Abstract
With the rapid growth of molecular biology, in vivo imaging of such molecular process (i.e., molecular imaging) has been well developed. The molecular imaging has been focused on justifying advanced treatments and for assessing the treatment effects. Most of molecular imaging has been developed using PET camera and suitable PET radiopharmaceuticals. However, this technique cannot be widely available and we need alternative approach. 123I-labeled compounds have been also suitable for molecular imaging using single-photon computed tomography (SPECT) 123I-labeled meta-iodobenzylguanidine (MIBG) has been used for assessing severity of heart failure and prognosis. In addition, it has a potential role to predict fatal arrhythmia, particularly for those who had and are planned to receive implantable cardioverter-defibrillator treatment. 123I-beta-methyl-iodophenylpentadecanoic acid (BMIPP) plays an important role for identifying ischemia at rest, based on the unique capability to represent persistent metabolic alteration after recovery of ischemia, so called ischemic memory. Since BMIPP abnormalities may represent severe ischemia or jeopardized myocardium, it may permit risk analysis in CAD patients, particularly for those with chronic kidney disease and/or hemodialysis patients. This review will discuss about recent development of these important iodinated compounds.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Molecular cardiovascular imaging has an important role for imaging cardiovascular disorders in molecular and cellular levels in vivo. This technique has a potential to assess severity of myocardial disorders such as heart failure (HF), severe coronary artery disease (CAD), and various types of cardiomyopathy. Molecular imaging has possibilities in monitoring treatments, and prediction of suitable treatment. Thus, molecular imaging is expected for clinical use for making treatment strategy in various cardiovascular disorders.1
Cardiac PET is a powerful, quantitative imaging modality which has been most extensively used to investigate cardiaovascular biology and physiology.2,3 On the other hand, various 123I-labeled compounds have been introduced for molecular imaging in most of clinical centers using conventional gamma cameras without need of cyclotron. Longer half life of 123I (13 hours) is suitable for delivering long distance from 123I supply centers. Japan has extensive clinical experiences with two major iodinated compounds: 123I-meta-iodobenzylguanidine (MIBG) and 123I-15-(p-iodophenyl)-3R,S-methyl pentadecanoic acid (BMIPP). This article will review the clinical values of these novel tracers, including most recent topics, such as predicting fatal arrhythmias by MIBG and silent ischemia in chronic kidney disease (CKD) by BMIPP.
MIBG Imaging
MIBG, a presynaptic imaging agent, is norepinephrine analog which is concentrated and stored in the myocardium in a similar fashion as norepinephrine.4 Its uptake is primarily through the energy requiring, high affinity, low capacity, “uptake 1” norepinephrine transporter mechanism.5,6 MIBG is washed out from the myocardium, but in contrast to norepinephrine, it is not catabolized by monamine oxidase or catechol-O-methyl transferase (COMT). Thus, the assessment of MIBG uptake and washout allows the unique characterization of sympathetic aspect of autonomic cardiac function.
Patients are usually instructed overnight fast prior to MIBG studies. Following intravenous administration of 111-370 MBq (3-10 mCi) of MIBG, anterior planar imaging and single-photon computed tomography (SPECT) are acquired at 30 minutes (early phase) and 4 hours (delayed phase). In order to minimize scatter noise from high-energy photons from 123I, medium-energy collimators or 123I collimators are preferred to the conventional low-energy collimators.7,8 The most common semiquantitative parameter is the heart to mediastinal count ratio (HMR) calculated from the mean count of the whole heart and upper third of the mediastinum in planar anterior view. In addition, the washout rate (WR) was also calculated as the following equation:
where each heart counts should be calculated after background subtraction.
