Abstract
Accurate prediction of sudden cardiac death due to ventricular arrhythmia remains challenging. Left ventricular ejection fraction has shown an association with increased risk of ventricular arrhythmias and is included in the recommendations for implantable cardioverter defibrillator as primary prevention. However, left ventricular ejection fraction may be normal in a large number of patients who are at risk of ventricular arrhythmias. Echocardiography remains the imaging technique of first choice to rule out the presence of structural heart disease and assess left and right ventricular function. Advances in strain echocardiography and cardiac magnetic resonance have provided important insights into the mechanisms of ventricular arrhythmias, and will be summarized in this review.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Accurate prediction of sudden cardiac death (SCD) due to ventricular arrhythmia remains challenging. Predictive models should take into consideration the interaction between vulnerable substrates, defined by the presence of genetic or acquired electrical, functional or structural heart disease, and the multiple transient factors (such as ischemia, catecholamine, or electrolyte dysregulations) that may precipitate the ventricular arrhythmia, making almost impossible to obtain one common predictive model for all patients, including individuals without known heart disease. Of the total number of SCD events, almost 50% occur in subjects without known heart disease.1 However, many of those individuals have subclinical coronary artery disease and accordingly, risk-profiling strategies that promote preventive and lifestyle modification therapies that reduce the risk of coronary artery disease have been encouraged.2 In patients with known ischemic heart disease and dilated cardiomyopathy, left ventricular ejection fraction (LVEF) has consistently shown an association with increased risk of ventricular arrhythmias and therefore, this variable is included in the recommendations for implantable cardioverter defibrillator (ICD) as primary prevention (class I).3 However, one third of these patients does not develop ventricular arrhythmias after ICD implantation.4 Finally, in patients with inheritable arrhythmogenic diseases, LVEF may be preserved in a large majority of patients and other variables such as duration of the corrected QT interval (in long QT syndrome), interventricular septum thickness (in hypertrophic cardiomyopathy), or right ventricular aneurysms (in arrhythmogenic dysplasia of the right ventricle) have been included in the predictive models.3
Cardiac imaging has developed several indices beyond LVEF that permit the identification of patients at high risk for SCD. Echocardiography remains the imaging technique of first choice to rule out the presence of structural heart disease and assess left and right ventricular functions. Advances in strain imaging have provided important insights into the dispersion of the mechanical activation throughout the left ventricle and the presence of heterogeneous regional function that may increase the risk of ventricular arrhythmias.5-8 Furthermore, cardiac magnetic resonance (CMR) is currently considered the reference standard for the measurement of the cardiac chamber dimensions and function and provides the unique opportunity of noninvasive myocardial tissue characterisation by identifying the presence and extent of myocardial oedema/inflammation, as well as focal, replacement, and interstitial myocardial fibrosis which can be a substrate for arrhythmia.
This review article provides an overview on current evidence showing the additional role of advanced echocardiography and CMR techniques to select patients for ICD implantation for primary prevention. Several echocardiographic and CMR-derived parameters characterizing the arrhythmogenic substrate and transient factors that may increase arrhythmogenicity in ischemic and nonischemic cardiomyopathies will be reviewed.
Ischemic Cardiomyopathy
In ischemic cardiomyopathy, the most frequent underlying mechanism of ventricular arrhythmia/fibrillation is reentry. The presence of unexcitable dense scar tissue (core infarct) forms an area of fixed conduction block whereas the surrounding areas with viable myocardium intermingled with fibrous tissue (border or peri-infarct zone) increase the nonuniform anisotropy, favors electrical uncoupling and leads to areas of unidirectional conduction block and slow conduction forming the substrate for reentry.9 Ischemia acts as a trigger of reentry by enhancing the electrical heterogeneity of the tissue, prolonging the duration of the action potential, influencing the calcium handling and myocyte membrane properties, reducing the cellular coupling and inducing redistribution of connexines.9 Furthermore, sympathetic innervation plays a role in the development of ventricular arrhythmias, and it has been shown that patients with ischemic heart disease and large mismatch between the denervated ventricular myocardium and viable myocardium have high risk of ventricular arrhythmic events.9 Although, LVEF remains the main parameter to consider ischemic heart failure patients for ICD in primary prevention, it does not reflect the complexity of the arrhythmogenic substrate and transient factors that may trigger the arrhythmias. While late gadolinium contrast-enhanced (LGE) CMR provides high spatial resolution data to characterize the infarct tissue and the components of the arrhythmogenic substrate (infarct core and border zone), several advanced echocardiographic parameters that characterize the functional properties of that substrate and have been associated with the increased risk of ventricular arrhythmias, have been proposed (Table 1).
