Abstract
Background
Children as a population have high antimicrobial prescribing rates which may lead to high resistance of bacteria according to data from some single-center surveys of antibiotic prescribing rates in China. The acquirement of baseline data of antibiotic prescribing is the basis of developing intervention strategies on inappropriate antimicrobial prescriptions. Few studies show clearly the pattern and detailed information on classes of antibiotics and distribution of indications of antibiotic prescriptions in children in China. This study aims to assess the antibiotic prescribing patterns among children and neonates hospitalized in 18 hospitals in China.
Methods
A 24-hour point prevalence survey on antimicrobial prescribing was conducted in hospitalized neonates and children in China from December 1st, 2016 to February 28th, 2017. Information on the antibiotic use of patients under 18 years of age who were administered one or more on-going antibiotics in the selected wards over a 24-hour period was collected. These data were submitted to the GARPEC (Global Antimicrobial Resistance, Prescribing and Efficacy in Children and Neonates) web-based application (https://pidrg-database.sgul.ac.uk/redcap/). For statistical analysis, Microsoft Excel 2007 and SPSS 22.0 were used.
Results
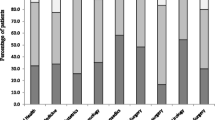
The antibiotic data were collected in 35 wards in 18 hospitals from 9 provinces. In total, 67.76% (975/1439) of the patients (n = 1439) were given at least one antibiotic, including 58.1% (173/298) of neonates (n = 298) and 70.3% (802/1141) of children (n = 1141). In neonates, the three most frequently prescribed antibiotics were third-generation cephalosporins (41.7%), penicillins plus enzyme inhibitor (23.8%), and carbapenems (11.2%). In children, the three most frequently prescribed antibiotics were third-generation cephalosporins (35.5%), macrolides (23.2%), and penicillins plus enzyme inhibitors (15.9%). The most common indication for antibiotics was proven or probable bacterial lower respiratory tract infection (30.9% in neonates and 66.6% in children).
Conclusions
Antibiotics are commonly prescribed in the Chinese children population. It is likely that the third-generation cephalosporins and macrolides are currently overused in Chinese children. Efforts must be made to ensure safe and appropriate antibiotic prescribing to reduce and prevent the future development of antibiotic resistance.


Similar content being viewed by others
References
Ardal Christine, Rottingen John-Arne, Opalska A, Van Hengel AJ, Larsen J. Pull Incentives for antibacterial drug development: an analysis by the transatlantic taskforce on antimicrobial resistance. Clin Infect Dis. 2017;65:1378–82.
Asensio A, Oliver A, González-Diego P, Baquero F, Pérez-Díaz JC, Ros P, et al. Outbreak of a multi-resistant Klebsiella pneumoniae strain in an intensive care unit: antibiotic use as risk factor for colonization and infection. Clin Infect Dis. 2000;30:55–60.
Principi N, Esposito S. Antimicrobial stewardship in paediatrics. BMC Infect Dis. 2016;16:424.
Hecker MT, Aron DC, Patel NP, Lehmann MK, Donskey CJ. Unnecessary use of antimicrobials in hospitalized patients: current patterns of misuse with an emphasis on the antianaerobic spectrum of activity. Arch Intern Med. 2003;163:972–8.
Liang X, Jin C, Wang L, Wei L, Tomson G, Rehnberg C, et al. Unnecessary use of antibiotics for inpatient children with pneumonia in two counties of rural China. Int J Clin Pharm. 2011;33:750–4.
Amadeo B, Zarb P, Muller A, Drapier N, Vankerckhoven V, Rogues AM, et al. European surveillance of antibiotic consumption(ESAC) point prevalence survey 2008: paediatric antimicrobial prescribing in 32 hospitals of 21 European countries. J Antimicrob Chemother. 2010;65:2247–52.
Xie X, Yang Q, Kuang M, Liu Y, Zhang T, Li G, et al. Analysis of the status of antibiotics use of children in China from 2004 to 2015. Zhongnan Yi Xue Ke Xue Za Zhi. 2016;44:130–4 (in Chinese).