The MIBG HMR as a marker of tracer retention in the myocardium has been found to be specific to sympathetic nerve terminals, whereas the MIBG HR between the early and the delayed images may represent a parameter of neurohormonal function. For assessing regional as well as global neuronal function, SPECT imaging can be analyzed for regional MIBG distribution and also defect score may be estimated as another semiquantitative parameter. A normal data base recently acquired by multicenter study from Japan may help precise assessment of SPECT distribution.9
MIBG in HF
HF is a major cause of mortality and represents a growing health problem.10,11 While severity of HF is evaluated mainly from symptoms, clinical findings, hemodynamic measurements, left ventricular ejection fraction (LVEF), or exercise tolerance, the assessment of neurohormonal system abnormalities related to HF has proven to be valuable for risk stratification.12-15 Despite these indices, the accurate evaluation of the cardiovascular risk remains difficult. An increase in presynaptic activity with a decrease of postsynaptic beta-adrenergic receptor density is well reported in failing heart.12,15-19
Because MIBG is an NE analog, WR and delayed HMR may directly reflect NE release from the nerve terminal and its reuptake into the nerve terminal (uptake-1). In addition, the MIBG WR may reflect presynaptic sympathetic tone. The local NE concentration in the synaptic cleft increases when WR increases or HMR decreases.20-22 MIBG imaging has been widely used for the assessment of cardiac sympathetic function in HF21-26 (Figure 1).
Merlet et al27 first showed the prognostic value of HMR in patients with HF, although washout kinetics of MIBG was not assessed in this study. Thereafter many prognostic studies using this imaging technique have been performed in European countries and Japan. In many studies, it has been reported that impaired cardiac adrenergic innervation as assessed by MIBG imaging was closely associated with mortality in patients with HF.27-36 Tamaki et al37,38 from Osaka showed the MIBG value for predicting sudden cardiac death in comparison with ECG parameters, such as T wave alteration. They found that MIBG WR was independent of LVEF for risk analysis in patients with HF. A multivariate Cox analysis suggested that MIBG WR and LVEF but not ECG parameters were significant and independent predictors for sudden cardiac death.
Verberne et al39 recently reported a meta-analysis of MIBG imaging in HF. They concluded that decreased late HMR and increased WR of MIBG indicated a poor prognosis. Although their conclusion was nearly consistent with the previous reports, HMR showed significant heterogeneity as compared to the consistent findings on WR analysis of MIBG for prognostic assessment. Heterogenic result of HMR may partly be due to differences in a specific activity of MIBG, clinical backgrounds among countries, cumulative death calculation, and various endpoints used. In addition, a different gamma camera with collimators with variable method for in estimation of count density in the myocardium and background activity may possibly cause heterogenous results in multicenter comparison. In this respect, standardization of MIBG image acquisitions and quantitative analysis with their validation should be established. This standardization is especially important for multicenter studies.40
There are some reports indicating MIBG imaging as a good predictor of response to beta adrenergic blocker therapy.41,42 Both studies suggested that relatively preserved uptake may represent a good responder, whereas severely decreased MIBG uptake was associated with a poor response sign for beta-blocker therapy. Altered adrenergic presynaptic function may cause postsynaptic receptor dysfunction. Spyrou et al43 reported that beta-adrenergic receptor down-regulation can be used as a predictor of LV remodeling in patients after acute myocardial infarction. We recently demonstrated that myocardial beta-adrenergic receptor down-regulation estimated by 11CGP-12177 PET may be related with increased sympathetic tone, shown as increased MIBG WR.19 Furthermore, beta-adrenergic receptor down-regulation may predict improvement of cardiac function after beta-blocker treatment in patients with dilated cardiomyopathy.44 Although this remains preliminary, adrenergic functional study may contribute to predict which patients may receive most benefit in patients with severe HF.