In patients with myocardial infarction, gadolinium-based contrast agents accumulate in the increased extracellular space with a subendocardial or transmural distribution within the left ventricular wall reflecting the ischemic-necrotic wave-front phenomenon during myocardial infarction. On T1-weighted CMR acquisitions, myocardial scarring appears hyperintense (white) in contrast to the normal viable myocardium (Figure 1). Detection and quantification of myocardial fibrosis with LGE CMR has been associated with the occurrence of ventricular arrhythmias in patients with ischemic heart disease.10-15 Scott et al demonstrated in 64 patients with known coronary artery disease who underwent LGE CMR prior to ICD implantation that an increasing number of LV segments with transmural myocardial infarction was associated with increased risk of having appropriate ICD shock during follow-up (HR 1.48, 95% CI 1.18-1.84, P = 0.001), whereas LVEF was not.15 Furthermore, based on different thresholds of signal intensity compared to normal myocardium (lowest signal) or the infarct core (highest signal), the tissue heterogeneity of the scarred myocardium can be assessed with LGE CMR. The border or peri-infarct zone shows characteristically lower signal intensity than the infarct core but higher than the normal myocardium. This tissue heterogeneity has been associated with the occurrence of ventricular arrhythmias.13,14 In 91 ischemic heart failure patients receiving an ICD, each 10-g increase in peri-infarct zone was independently associated with the occurrence of ventricular arrhythmias (HR 1.49, 95% CI 1.01-2.20; P = 0.04) whereas LVEF and total infarct size were not associated.13 In addition, the analysis of the peri-infarct zone with LGE CMR permits the identification of conduction channels (critical isthmus of most ventricular arrhythmias), having important implications for ablation of ventricular tachycardia.16,17 These channels consist of bundles of viable myocardium surrounded by compact scar tissue that connect with normal myocardium by at least one side of the of the scar and have characteristically a lower signal intensity than the infarct core on LGE CMR images. These structures have been more frequently identified in patients with ischemic cardiomyopathy and ventricular arrhythmias as compared with patients without arrhythmias (88% vs 33%, P < 0.001).17 The 3-dimensional reconstruction of the myocardial scar can be merged with electroanatomical mapping and facilitate the ablation procedures by noninvasively visualizing the critical isthmus.16
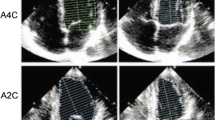
Cardiac magnetic resonance and echocardiographic speckle tracking analysis for risk stratification of patients with ischemic heart disease. Panels A and B show transmural myocardial scar in the apical septal and anteroseptal segments (arrows) and subendocardial scar in the mid-inferoseptal segment. On 2-dimensional speckle tracking echocardiography, the magnitude of global longitudinal strain is −10.6% (panel C). The LV apical segments show positive values and are color coded in blue indicating lengthening (correlating with the area of transmural scar). Panel D shows significant mechanical dispersion (65.7 ms) based on the standard deviation of time to peak longitudinal strain of 17 segments. The most delayed areas coincide with the areas with scar and impaired longitudinal strain
The electrophysiological properties of the myocardial scar may change over time and may be influenced by changes in the composition of the extracellular matrix or the presence of ischemia.18,19 For example, the presence of iron deposition in myocardial infarction has been associated with prolonged inflammation, long-corrected QT interval, isolated late potentials, and LV remodeling.20 Iron deposits are visualized on balanced steady-state free precession CMR sequences as hypointense cores and have been shown to provide incremental value to LVEF to predict ventricular arrhythmias (area under the curve 0.68 for LVEF alone, 0.87 for LVEF + hypointense cores).18 Furthermore, vasodilator stress CMR perfusion demonstrated the complementary prognostic value of reversible perfusion defects (ischemia) to the presence of LGE.19 In 254 patients with suspected or known coronary artery disease (22% with prior myocardial infarction), the presence of reversible perfussion defects was associated with a 3-fold increased risk of cardiac death after adjusting for presence of LGE, age, and gender.19
Advanced echocardiography can also assess the tissue heterogeneity of myocardial infarction focusing on the mechanical and electrical properties. Echocardiographic speckle tracking analysis informs about the deformational capacity of the LV myocardium, representing the contractile status of the myocardium. The 3-dimensional disposition of the myocardial fibers changing continuously from a right-handed helix in the subendocardium to a left-handed helix in the subepicardium determines the specific deformation of the left ventricle: shortening-lengthening in the longitudinal and circumferential directions and thickening-thinning in the radial direction.21 Myocardial infarction will alter this disposition by the deposition of collagen fibers, scar formation and remodeling increasing the functional heterogeneity of the myocardial tissue of the core infarct, the peri-infarct and the remote zone. The magnitude of global and regional LV longitudinal strain assessed with speckle tracking echocardiography has been associated with the risk of developing ventricular arrhythmias.5,8 In 988 patients after acute myocardial infarction who were followed up for a median of 28 months, the occurrence of the composite endpoint (SCD, ventricular arrhythmias, or appropriate ICD shocks) was documented in 34 (3.4%) patients.5 In this population, Ersboll et al showed that LV global longitudinal strain (GLS) was independently associated with the occurrence of the composite endpoint [hazard ratio (HR): 1.24; 95% confidence interval (CI): 1.10 to 1.40; P = 0.0004] (Figure 1). More specifically, regional LV longitudinal strain may better to characterize the function of the infarct core, border zone, and remote zone. Using regional LV longitudinal strain, Ng et al evaluated the prognostic value of the longitudinal strain of the border zone in 424 patients with ischemic heart disease recipients of an ICD.8 The infarct core zone was defined by LV segments with a value of regional longitudinal strain of >−5%, and the border zone was formed by all the surrounding segments immediately adjacent to the infarct segments. During a median follow-up of 24 months, 95 (22%) patients had appropriate ICD shocks. When the population was dichotomized according to the medial value of longitudinal strain of the border zone (≤−9.9% versus >−9.9%), patients with values ≤−9.9% (more preserved function) showed less frequently appropriate ICD shocks compared with their counterparts (8%, 11%, and 14% at 1, 2, and 3 years follow-up compared with a respective 15%, 21%, and 25%, respectively; log-rank P = 0.008).8 On multivariate analysis, each 1% deterioration in longitudinal strain of the LV segments of the border zone was independently associated with 1.22 increased HR of having ventricular arrhythmias (95% CI 1.09-1.36; P < 0.001).
