by the UNC5B receptor. Biochem Biophys Res Commun 464:263–268
Lee HK, Seo IA, Seo E et al (2007) Netrin-1 induces proliferation of Schwann cells through Unc5b receptor. Biochem Biophys Res Commun 362:1057–1062
Author information
Authors and Affiliations
Author notes
Majid Salehi and Mahdi Naseri-Nosar have contributed equally to this work.
Corresponding author
Ethics declarations
Animal experiments were approved by the ethics committee of Tehran University of Medical Sciences and were carried out in accordance with the university’s guidelines.
Conflicts of interest
The authors declare that they have no conflicts of interest.
About this article
Cite this article
Salehi, M., Naseri-Nosar, M., Ebrahimi-Barough, S. et al. Regeneration of sciatic nerve crush injury by a hydroxyapatite nanoparticle-containing collagen type I hydrogel. J Physiol Sci 68, 579–587 (2018). https://doi.org/10.1007/s12576-017-0564-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12576-017-0564-6