MIBG for Predicting Fatal Arrhythmias
Sudden cardiac death due to fatal arrhythmia represents an important health care problem in many countries. A number of efforts have been done to develop suitable therapeutic options, implantable cardioverter-defibrillator (ICD) treatment has been well established for preventive use in patients with high risk for arrhythmic death.45,46 Despite clear indication for ICD treatment, only minority of the patients actually received this treatment.47 On the contrary, widespread use of ICD therapy has increased medical cost and unfavorable side effects especially for those at lower risk for sudden cardiac death. While general criteria for ICD therapy is defined, but has been frequently modified since the current criteria remain unsatisfactory.48-50
Autonomic dysfunction assessed by MIBG is thought to play an important role in the detection of high risk ventricular arrhythmia.51-53 Particularly, MIBG may identify the areas of denervation hypersensitivity which may likely to cause ventricular arrhythmias. There are a number of pilot studies indicated MIBG as a potential predictor for ventricular arrhythmias in patients with ICD.54-56
Jacobson et al57 report the results of a prospective MIBG imaging trial of 961 patients with HF recruited at 96 sites in North America and Europe, ADMIRE-HF. Patients with New York Heart Association (NYHA) Class II and III HF and LVEF ≤ 35% were enrolled. They concluded that HMR of <1.6 measured at 4 hours after MIBG administration provided prognostic data beyond that available from LVEF, BNP assay, and NYHA class at the time of enrollment. This important study indicates adrenergic neuronal functional parameter obtained by MIBG scan as an important and independent parameter for predicting sudden death from the commonly used LV functional parameters. For patients who make criteria for ICD but are ambivalent, it provides yet another means of assessing overall risk of events to guide clinical decisions.58
Recently, Boogers et al59 reported the value of MIBG imaging in 116 patients with HF who may have a candidate for ICD treatment. They showed that the MIBG defect size on delayed SPECT imaging can predict ventricular arrhythmias causing appropriate ICD discharge as a primary end point as well as the composite of appropriate ICD therapy or cardiac death as secondary end point. They also concluded that MIBG SPECT may improve risk stratification for arrhythmic death in patients who have an indication for ICD treatment. One of the new findings is that they used different criteria (denervation as a MIBG defect size) from the previous reports (mostly HMR as global MIBG uptake and/or WR). Since MIBG uptake is generally decreased in many patients with HF, it is often difficult to reconstruct SPECT images, particularly in those showing severity decreased MIBG uptake. In addition, it may be quite unreliable to estimate defects score in such cases as compared to high myocardial uptake. It would be better to analyze innervation/perfusion mismatch on SPECT using two different radiotracers rather than MIBG SPECT alone. A standardized criteria showing decreased MIBG uptake or MIBG defect may be required in the future.
Another recent report by Nishisato et al60 included prospective study of MIBG imaging in combination with resting myocardial perfusion imaging in patients who received ICD treatment. During the mean follow-up of 29 months, ICD shocks (discharge) were documented in 30 of the total of 60 patients (50%). Among various clinical and scintigraphic variables, both lower HMR on MIBG and large perfusion defect were the most powerful predictors for ICD discharge on Cox multivariate analysis. This is the first report indicating incremental benefit in combined assessment of myocardial perfusion and sympathetic nerve function for appropriate risk stratification of patients who may need prophylactic ICD therapy. This result indicates both denervation and myocardial scar were important predictors for ICD discharge and fatal arrhythmias. But it remains unknown whether a simple perfusion imaging is enough or both MIBG and perfusion imaging may be required for prediction of such fatal arrhythmias. Another important issue is whether global assessment using MIBG kinetics or regional assessment of neuronal function using precise MIBG SPECT analysis may be required for prediction of fatal arrhythmias in HF patients. Further study with larger patients is required to confirm this preliminary result for cardiologists to use MIBG for selecting appropriate ICD treatment.
BMIPP Imaging
15-(p-Iodophenyl)-3R,S-methyl pentadecanoic acid (BMIPP) is one of iodinated branch-chain fatty acids introduced by Knapp et al.61 Because of high uptake and long retention in the myocardium, BMIPP is particularly useful for SPECT imaging with a conventional gamma camera. The unique and desirable properties of methyl-branched fatty acids are due to the inhibition of beta-oxidation by the presence of a methyl group in the beta-position.
Animal experiments have demonstrated that the clearance of BMIPP from the myocardium is slow with approximately 25% clearance in 2 hours.61 The fractional distribution of these compounds at 30 minutes after tracer injection in rats showed that 65-80% of the total activity resided in the triglyceride pool.
BMIPP was usually injected under fasting condition and SPECT imaging was obtained about 15-30 minutes after intravenous administration of 111-148 MBq (3-4 mCi) of BMIPP. BMIPP has been most widely used over 10 years in Japan.62-64
In general, BMIPP uptake was similar to regional perfusion seen on thallium-201 or technetium-99m perfusion agents. In the areas with perfusion abnormalities, BMIPP uptake is also decreased. But the discrepancy of perfusion and metabolism is often observed under various circumstances, including myocardial ischemia.56-58 In order to identify the perfusion-metabolism mismatch, regional BMIPP uptake is often compared with regional perfusion.