In addition, the dispersion of the LV mechanical activation measured with speckle tracking echocardiography as the standard deviation of the time to peak longitudinal strain of 16 LV segments has been proposed as a surrogate to characterize the tissue heterogeneity that may predispose to ventricular arrhythmias (Figure 1).6 In a prospective multi-center study including 569 patients who survived >40 days after an acute myocardial infarction (47% with ST-segment elevation myocardial infarction), the prognostic value of LV mechanical dispersion was assessed.6 During a follow-up of 30 months, 15 (3%) patients presented with ventricular arrhythmias. Each 10-ms increase in LV mechanical dispersion was associated with increased risk of ventricular arrhythmias at follow-up (HR 1.7, 95% CI 1.2-2.5; P < 0.01), whereas LV GLS was not significantly associated. In the study by Ersboll et al above mentioned, LV mechanical dispersion was also associated with increased risk of ventricular arrhythmias (each 10 ms increase: HR 1.15, 95% CI 1.01-1.31; P = 0.032).5 It has been suggested that LV mechanical dispersion may become more relevant than LV GLS in populations with a history of myocardial infarction.7 Indeed, LV mechanical dispersion may be a consequence of scar tissue formation and collagen deposition and may promote itself ongoing ventricular remodeling and fibrosis, particularly in the infarct and border zones. In 206 patients with prior myocardial infarction (median myocardial infarction age, 6.2 years), increasing LV mechanical dispersion was associated with increased risk of ventricular arrhythmias independently of LV GLS (HR 1.12, 95% CI 1.06-1.18; P < 0.001).7
Furthermore, in ischemic heart failure patients, assessment of myocardial ischemia and viability with dobutamine stress echocardiography is of importance and has been associated with the occurrence of ventricular arrhythmias. In 90 patients with ischemic heart disease and treated with an ICD for primary or secondary prevention, the presence of inducible ischemia during dobutamine stress echocardiography was associated with 2-fold increased risk of death or appropriate ICD therapy at follow-up (95% CI, 1.2-3.5; P < 0.001).22 Revascularization of ischemic myocardium has demonstrated to reduce the risk of arrhythmic events.23
Nonischemic Cardiomyopathies
Reduction of LVEF in the absence of significant coronary artery disease, valvular heart disease, hypertension, or congenital heart disease, defines nonischemic cardiomyopathy, and can be caused by primary disorders of the myocardium or secondary to systemic diseases that cause myocardial damage.24 The most frequent form is dilated cardiomyopathy, with a yearly incidence of 0.57 cases/100,000 per year among children and 7 cases/100 000 per year among adults.24 Familial dilated cardiomyopathy may be observed in 20-48% and frequently has an autosomal dominant inheritance. Myocarditis, toxicity-related myocardial damage, metabolic disturbance storage diseases, and infiltrative diseases are other causes of nonischemic cardiomyopathy. Patients with nonischemic cardiomyopathy have an increased risk of ventricular arrhythmias and SCD, and the efficacy of ICD to improve long-term outcome in primary prevention has been shown in several randomized trials.25,26 Evaluation of arrhythmogenic substrate with CMR and echocardiography may refine risk stratification in patients with nonischemic cardiomyopathy. Replacement fibrosis assessed with LGE CMR and mechanical and electrical tissue heterogeneity using speckle tracking echocardiography have been associated with increased risk of ventricular arrhythmias and SCD (Table 2).27-42
The association between the presence of LGE (replacement fibrosis) and risk of SCD, aborted SCD, or appropriate ICD therapy for ventricular tachycardia was demonstrated in a recent meta-analysis of 7 studies including 1194 patients with nonischemic cardiomyopathy (odds ratio 5.32; 95% CI 3.45-8.2; P < 0.001).43 Each type of nonischemic cardiomyopathy may show a distinct spatial distribution of replacement fibrosis on LGE CMR (Figure 2). In dilated cardiomyopathy, 30% of patients may show septal mid-wall fibrosis.32 In myocarditis, LGE distribution is typically epicardial, particularly in the inferolateral wall or septum.35 Cardiac sarcoidosis and Anderson-Fabry’s disease typically show mid-wall LGE in the basal inferolateral segments, while in Duchenne muscular dystrophy, the distribution of LGE is typically subepicardial affecting the lateral segments.37-39 Diffuse and patchy distribution of LGE or more typically circumferential subendocardial distribution of LGE can be observed in cardiac amyloidosis.44 In contrast to ischemic cardiomyopathy, the different studies evaluating the role of LGE CMR for risk stratification of patients with nonischemic cardiomyopathy have focused mainly on the presence of LGE (Table 2).27-42 Furthermore, LGE CMR permits characterization of the border zone which may include isthmus sites of ventricular tachycardia in nonischemic cardiomyopathy patients.45
Patterns of late gadolinium contrast enhancement in nonischemic cardiomyopathies. Septal mid-wall late gadolinium enhancement (arrow) is typically observed in dilated cardiomyopathy (A). Mid-wall late gadolinium enhancement of the basal inferolateral wall (arrow) in a patient with cardiac sarcoidosis (B). Patchy mid-wall late gadolinium enhancement of the hypertrophic septum at the level of the right ventricular junction (arrow) is typical of hypertrophic cardiomyopathy (C). In cardiac amyloidosis (D), the pattern of late gadolinium enhancement is characterized by circumferential subendocardial distribution (arrows)
Few studies have associated echocardiographic global LV longitudinal strain and mechanical dispersion (as surrogates of myocardial fibrosis and slow conduction) with ventricular arrhythmias and SCD.41,42 In 100 patients with sarcoidosis who were followed-up during a median of 35 months, Joyce et al demonstrated that global LV longitudinal strain was independently associated with a 1.4-fold increased risk for the combined end point (all-cause mortality, heart failure hospitalization, device implantation, new arrhythmias, and development of cardiac sarcoidosis).41 In 94 patients with nonischemic dilated cardiomyopathy, Haugaa and colleagues demonstrated the prognostic value of global LV longitudinal strain and mechanical dispersion.42 During a median follow-up, 13% of patients presented with sustained ventricular tachycardia or cardiac arrest. Each 1% worsening in global LV longitudinal strain and each 10-ms increase in mechanical dispersion were both independently associated with a 1.2-fold increased risk of ventricular arrhythmias or cardiac arrest (P = 0.002 for both).42
Inheritable Arrhythmogenic Diseases
