Abstract
Background
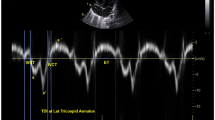
Assessment of cardiac function is crucial in pediatric patients undergoing cardiovascular surgery, monitoring cardiac output and changing hemodynamic conditions during surgery accordingly is important to improve post-surgical outcome. We aimed to measure cardiac index (CI) and maximal rate of the increase of left ventricular pressure dp/dt(max) with the pressure recording analytic method (PRAM, MostCare®) and compared it with transthoracic echocardiographic cardiac index estimation in infants with transposition of the great arteries (TGA) undergoing surgical correction.
Methods
We enrolled 74 infants with TGA consecutively into this study. CI and dp/dt(max) were measured with PRAM and echocardiography at 0, 4, 8, 12, 24 and 48 h postoperatively. Blood brain natriuretic peptide (BNP) and blood lactate (Lac) were measured at baseline and after operation.
Results
The median age at surgery was 13 days (range 1–25 days) with an average weight of 3.24 kg (range 2.31–4.17 kg). CI estimated by PRAM was 1.11 ± 0.12 L/min/m2 (range 0.69–1.36) and by Doppler echocardiography was 1.13 ± 0.13 L/min/m2 (range 0.76–1.40). dp/dt(max) estimated by PRAM was 1.31 ± 0.03 mmHg/s (range 1.23–1.43) and by Doppler echocardiography was 1.31 ± 0.04 L/min/m2 (range 1.25–1.47). CI (r = 0.817, P < 0.001) and dp/dt(max) (r = 0.794, P < 0.001) measured by two methods were highly correlated with a linear relation. Blood BNP and lactate increased to the highest level at 8–12 h post-operatively.
Conclusions
In the early post-operative period, PRAM provides reliable estimates of cardiac index and dp/dt(max) value compared with echocardiographic measurements. PRAM through mostcare® is a reliable continuous monitoring method for peri-operative management in children with congenital heart disease.




Similar content being viewed by others
References
Hamilton MA, Cecconi M, Rhodes A. A systematic review and meta-analysis on the use of preemptive hemodynamic intervention to improve postoperative outcomes in moderate and high risk surgical patients. Anesth Analg. 2011;112:1392–402.
Vincent JL, Pelosi P, Pearse R, Payen D, Perel A, Hoeft A, et al. Perioperative cardiovascular monitoring of high—risk patients: a consensus of 12. Crit Care. 2015;19:224–36.
Thompson AE. Pulmonary artery catheterization in children. New Horiz. 1997;5:244–50.
Romano SM, Pistolesi M. Assessment of cardiac output from systemic arterial pressure in humans. Crit Care Med. 2002;30:1834–41.
Garisto C, Favia I, Ricci Z, Romagnoli S, Haiberger R, Polito A, et al. Pressure recording analytical method and bioreactance for stroke volume index monitoring during pediatric cardiac surgery. Paediatr Anaesth. 2014;2:143–9.
Scolletta S, Bodson L, Donadello K, Taccone FS, Devigili A, Vincent JL, et al. Assessment of left ventricular function by pulse wave analysis in critically ill patients. Intensive Care Med. 2013;39:1025–33.
Alhashemi JA, Cecconi M, Hofer CK. Cardiac output monitoring: an integrative perspective. Crit Care. 2011;15:214–23.
Calamandrei M, Mirabile L, Muschetta S, Gensini GF, De Simone L, Romano SM. Assessment of cardiac output in children: a comparison between the pressure recording analytical method and Doppler echocardiography. Pediatr Crit Care Med. 2008;9:310–2.
Giomarelli P, Biagioli B, Scolletta S. Cardiac output monitoring by pressure recording analytical method in cardiac surgery. Eur J Cardiothorac Surg. 2004;26:515–20.
Lipshultz SE, Miller TL. Establishing norms for echocardiographic measurements of cardiovascular structures and function in children. J Appl Physiol. 1985;2005:386–8.
Yingchoncharoen T, Agarwal S, Popovic ZB, Marwick TH. Normal ranges of left ventricular strain: a meta-analysis. J Am Soc Echocardiogr. 2013;26:185–91.
Gottdiener JS, Bednarz J, Devereux R, Gardin J, Klein A, Manning WJ, et al. American Society of Echocardiography recommendations for use of echocardiography in clinical trials. J Am Soc Echocardiogr. 2004;17:1086–119.
Labovitz AJ, Buckingham TA, Habermehl K, Nelson J, Kennedy HL, Williams GA, et al. The effects of sampling site on the two-dimensional echo-Doppler determination of cardiac output. Am Heart J. 1985;109:327–32.
DuBourg O, Jondeau G, Beauchet A, Hardy A, Bourdarias JP. Doppler-derived aortic maximal acceleration: a reliable index of left ventricular systolic function. Chest. 1993;103:1064–7.
Michalak KW, Moll JA, Moll M, Dryzek P, Moszura T, Kopala M, et al. The neoaortic root in children with transposition of the great arteries after an arterial switch operation. Eur J Cardiothorac Surg. 2013;43:1101–8.
Chew MS, Poelaert J. Accuracy and repeatability of pediatric cardiac output measurement using Doppler: 20-year review of the literature. Intensive Care Med. 2003;29:1889–94.
Sangkum L, Liu GL, Yu L, Yan H, Kaye AD, Liu H. Minimally invasive of noninvasive cardiac output measurement: an update. J Anesth. 2016;30:461–80.
Marik PE. Noninvasive cardiac output monitors: a state-of the art review. J Cardiothorac Vasc Anesth. 2013;27:121–34.
Pittman J, Bar-Yosef S, SumPing J, Sherwood M, Mark J. Continuous cardiac output monitoring with pulse contour analysis: a comparison with lithium indicator dilution cardiac output measurement. Crit Care Med. 2005;33:2015–21.
Mellander M, Sabel KG, Caidahl K, Solymar L, Eriksson B. Doppler determination of cardiac output in infants and children: comparison with simultaneous thermodilution. Pediatr Cardiol. 1987;8:241–6.
Alverson DC, Eldridge M, Dillon T, Yabek SM, Berman W Jr, et al. Noninvasive pulsed Doppler determination of cardiac output in neonates and children. J Pediatr. 1982;101:46–50.
Mandelbaum-Isken VH, Linderkamp O. Cardiac output by pulsed Doppler in neonates using the apical window. Pediatr Cardiol. 1991;12:13–6.
Acknowledgements
We thank everybody of this study group members. We also thank the physicians and nurses of HBCH and OPBG-units for their dedicated work and the patients and their families for their cooperation.
Funding
No funding was secured for this study.
Author information
Authors and Affiliations
Contributions
YF designed the study, collected cases, analyzed the data and wrote the paper. RI designed the study, wrote part of the paper and corrected the original paper. WJM and FSI contributed to offer the suitable cases and related equipments. All authors contributed to the critical revision and final approval of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
The study protocol was approved by Local Ethics Committee of Hebei Province Children’s Hospital.
Conflict of interest
No financial or nonfinancial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yang, F., Iacobelli, R., Wang, JM. et al. Assessment of cardiac function in infants with transposition of the great arteries after surgery: comparison of two methods. World J Pediatr 14, 373–377 (2018). https://doi.org/10.1007/s12519-018-0178-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-018-0178-y