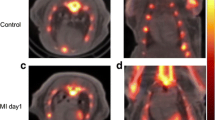
BMIPP for Identifying Ischemia
Ischemia may cause reduction of fatty acid utilization and shift from fatty acid to glucose utilization. In addition, such metabolic shift may persist shortly after recovery of ischemia. Thus, BMIPP uptake is often seen in ischemic myocardium, mainly due to persistent suppression of fatty acid metabolism after severe ischemia. This metabolic alteration as a result of prior ischemia is so called as ischemic memory (Figure 2).63-65 Such ischemic memory imaging may be used with BMIPP, since reduction of BMIPP uptake may identify prior ischemic insult after recovery of perfusion. A number of reports have indicated that BMIPP imaging at rest can be used for identifying ischemic myocardium in coronary patients without evidence of myocardial infarction66-73 (Figure 2). Recent meta-analysis from MEDLINE search of the published literature confirmed that BMIPP SPECT at rest exhibited a moderate sensitivity and high specificity to detect CAD lesions with a high prevalence of CAD.74 They concluded BMIPP may be of great value for patients with acute chest pain and those with relatively contraindications to exercise or pharmacologic stress myocardial perfusion imaging. The important point is that all these results were obtained with BMIPP imaging at rest, not under stress imaging to identify myocardial ischemia. When the BMIPP imaging was compared with stress myocardial perfusion imaging for the same patients suspected with CAD, the diagnostic accuracy was similar or slightly less than those of stress myocardial perfusion imaging.75 BMIPP abnormalities tended to be associated with unstable angina, regional wall motion abnormalities, and ECG changes, reflecting severe ischemia.69,75
A A series of short axis slices of resting perfusion (top), pharmacological stress perfusion (middle), and resting BMIPP (bottom) in a 55-year-old patient with coronary artery disease. While mild stress-induced ischemia is seen in inferior regions, a greater decrease in BMIPP uptake at rest is noted in inferior and lateral regions. B Right coronary arteriogram of the same patient shows a severe stenosis on proximal portion of the right coronary artery (arrow)
One of the major applications of BMIPP is to accurate diagnosis of acute coronary syndrome in emergency unit. We applied both BMIPP and myocardial perfusion imaging performed at rest for 111 consecutive patients with acute chest pain.72 All of them received coronary angiography to confirm the radionuclide findings. BMIPP imaging acquired within 48 hours after the last chest pain showed sensitivity of 74% and specificity of 92% doe identifying coronary stenosis, which was better than the resting myocardial perfusion imaging taken within 24 hours after the chest pain. This is the first report showing the value of BMIPP for identifying prior ischemic insult after recovery of chest pain in emergency department. In addition, altered BMIPP uptake was seen in many patients having coronary spasm. This finding has recently been confirmed by multicenter study in United States.76,77 They concluded that BMIPP SPECT in emergency department had similar sensitivity for detection patients with acute coronary syndrome with other contemporary imaging modalities. But BMIPP has a unique property of maintaining sensitivity even when performed up to 30 hours after symptom resolution.
Since less BMIPP uptake than perfusion may represent ischemic and jeopardized myocardium, the combined imaging with BMIPP and perfusion imaging may hold a prognostic value for identifying high-risk subgroups among patients with CAD.78-81 Such prognostic studies have been extended to angina patients without prior myocardial infarction.82,83 When 167 consecutive patients with angina were followed-up for 48 months, BMIPP defect score at rest, stress perfusion score, diabetes, and LVEF were independent predictors on the multivariate Cox’s analysis.82 No hard event was observed with normal BMIPP uptake, whereas two patients with nearly normal stress perfusion with abnormal BMIPP uptake had hard cardiac events. These preliminary reports may indicate a decrease in BMIPP uptake as an important prognostic indicator independent of stress induced ischemia on myocardial perfusion imaging in patients with angina without prior myocardial infarction. A recent systemic review of current literature suggested that an abnormal finding on BMIPP imaging was significantly associated with future cardiovascular outcomes across the spectrum of CAD.84 Thus, BMIPP imaging at rest may be useful for risk stratification of patients with CAD, particularly those with acute chest pain. A large prospective randomized control trial is warranted to confirm the prognostic value of BMIPP imaging for CAD patients.