Hypertrophic cardiomyopathy is the most frequent genetic heart disease, usually caused by mutations of genes encoding sarcomeric proteins, transmitted with an autosomal dominant inheritance but with incomplete penetrance and variable expression.46,47 The diagnosis is based on the presence of abnormally increased LV wall thickness (≥15 mm) by any imaging modality not explained by loading conditions and in the absence of other diseases associated with LV hypertrophy (Figure 3).48 The arrhythmogenic substrate is characterized by myocyte disarray and myocardial fibrosis, while microvascular dysfunction, ischemia, and sympathetic innervation disturbances that may influence the arrhythmogenic substrate triggering the occurrence of ventricular arrhythmias. Nonsustained ventricular arrhythmias have been reported in 25% of patients during ambulatory electrocardiographic monitoring49 and the prevalence increases with LV wall thickness and the presence of replacement fibrosis on LGE CMR.50 The annual incidence of SCD is 0.8%, with the highest prevalence among young patients.51,52 The 2014 European Society of Cardiology guidelines on the diagnosis and management of patients with hypertrophic cardiomyopathy proposed an algorithm to calculate the risk of SCD.46 Maximum LV wall thickness, maximum LV outflow tract gradient (at rest and during Valsalva maneuvres) and left atrial size were included in the algorithm, and can be assessed with echocardiography. Cine CMR can also quantify LV wall thickness and left atrial dimensions; however, quantification of the LV outflow tract obstruction is not routinely assessed. Replacement fibrosis on LGE CMR has been described in 65% of patients (range 33-84%) and is typically distributed following a patchy mid-wall pattern in areas of hypertrophy and at the insertion points of the right ventricle (Figure 3).53 In a recent large registry including 1293 patients with hypertrophic cardiomyopathy, each 10% increase in LGE was independently associated with increased risk of SCD events (HR 1.46, 95% CI 1.12-1.92; P = 0.002).54 The addition of LGE to a SCD event risk model resulted in enhanced integrated discrimination improvement (56.5%) and net reclassification improvement (12.9%). A recent meta-analysis of 6 studies including 3067 patients with hypertrophic cardiomyopathy evaluated with LGE CMR (54% showing LGE) demonstrated that the incidence of SCD events was significantly increased among those patients with LGE compared with patients without (odds ratio 2.52, 95% CI 1.44-4.4; P = 0.001).55 However, meta-regression analysis showed that the extent of LGE was not significantly associated with SCD events risk (P = 0.35) probably due to the inclusion of 5 studies that included patients with a mean LGE extent <10%.54,56-59
Hypertrophic cardiomyopathy. Panel A shows left ventricular (LV) hypertrophy with >15 mm thickness of the septal and lateral walls. Panel B shows late gadolinium-enhanced cardiac magnetic resonance of a patient with hypertrophic cardiomyopathy and delayed enhancement in the septum, at the insertion of the right ventricle (arrow)
Speckle tracking echocardiographic LV strain analysis has demonstrated to correlate with the amount of replacement fibrosis in hypertrophic cardiomyopathy patients, and therefore it could be hypothesized that the assessment of LV strain may be also associated with increased risk of ventricular arrhythmias (Figure 4).60 In 92 hypertrophic cardiomyopathy patients undergoing ICD implantation, Debonnaire et al showed that global LV longitudinal strain measured with speckle tracking echocardiography was independently associated with occurrence of appropriate ICD therapy at follow-up (HR 1.15, 95% CI 1.02-1.3; P = 0.03).61
Risk stratification of patients with hypertrophic cardiomyopathy using two-dimensional speckle tracking echocardiography. Example of a patient with hypertrophic obstructive cardiomyopathy with asymmetric septal hypertrophy and systolic anterior motion of the mitral valve (A). On echocardiographic speckle tracking analysis, the magnitude of global left ventricular longitudinal strain (GLS) is −13.8% (B). The study by Debonnaire et al showed that patients with a left ventricular GLS ≥−14% had higher rates of appropriate implantable cardioverter defibrillator (ICD) therapy compared with patients with more preserved GLS (<−14%) (C). Reproduced with permission from Debonnaire et al.61
Arrhythmogenic right ventricular cardiomyopathy (ARVC) is also an autosomal dominant inheritance disease with variable penetrance and phenotype expression characterized by replacement of ventricular myocardium by fibrous and fatty tissue.62 Sustained monomorphic ventricular tachycardia with left bundle branch block morphology is the most frequent arrhythmia and is usually observed at advanced stages of the disease, whereas ventricular fibrillation may occur at any phase of the disease. The imaging criteria that suggest ARVC include right ventricular dilatation and regional right ventricular wall motion abnormalities (aneurysms).62 CMR is considered the reference standard for right ventricular volumes quantification and its high spatial resolution permits better identification of right ventricular aneurysms (Figure 5). Two-dimensional echocardiography provides several measurements to accurately estimate the RV dimensions, and with the use of intravenous contrast, the regional wall motion abnormalities can be better visualized. However, it has been shown that echocardiography had lower diagnostic performance compared with CMR.63 Although assessment of LGE with CMR in ARVC is challenging due to the thin right ventricular walls and the low specificity (as it can also be observed in other cardiomyopathies that resemble ARVC such as cardiac sarcoidosis), right ventricular LGE can be observed in 88% of patients.64 In a recent study including 69 patients with ARVC, the presence of abnormalities on CMR (right ventricular dilatation, wall motion abnormalities, LGE or LV, and biventricular involvement) was associated with development of ventricular arrhythmias; specifically, the presence of right ventricular LGE was only observed in patients presenting with arrhythmic events.65 Assessment of global LV longitudinal strain with speckle tracking echocardiography has demonstrated that LV involvement in ARVC patients demonstrated by impaired global LV longitudinal strain was independently associated with the occurrence of ventricular tachycardia, SCD, and appropriate ICD therapies.66 If confirmed in larger studies, the results may have important implications, since in many ARVC patients LV involvement occurs at a late stage of the disease, and earlier detection of LV dysfunction may identify the patients who may potentially benefit from an ICD.