Zhao YG, Gang Y, Guo MY, Miu F, Li BP. Analysis of antibiotics used in inpatients of the children's hospital. J Pediatric Pharm. 2006;12:5–6 (in Chinese).
Li WM, Lu YL, Li WH. Meta-analysis of antibiotic prescribing in Children with upper respiratory tract infection. Chin J Health Stat. 2017;34:625–8 (in Chinese).
Zhao YM. Analysis of survey on antibiotic usage in children. Chin Pediatr Emerg Med. 2009;16:297–8 (in Chinese).
Versporten A, Sharland M, Bielicki J, Drapier N, Vankerckhoven V, Goossens H. ARPEC project group members. The antibiotic resistance and prescribing in European children project: a neonatal and pediatric antimicrobial web-based point prevalence survey in 73 hospitals worldwide. Pediatr Infect Dis J. 2013;32:e242–53.
Sviestina I, Mozgis D. Antimicrobial usage among hospitalized children in Latvia: a neonatal and pediatric antimicrobial point prevalence survey. Med (Kaunas). 2014;50:175–81.
De Luca M, Donà D, Montagnani C, Lo Vecchio A, Romanengo M, Tagliabue C, et al. Antibiotic prescriptions and prophylaxis in Italian children. It is time to change? Data from the ARPEC project. PLoS One. 2016;11:e0154662.
Blinova E, Lau E, Bitnun A, Cox P, Schwartz S, Atenafu E, et al. Point prevalence survey of antimicrobial utilization in the cardiac and pediatric critical care unit. Pediatr Crit Care Med. 2013;14:e280–8.
Versporten A, Bielicki J, Drapier N, Sharland M, Goossens H. ARPEC project group. The worldwide antibiotic resistance and prescribing in European children(ARPEC) point prevalence survey: developing hospital-quality indicators of antibiotic prescribing for children. J Antimicrob Chemother. 2016;71:1106–17.
Lixian H, Yonghong X, Quan L, Yingchun X, Zhanliang L. Antimicrobial treatment of common pediatric infectious diseases. In: Lixian H, Yonghong X, Quan L, Yingchun X, Zhanliang L, editors. National guideline of antimicrobial treatment. Beijing: People’s Medical Publishing House; 2012. p. 12–9.
Sharland M. Neonatal infections. In: Sharland M, editor. Manual of childhood infections. 4th ed. New York: Oxford University Press; 2016. p. 220–7.
Subspecialty Group of Respiratory Diseases, The Society of Pediatrics, Chinese Medical Association, Editorial Board, Chinese Journal of Pediatrics. Guidelines for management of community acquired pneumonia in children (the revised edition of 2013) (I). Chin J Pediatr. 2013;51:745–52 (in Chinese).
Acknowledgements
The authors would like to sincerely thank all the members who participated in this study and the linguistic assistance. The authors thank the GARPEC research group for their support.
Funding
This research was funded by Sanming Project of Medicine in Shenzhen (SZSM201512030), Shenzhen Healthcare Research Project (No. SZLY2018016), and the PENTA Foundation.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to this paper. YHY, JSZ, WSZ, YJZ, and JKD were responsible for the study concept and design. YHY organized all hospitals to collect data. JSZ, GL, WSZ, HYS, GL, CAZ, CCL, YQL, YNS, DYT, MJD, CYL, LJL, XYD, PJ, PW, CMZ, and CQW collected the data of antibiotic prescriptions. JSZ contributed to the analysis and interpretation of data and writing of the manuscript. YHY and Mike Sharland revised the manuscript. All authors reviewed and agreed the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
The ethics committee of Shenzhen Children’s Hospital approved the procedures in this study. The protocol of this study was in accordance with the principles of the Declaration of Helsinki.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Zhang, JS., Liu, G., Zhang, WS. et al. Antibiotic usage in Chinese children: a point prevalence survey. World J Pediatr 14, 335–343 (2018). https://doi.org/10.1007/s12519-018-0176-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-018-0176-0