BMIPP in CKD
CAD is often accompanied with CKD. Of particular, CAD may be the main cause of deaths in patients with end-stage renal disease (ESRD) who undergo renal replacement therapy. The incidence of cardiac death is higher among patients on hemodialysis when compared with the general population. This is probably due to the high prevalence of either underlying obstructive CAD or cardiovascular risk factors in those with ESRD.85-87 Insulin resistance is a common feature of patients with ESRD,88 it is linked with vascular endothelial dysfunction and it plays an important role in the clustering of risk factors of atherosclerosis.89-91 In addition, endothelial damage caused by insulin resistance appears to have particularly significant effects on small arterioles.92-94 Use of contrast materials may not be suitable for those patients, and therefore, CT angiography or coronary angiography is not applied for screening CAD. While stress perfusion imaging is a method of choice to rule out CAD, stress test may not be suitable for many of these patients.
As previously described, BMIPP imaging is a useful means for identifying ischemia and/or ischemic history of ischemia (ischemic memory) as an area of reduced BMIPP uptake at rest. Based on these results, Nishimura et al95 first applied BMIPP imaging for detection of CAD in hemodialysis patients. They demonstrated high prevalence of BMIPP abnormalities and coronary arteriography confirmed coronary stenosis on those showing BMIPP abnormalities. These patients often have silent myocardial ischemia but many of these patients may not be feasible to receive stress perfusion imaging. In this respect, BMIPP imaging may hold a promise to identify ischemia at rest without stress study. Based on the idea that BMIPP abnormalities are associated with severe ischemia and jeopardized myocardium, we hypothesized that those with severe BMIPP abnormalities may have poor outcome on the follow-up in hemodialysis patients. In the prospective 375 asymptomatic hemodialysis patients, severe BMIPP defect identify high-risk for cardiac death on the follow-up study.96 In addition, BMIPP and perfusion mismatch also showed a significant predictor for cardiac death in these patients. Furthermore, BMIPP findings may also be associated cardiac death after coronary revascularization in these patients.97 These data indicate that many hemodialysis patients may have silent myocardial ischemia and infarction. Since severe metabolic alteration may have future fatal events, BMIPP may have an important role to select such high risk group who may require early revascularization therapy.
Based on this experience, a multicenter prospective trial has recently been designed to investigate the applicability of BMIPP-SPECT imaging for detection of CAD and prediction of cardiac events in hemodialysis patients. We call this study as BMIPP-SPECT analysis for decreasing cardiac events (B-SAFE in hemodialysis patients).98 Regional decrease in BMIPP uptake in the left ventricular myocardium was occasionally observed similarly to the previous reports in these patients with hemodialysis. The frequency of the BMIPP abnormalities and their relation to the various clinical data has been precisely investigated at present. In addition, prognostic study will come out in a moment. This is the first multicenter cohort study to demonstrate frequency of BMIPP abnormalities in relation to various clinical parameters and to clarify the value of new fatty acid imaging to detect CAD and assess risk stratification in patients with hemodialysis. On the other hand, there has been no definite study showing the value of BMIPP imaging for general population of CKD without hemodialysis. Many CKD patients may often have silent ischemia. Particularly, the CKD patients with high risk subgroup are good candidate for stress myocardial perfusion imaging to rule out CAD. But some patients may not be suitable for exercise or pharmacological stress test. In this respect, BMIPP imaging may be one of alternative for CAD diagnosis and further management without need of stress condition.
Conclusions
Both MIBG and BMIPP imaging has provided valuable for assessment of myocardial disorders in various clinical settings. MIBG has been used for assessing severity of HF and prognosis. In addition, it has a potential role to predict fatal arrhythmia, particularly for those who had and are planned to receive implantable ICD treatment. In this sense, MIBG may hold a promise for reducing medical cost and proving personalized medicine in patients with severe HF. BMIPP plays an important role for identifying ischemia at rest, based on the unique capability to represent persistent metabolic alteration after recovery of ischemia, so called ischemic memory. Since BMIPP abnormalities may represent severe ischemia or jeopardized myocardium, it may permit risk analysis in CAD patients, particularly for those with CKD and/or hemodialysis patients. Such iodinated imaging provides unique molecular and cellular functions beyond myocardial perfusion and cardiac function in vivo. Such imaging may hold a promise to play an important role to select which individual patient may require expensive new treatment, and thus, to permits suitable treatment strategy in cardiovascular diseases in the near future.
References
Wu JC, Bengel FM, Gambhir SS. Cardiovascular molecular imaging. Radiology 2007;244:337-55.