Cardiac magnetic resonance in arrhythmogenic right ventricular cardiomyopathy. Example of a patient who presented with ventricular tachycardia. On cine cardiac magnetic resonance, the 4-chamber view shows a dilated right ventricle, with depressed ejection fraction (35%) and areas of dyskinesia (arrow, A). On late gadolinium contrast-enhanced cardiac magnetic resonance, the areas with dyskinesia show hyperenhancement (arrow, B)
Finally, primary electric disorders or channelopathies, such as long QT syndrome, Wolff-Parkinson-White syndrome or Brugada syndrome are characterized by preserved LVEF without structural abnormalities. The prolongation of the action potential and repolarization that occur in these disorders may increase the risk of afterdepolarizations and polymorphic ventricular arrhythmias. Speckle tracking echocardiography has demonstrated to identify mechanical disturbances as a consequence of the electric derangements.67 Particularly, in long QT syndrome, LV mechanical dispersion (calculated as the differences in time to regional peak strain measured in the sub- and the midmyocardium) was longer in symptomatic patients compared with asymptomatic carriers (45 ± 13 ms vs 27 ± 12 ms and 46 ± 22 ms vs 26 ± 21 ms, respectively; P < 0.001 for both).67 There is limited literature on the role of CMR in this patient group. In a cohort of 81 patients with genetically positive Brugada syndrome, CMR demonstrated changes in RV ejection fraction and volumes compared to patients without the mutation.68
New Knowledge Gained
Left ventricular ejection fraction assessed with any imaging technique remains as an important criterion to identify the patients at risk of having ventricular arrhythmias or SCD.3 However, a significant proportion of patients with reduced LVEF who receive an ICD for primary prevention may not experience an appropriate therapy. In contrast, patients with relatively preserved LVEF or patients without structural heart disease and normal LVEF may experience life-threatening arrhythmias. Advanced echocardiographic imaging techniques evaluating the active deformation of the myocardium provided the incremental value over LVEF for risk stratification in a variety of patients with cardiac disease. Cardiac magnetic resonance and particularly, the use of LGE have provided further characterization of the arrhythmogenic substrate with important prognostic and therapeutic implications. Current guidelines support the role of these imaging techniques to accurately assess patients at risk of SCD.
Abbreviations
- ARVC:
-
Arrhythmogenic right ventricular cardiomyopathy
- CI:
-
Confidence interval
- CMR:
-
Cardiac magnetic resonance
- GLS:
-
Global longitudinal strain
- HR:
-
Hazard ratio
- ICD:
-
Implantable cardioverter defibrillator
- LGE:
-
Late gadolinium enhancement
- LV:
-
Left ventricular
- LVEF:
-
Left ventricular ejection fraction
- SCD:
-
Sudden cardiac death
References
Myerburg RJ, Kessler KM, Castellanos A. Sudden cardiac death. Structure, function, and time-dependence of risk. Circulation 1992;85:I2–10.
Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren M, et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Eur Heart J 2012;2012(33):1635–701.
Priori SG, Blomstrom-Lundqvist C, Mazzanti A, Blom N, Borggrefe M, Camm J, et al. 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC)Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J 2015;36:2793–867.
Moss AJ, Greenberg H, Case RB, Zareba W, Hall WJ, Brown MW, et al. Long-term clinical course of patients after termination of ventricular tachyarrhythmia by an implanted defibrillator. Circulation 2004;110:3760–5.
Ersboll M, Valeur N, Andersen MJ, Mogensen UM, Vinther M, Svendsen JH, et al. Early echocardiographic deformation analysis for the prediction of sudden cardiac death and life-threatening arrhythmias after myocardial infarction. JACC Cardiovasc Imaging 2013;6:851–60.
Haugaa KH, Grenne BL, Eek CH, Ersboll M, Valeur N, Svendsen JH, et al. Strain echocardiography improves risk prediction of ventricular arrhythmias after myocardial infarction. JACC Cardiovasc Imaging 2013;6:841–50.
Leong DP, Hoogslag GE, Piers SR, Hoke U, Thijssen J, Marsan NA, et al. The relationship between time from myocardial infarction, left ventricular dyssynchrony, and the risk for ventricular arrhythmia: Speckle-tracking echocardiographic analysis. J Am Soc Echocardiogr 2015;28:470–7.
Ng AC, Bertini M, Borleffs CJ, Delgado V, Boersma E, Piers SR, et al. Predictors of death and occurrence of appropriate implantable defibrillator therapies in patients with ischemic cardiomyopathy. Am J Cardiol 2010;106:1566–73.