Sinusus AJ, Bengel F, Nahrendorf M, Epstein FH, Wu JC, Villanueva FS, et al. Multimodality cardiovascular molecular imaging. Part I. Circ Cardiovasc Imaging 2008;1:244-56.
Bengel FM, Higuchi T, Javadi M, Lautamaki R. Cardiac positron emission tomography. J Am Coll Cardiol 2009;54:1-15.
Manger WM, Hoffman BB. Heart imaging in the diagnosis of pheochromocytoma and assessment of catecholamine uptake [teaching editorial]. J Nucl Med 1983;24:1194-6.
Tobes MC, Jacques S, Wieland DM, Sisson JC. Effect of uptake one inhibitors on the uptake of norepinephrine and metaiodobenzylguanidine. J Nucl Med 1985;26:897-907.
Degrado TR, Zalutsky MR, Vaidyanathan G. Uptake mechanisms of meta-[123I]iodobenzylguanidine in isolated rat heart. Nucl Med Biol 1995;22:1-12.
Inoue Y, Suzuki A, Shirouzu I, Machida T, Yoshizawa Y, Akita F, et al. Effect of collimator choice on quantitative assessment of cardiac iodine 123 MIBG uptake. J Nucl Cardiol 2003;10:623-32.
Pfiffer MA, Braunwald E, Moye LA, et al. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction. Results of the survival and ventricular enlargement trial. The SAVE Investigators. N Engl J Med 1992;327:669-77.
Matsuo S, Nakajima K, Yamashina S, Sakata K, Momose M, Hashimoto J, et al. Characterization of Japanese standards for myocardial sympathetic and metabolic imaging in comparison with perfusion imaging. Ann Nucl Med 2009;23:517-22.
Packer M, Bristow MR, Cohn JN, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. U.S. Carvedilol Heart Failure Study Group. N Engl J Med 1996;334:1349-55.
Cohn JN, Levine TB, Olivari MT, et al. Plasma norepinephrine as a guide to prognosis in patients with chronic congestive heart failure. N Engl J Med 1984;311:819-23.
Hall C, Rouleau JL, Moye L, et al. N-terminal proatrial natriuretic factor. An independent predictor of long-term prognosis after myocardial infarction. Circulation 1994;89:1934-42.
Omland T, Aakvaag A, Bonarjee VV, et al. Plasma brain natriuretic peptide as an indicator of left ventricular systolic function and long-term survival after acute myocardial infarction. Comparison with plasma atrial natriuretic peptide and N-terminal proatrial natriuretic peptide. Circulation 1996;93:1963-9.
Tsutamoto T, Wada A, Maeda K, et al. Attenuation of compensation of endogenous cardiac natriuretic peptide system in chronic heart failure: Prognostic role of plasma brain natriuretic peptide concentration in patients with chronic symptomatic left ventricular dysfunction. Circulation 1997;96:509-16.
Bristow MR, Ginsburg R, Minobe W, et al. Decreased catecholamine sensitivity and beta-adrenergic-receptor density in failing human hearts. N Engl J Med 1982;307:205-11.
Fowler MB, Laser JA, Hopkins GL, Minobe W, Bristow MR. Assessment of the beta-adrenergic receptor pathway in the intact failing human heart: Progressive receptor down-regulation and subsensitivity to agonist response. Circulation 1986;74:1290-302.
Ruffolo RR Jr, Kopia GA. Importance of receptor regulation in the pathophysiology and therapy of congestive heart failure. Am J Med 1986;80:67-72.
Merlet P, Delforge J, Syrota A, et al. Positron emission tomography with 11C CGP-12177 to assess beta-adrenergic receptor concentration in idiopathic dilated cardiomyopathy. Circulation 1993;87:1169-78.
Tsukamoto T, Morita K, Naya M, Inubushi M, Katoh C, Nishijima K, et al. Decreased myocardial beta-adrenergic receptor density in relation to increased sympathetic tone in patients with nonischemic cardiomyopathy. J Nucl Med 2007;48:1777-82.
Wieland DM, Brown LE, Rogers WL, et al. Myocardial imaging with a radioiodinated norepinephrine storage analog. J Nucl Med 1981;22:22-31.
Henderson EB, Kahn JK, Corbett JR, et al. Abnormal I-123 metaiodobenzylguanidine myocardial washout and distribution may reflect myocardial adrenergic derangement in patients with congestive cardiomyopathy. Circulation 1988;78:1192-9.