Bertini M, Schalij MJ, Bax JJ, Delgado V. Emerging role of multimodality imaging to evaluate patients at risk for sudden cardiac death. Circ Cardiovasc Imaging 2012;5(4):525–35.
Bello D, Fieno DS, Kim RJ, Pereles FS, Passman R, Song G, et al. Infarct morphology identifies patients with substrate for sustained ventricular tachycardia. J Am Coll Cardiol 2005;45:1104–8.
Boye P, Abdel-Aty H, Zacharzowsky U, Bohl S, Schwenke C, van der Geest RJ, et al. Prediction of life-threatening arrhythmic events in patients with chronic myocardial infarction by contrast-enhanced CMR. JACC Cardiovasc Imaging 2011;4:871–9.
Lee DC, Goldberger JJ. CMR for sudden cardiac death risk stratification: Are we there yet? JACC Cardiovasc Imaging 2013;6:345–8.
Roes SD, Borleffs CJ, van der Geest RJ, Westenberg JJ, Marsan NA, Kaandorp TA, et al. Infarct tissue heterogeneity assessed with contrast-enhanced MRI predicts spontaneous ventricular arrhythmia in patients with ischemic cardiomyopathy and implantable cardioverter-defibrillator. Circ Cardiovasc Imaging 2009;2:183–90.
Schmidt A, Azevedo CF, Cheng A, Gupta SN, Bluemke DA, Foo TK, et al. Infarct tissue heterogeneity by magnetic resonance imaging identifies enhanced cardiac arrhythmia susceptibility in patients with left ventricular dysfunction. Circulation 2007;115:2006–14.
Scott PA, Morgan JM, Carroll N, Murday DC, Roberts PR, Peebles CR, et al. The extent of left ventricular scar quantified by late gadolinium enhancement MRI is associated with spontaneous ventricular arrhythmias in patients with coronary artery disease and implantable cardioverter-defibrillators. Circ Arrhythm Electrophysiol 2011;4:324–30.
Fernandez-Armenta J, Berruezo A, Andreu D, Camara O, Silva E, Serra L, et al. Three-dimensional architecture of scar and conducting channels based on high resolution ce-CMR: Insights for ventricular tachycardia ablation. Circ Arrhythm Electrophysiol 2013;6:528–37.
Perez-David E, Arenal A, Rubio-Guivernau JL, del Castillo R, Atea L, Arbelo E, et al. Noninvasive identification of ventricular tachycardia-related conducting channels using contrast-enhanced magnetic resonance imaging in patients with chronic myocardial infarction: Comparison of signal intensity scar mapping and endocardial voltage mapping. J Am Coll Cardiol 2011;57:184–94.
Cokic I, Kali A, Yang HJ, Yee R, Tang R, Tighiouart M et al (2015) Iron-sensitive cardiac magnetic resonance imaging for prediction of ventricular arrhythmia risk in patients with chronic myocardial infarction: Early evidence. Circ Cardiovasc Imaging p 8 (in press).
Steel K, Broderick R, Gandla V, Larose E, Resnic F, Jerosch-Herold M, et al. Complementary prognostic values of stress myocardial perfusion and late gadolinium enhancement imaging by cardiac magnetic resonance in patients with known or suspected coronary artery disease. Circulation 2009;120:1390–400.
Kali A, Kumar A, Cokic I, Tang RL, Tsaftaris SA, Friedrich MG, et al. Chronic manifestation of postreperfusion intramyocardial hemorrhage as regional iron deposition: a cardiovascular magnetic resonance study with ex vivo validation. Circ Cardiovasc Imaging 2013;6:218–28.
Geyer H, Caracciolo G, Abe H, Wilansky S, Carerj S, Gentile F, et al. Assessment of myocardial mechanics using speckle tracking echocardiography: Fundamentals and clinical applications. J Am Soc Echocardiogr 2010;23:351–69.
Elhendy A, Chapman S, Porter TR, Windle J. Association of myocardial ischemia with mortality and implantable cardioverter-defibrillator therapy in patients with coronary artery disease at risk of arrhythmic death. J Am Coll Cardiol 2005;46:1721–6.
van der Burg AE, Bax JJ, Boersma E, Pauwels EK, van der Wall EE, Schalij MJ. Impact of viability, ischemia, scar tissue, and revascularization on outcome after aborted sudden death. Circulation 2003;108:1954–9.
Jefferies JL, Towbin JA. Dilated cardiomyopathy. Lancet 2010;375:752–62.
Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med 2005;352:225–37.
Kadish A, Dyer A, Daubert JP, Quigg R, Estes NA, Anderson KP, et al. Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N Engl J Med 2004;350:2151–8.
Wu KC, Weiss RG, Thiemann DR, Kitagawa K, Schmidt A, Dalal D, et al. Late gadolinium enhancement by cardiovascular magnetic resonance heralds an adverse prognosis in nonischemic cardiomyopathy. J Am Coll Cardiol 2008;51:2414–21.
Iles L, Pfluger H, Lefkovits L, Butler MJ, Kistler PM, Kaye DM, et al. Myocardial fibrosis predicts appropriate device therapy in patients with implantable cardioverter-defibrillators for primary prevention of sudden cardiac death. J Am Coll Cardiol 2011;57:821–8.
Lehrke S, Lossnitzer D, Schob M, Steen H, Merten C, Kemmling H, et al. Use of cardiovascular magnetic resonance for risk stratification in chronic heart failure: Prognostic value of late gadolinium enhancement in patients with non-ischaemic dilated cardiomyopathy. Heart 2011;97:727–32.
Gao P, Yee R, Gula L, Krahn AD, Skanes A, Leong-Sit P, et al. Prediction of arrhythmic events in ischemic and dilated cardiomyopathy patients referred for implantable cardiac defibrillator: evaluation of multiple scar quantification measures for late gadolinium enhancement magnetic resonance imaging. Circ Cardiovasc Imaging 2012;5:448–56.
Muller KA, Muller I, Kramer U, Kandolf R, Gawaz M, Bauer A, et al. Prognostic value of contrast-enhanced cardiac magnetic resonance imaging in patients with newly diagnosed non-ischemic cardiomyopathy: Cohort study. PLoS One 2013;8:e57077.
Gulati A, Jabbour A, Ismail TF, Guha K, Khwaja J, Raza S, et al. Association of fibrosis with mortality and sudden cardiac death in patients with nonischemic dilated cardiomyopathy. JAMA 2013;309:896–908.
Neilan TG, Coelho-Filho OR, Danik SB, Shah RV, Dodson JA, Verdini DJ, et al. CMR quantification of myocardial scar provides additive prognostic information in nonischemic cardiomyopathy. JACC Cardiovasc Imaging 2013;6:944–54.
Masci PG, Doulaptsis C, Bertella E, Del Torto A, Symons R, Pontone G, et al. Incremental prognostic value of myocardial fibrosis in patients with non-ischemic cardiomyopathy without congestive heart failure. Circ Heart Fail 2014;7:448–56.
Grun S, Schumm J, Greulich S, Wagner A, Schneider S, Bruder O, et al. Long-term follow-up of biopsy-proven viral myocarditis: Predictors of mortality and incomplete recovery. J Am Coll Cardiol 2012;59:1604–15.
Mello RP, Szarf G, Schvartzman PR, Nakano EM, Espinosa MM, Szejnfeld D, et al. Delayed enhancement cardiac magnetic resonance imaging can identify the risk for ventricular tachycardia in chronic Chagas’ heart disease. Arq Bras Cardiol 2012;98:421–30.
Kramer J, Niemann M, Stork S, Frantz S, Beer M, Ertl G, et al. Relation of burden of myocardial fibrosis to malignant ventricular arrhythmias and outcomes in Fabry disease. Am J Cardiol 2014;114:895–900.
Florian A, Ludwig A, Engelen M, Waltenberger J, Rosch S, Sechtem U, et al. Left ventricular systolic function and the pattern of late-gadolinium-enhancement independently and additively predict adverse cardiac events in muscular dystrophy patients. J Cardiovasc Magn Reson 2014;16:81.
Greulich S, Deluigi CC, Gloekler S, Wahl A, Zurn C, Kramer U, et al. CMR imaging predicts death and other adverse events in suspected cardiac sarcoidosis. JACC Cardiovasc Imaging 2013;6:501–11.
Murtagh G, Laffin LJ, Beshai JF, Maffessanti F, Bonham CA, Patel AV, et al. Prognosis of myocardial damage in sarcoidosis patients with preserved left ventricular ejection fraction: Risk stratification using cardiovascular magnetic resonance. Circ Cardiovasc Imaging 2016;9:e003738.
Joyce E, Ninaber MK, Katsanos S, Debonnaire P, Kamperidis V, Bax JJ, et al. Subclinical left ventricular dysfunction by echocardiographic speckle-tracking strain analysis relates to outcome in sarcoidosis. Eur J Heart Fail 2015;17:51–62.
Haugaa KH, Goebel B, Dahlslett T, Meyer K, Jung C, Lauten A, et al. Risk assessment of ventricular arrhythmias in patients with nonischemic dilated cardiomyopathy by strain echocardiography. J Am Soc Echocardiogr 2012;25:667–73.
Kuruvilla S, Adenaw N, Katwal AB, Lipinski MJ, Kramer CM, Salerno M. Late gadolinium enhancement on cardiac magnetic resonance predicts adverse cardiovascular outcomes in nonischemic cardiomyopathy: A systematic review and meta-analysis. Circ Cardiovasc Imaging 2014;7:250–8.
Fontana M, Pica S, Reant P, Abdel-Gadir A, Treibel TA, Banypersad SM, et al. Prognostic value of late gadolinium enhancement cardiovascular magnetic resonance in cardiac amyloidosis. Circulation 2015;132:1570–9.
Piers SR, Tao Q, de Riva SM, Siebelink HM, Schalij MJ, van der Geest RJ, et al. CMR-based identification of critical isthmus sites of ischemic and nonischemic ventricular tachycardia. JACC Cardiovasc Imaging 2014;7:774–84.
Elliott PM, Anastasakis A, Borger MA, Borggrefe M, Cecchi F, Charron P, et al. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: The Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J 2014;35:2733–79.
Gersh BJ, Maron BJ, Bonow RO, Dearani JA, Fifer MA, Link MS, et al. 2011 ACCF/AHA guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2011;124:e783–831.
Cardim N, Galderisi M, Edvardsen T, Plein S, Popescu BA, D’Andrea A, et al. Role of multimodality cardiac imaging in the management of patients with hypertrophic cardiomyopathy: an expert consensus of the European Association of Cardiovascular Imaging Endorsed by the Saudi Heart Association. Eur Heart J Cardiovasc Imaging 2015;16:280.
Monserrat L, Elliott PM, Gimeno JR, Sharma S, Penas-Lado M, McKenna WJ. Non-sustained ventricular tachycardia in hypertrophic cardiomyopathy: an independent marker of sudden death risk in young patients. J Am Coll Cardiol 2003;42:873–9.