Schofer J, Spielmann R, Schuchert A, Weber K, Schluter M. Iodine-123 meta-iodobenzylguanidine scintigraphy: A noninvasive method to demonstrate myocardial adrenergic nervous system disintegrity in patients with idiopathic dilated cardiomyopathy. J Am Coll Cardiol 1988;12:1252-8.
Glowniak JV, Turner FE, Gray LL, Palac RT, Lagunas-Solar MC, Woodward WR. Iodine-123 metaiodobenzylguanidine imaging of the heart in idiopathic congestive cardiomyopathy and cardiac transplants. J Nucl Med 1989;30:1182-91.
Merlet P, Dubois-Rande JL, Adnot S, et al. Myocardial beta-adrenergic desensitization and neuronal norepinephrine uptake function in idiopathic dilated cardiomyopathy. J Cardiovasc Pharmacol 1992;19:10-6.
Merlet P, Pouillart F, Dubois-Rande JL, et al. Sympathetic nerve alterations assessed with 123I-MIBG in the failing human heart. J Nucl Med 1999;40:224-31.
Cohen-Solal A, Rouzet F, Berdeaux A, et al. Effects of carvedilol on myocardial sympathetic innervation in patients with chronic heart failure. J Nucl Med 2005;46:1796-803.
Merlet P, Benvenuti C, Moyse D, et al. Prognostic value of MIBG imaging in idiopathic dilated cardiomyopathy. J Nucl Med 1999;40:917-23.
Merlet P, Valette H, Dubois-Rande JL, et al. Prognostic value of cardiac metaiodobenzylguanidine imaging in patients with heart failure. J Nucl Med 1992;33:471-7.
Momose M, Kobayashi H, Iguchi N, et al. Comparison of parameters of 123I-MIBG scintigraphy for predicting prognosis in patients with dilated cardiomyopathy. Nucl Med Commun 1999;20:529-35.
Yamada T, Shimonagata T, Fukunami M, et al. Comparison of the prognostic value of cardiac iodine-123 metaiodobenzylguanidine imaging and heart rate variability in patients with chronic heart failure: A prospective study. J Am Coll Cardiol 2003;41:231-8.
Nakata T, Miyamoto K, Doi A, Sasao H, Wakabayashi T, Kobayashi H, et al. Cardiac death prediction and impaired cardiac sympathetic innervation assessed by MIBG in patients with failing and nonfailing hearts. J Nucl Cardiol 1998;5:579-90.
Nakata T, Wakabayashi T, Kyuma M, Takahashi T, Hashimoto A, Ogata H. Prognostic implications of an initial loss of cardiac metaiodobenzylguanidine uptake and diabetes mellitus in patients with left ventricular dysfunction. J Card Fail 2003;9:113-21.
Kyuma M, Nakata T, Hashimoto A, Nagao K, Sasao H, Takahashi T, et al. Incremental prognostic implications of brain natriuretic peptide, cardiac sympathetic nerve innervation, and noncardiac disorders in patients with heart failure. J Nucl Med 2004;45:155-63.
Imamura Y, Fukuyama T, Mochizuki T, Miyagawa M, Watanabe K, Ehime MIBG Heart Failure Study Investigators. Prognostic value of Iodine-123-metaiodobenzylguanidine imaging and cardiac natriuretic peptide levels in patients with left ventricular dysfunction resulting from cardiomyopathy. Jpn Circ J 2001;65:155-60.
Fujimoto S, Amano H, Inoue A, Ishida S, Yamashina S, Yamashina H, et al. Usefulness of 123I-metaiodobenzylguanidine myocardial scintigraphy in the prediction of cardiac events in patients with cardiomyopathy showing stabilization of symptoms or preserved cardiac function. Ann Nucl Med 2004;18:591-8.
Agostini D, Verberne HJ, Burchert W, Knuuti J, Povinec P, Sambuceti G, et al. I-123-mIBG myocardial imaging for assessment of risk for a major cardiac event in heart failure patients: Insights from a retrospective European multicenter study. Eur J Nucl Med Mol Imaging 2008;35:535-46.