O’Hanlon R, Grasso A, Roughton M, Moon JC, Clark S, Wage R, et al. Prognostic significance of myocardial fibrosis in hypertrophic cardiomyopathy. J Am Coll Cardiol 2010;56:867–74.
Maron BJ, Spirito P, Shen WK, Haas TS, Formisano F, Link MS, et al. Implantable cardioverter-defibrillators and prevention of sudden cardiac death in hypertrophic cardiomyopathy. JAMA 2007;298:405–12.
O’Mahony C, Elliott PM. Prevention of sudden cardiac death in hypertrophic cardiomyopathy. Heart 2014;100:254–60.
Rudolph A, Abdel-Aty H, Bohl S, Boye P, Zagrosek A, Dietz R, et al. Noninvasive detection of fibrosis applying contrast-enhanced cardiac magnetic resonance in different forms of left ventricular hypertrophy relation to remodeling. J Am Coll Cardiol 2009;53:284–91.
Chan RH, Maron BJ, Olivotto I, Pencina MJ, Assenza GE, Haas T, et al. Prognostic value of quantitative contrast-enhanced cardiovascular magnetic resonance for the evaluation of sudden death risk in patients with hypertrophic cardiomyopathy. Circulation 2014;130:484–95.
Briasoulis A, Mallikethi-Reddy S, Palla M, Alesh I, Afonso L. Myocardial fibrosis on cardiac magnetic resonance and cardiac outcomes in hypertrophic cardiomyopathy: A meta-analysis. Heart 2015;101:1406–11.
Bruder O, Wagner A, Jensen CJ, Schneider S, Ong P, Kispert EM, et al. Myocardial scar visualized by cardiovascular magnetic resonance imaging predicts major adverse events in patients with hypertrophic cardiomyopathy. J Am Coll Cardiol 2010;56:875–87.
Ismail TF, Jabbour A, Gulati A, Mallorie A, Raza S, Cowling TE, et al. Role of late gadolinium enhancement cardiovascular magnetic resonance in the risk stratification of hypertrophic cardiomyopathy. Heart 2014;100:1851–8.
Maron MS, Appelbaum E, Harrigan CJ, Buros J, Gibson CM, Hanna C, et al. Clinical profile and significance of delayed enhancement in hypertrophic cardiomyopathy. Circ Heart Fail 2008;1:184–91.
Rubinshtein R, Glockner JF, Ommen SR, Araoz PA, Ackerman MJ, Sorajja P, et al. Characteristics and clinical significance of late gadolinium enhancement by contrast-enhanced magnetic resonance imaging in patients with hypertrophic cardiomyopathy. Circ Heart Fail 2010;3:51–8.
Almaas VM, Haugaa KH, Strom EH, Scott H, Smith HJ, Dahl CP, et al. Noninvasive assessment of myocardial fibrosis in patients with obstructive hypertrophic cardiomyopathy. Heart 2014;100(8):631–8.
Debonnaire P, Thijssen J, Leong DP, Joyce E, Katsanos S, Hoogslag GE, et al. Global longitudinal strain and left atrial volume index improve prediction of appropriate implantable cardioverter defibrillator therapy in hypertrophic cardiomyopathy patients. Int J Cardiovasc Imaging 2014;30:549–58.
Marcus FI, McKenna WJ, Sherrill D, Basso C, Bauce B, Bluemke DA, et al. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the task force criteria. Circulation 2010;121:1533–41.
Borgquist R, Haugaa KH, Gilljam T, Bundgaard H, Hansen J, Eschen O, et al. The diagnostic performance of imaging methods in ARVC using the 2010 Task Force criteria. Eur Heart J Cardiovasc Imaging 2014;15:1219–25.
te Riele AS, Tandri H, Bluemke DA. Arrhythmogenic right ventricular cardiomyopathy (ARVC): cardiovascular magnetic resonance update. J Cardiovasc Magn Reson 2014;16:50.
te Riele AS, Bhonsale A, James CA, Rastegar N, Murray B, Burt JR, et al. Incremental value of cardiac magnetic resonance imaging in arrhythmic risk stratification of arrhythmogenic right ventricular dysplasia/cardiomyopathy-associated desmosomal mutation carriers. J Am Coll Cardiol 2013;62:1761–9.
Mast TP, Teske AJ, vd Heijden JF, Groeneweg JA, te Riele AS, Velthuis BK, et al. Left ventricular involvement in arrhythmogenic right ventricular dysplasia/cardiomyopathy assessed by echocardiography predicts adverse clinical outcome. J Am Soc Echocardiogr 2015;28:1103–13.
Haugaa KH, Amlie JP, Berge KE, Leren TP, Smiseth OA, Edvardsen T. Transmural differences in myocardial contraction in long-QT syndrome: mechanical consequences of ion channel dysfunction. Circulation 2010;122:1355–63.
Rudic B, Schimpf R, Veltmann C, Doesch C, Tülümen E, Schoenberg SO, et al. Brugada syndrome: clinical presentation and genotype—correlation with magnetic resonance imaging parameters. Europace 2015. doi:10.1093/europace/euv300.
Disclosure
The Department of Cardiology received research grants from Biotronik, Edwards Lifesciences, Medtronic, Boston Scientific. Victoria Delgado received speaker fees from Abbott Vascular.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Delgado, V., Bucciarelli-Ducci, C. & Bax, J.J. Diagnostic and prognostic roles of echocardiography and cardiac magnetic resonance. J. Nucl. Cardiol. 23, 1399–1410 (2016). https://doi.org/10.1007/s12350-016-0595-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-016-0595-z