Tamaki S, Yamada T, Okuyama Y, Morita T, Sanada S, Tsukamoto Y, et al. Cardiac iodine-123 metaiodobenzylguanidine imaging predicts sudden cardiac death independently of left ventricular ejection fraction in patients with chronic heart failure and left ventricular systolic dysfunction. J Am Coll Cardiol 2009;53:426-35.
Brunner M, Peng X, Liu GX, Ren XQ, Ziv O, Choi BR, et al. Mechanisms of cardiac arrhythmias and sudden death in transgenic rabbits with long QT syndrome. J Clin Invest 2008;118:2246-59.
Verberne HJ, Brewster LM, Somsen GA, van Eck-Smit BL. Prognostic value of myocardial 123I-metaiodobenzylguanidine (MIBG) parameters in patients with heart failure: A systematic review. Eur Heart J 2008;29:1147-59.
Verberne HJ, Habraken JB, van Eck-Smit BL, Agostini D, Jacobson AF. Variations in 123I-metaiodobenzylguanidine (MIBG) late heart mediastinal ratios in chronic heart failure: A need for standardisation and validation. Eur J Nucl Med Mol Imaging 2008;35:547-53.
Suwa M, Otake Y, Moriguchi A, et al. Iodine-123 metaiodobenzylguanidine myocardial scintigraphy for prediction of response to beta-blocker therapy in patients with dilated cardiomyopathy. Am Heart J 1997;133:353-8.
Kakuchi H, Sasaki T, Ishida Y, Komamura K, Miyatake K. Clinical usefulness of 123I meta-iodobenzylguanidine imaging in predicting the effectiveness of beta blockers for patients with idiopathic dilated cardiomyopathy before and soon after treatment. Heart 1999;81:148-52.
Spyrou N, Rosen SD, Fath-Ordoubadi F, et al. Myocardial beta-adrenoceptor density one month after acute myocardial infarction predicts left ventricular volumes at six months. J Am Coll Cardiol 2002;40:1216-24.
Naya M, Tsukamoto T, Morita K, Katoh C, Nishijima K, Komatsu H, et al. Myocardial beta-adrenergic receptor density assessed by 11C-CGP12177 PET predicts improvement of cardiac function after carvedilol treatment in patients with idiopathic dilated cardiomyopathy. J Nucl Med 2009;50:220-5.
Josephson M, Wellens HJ. Implantable defibrillators and sudden cardiac death. Circulation 2004;109:2685-91.
Epstein AE, DiMarco JP, Ellenbogen KA, et al. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities. J Am Coll Cardiol 2008;51:e1-62.
Moss AJ, Greenberg H, Case RB, et al. Long-term clinical course of patients after termination of ventricular tachyarrhythmia by an implantable defibrillator. Circulation 2004;110:3760-5.
Bardy GH, Lee KL, Mark DB, et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Eng J Med 2005;352:225-37.
Tung R, Zimetbaum P, Josephson ME. A critical appraisal of implantable cardioverter-defibrillator therapy for the prevention of sudden cardiac death. J Am Coll Cardiol 2008;52:1111-21.
Myerburg RJ, Reddy V, Castellanos A. Indications for implantable cardioverter-defibrillators based on evidence and judgment. J Am Coll Cardiol 2009;54:747-63.
Podrid PJ, Fuchs T, Candinas R. Role of the sympathetic nervous system in the genesis of ventricular arrhythmia. Circulation 1990;822:I103-13.
Zipes DP. Sympathetic stimulation and arrhythmias. N Eng J Med 1991;325:656-7.
Mitrani RD, Klein LS, Miles WM, et al. Regional cardiac sympathetic denervation in patients with ventricular tachycardia in the absence of coronary artery disease. J Am Coll Cardiol 1993;22:1344-53.
Arora R, Ferrick KJ, Nakata T, et al. I-123 MIBG imaging and heart rate variability analysis to predict the need for an implantable cardioverter defibrillator. J Nucl Cardiol 2003;10:121-31.
Nagahara D, Nakata T, Hashimoto A, et al. Predicting the need of an implantable cardioverter defibrillator using metaiodobenzylguanidine activity together with plasma natriuretic peptide concentration or left ventricular function. J Nucl Med 2008;49:225-33.
Bax JJ, Kraft O, Buxton AE, et al. 123I-MIBG scintigraphy to predict testing. A prospective multicenter pilot study. Circ Cardiovasc Imaging 2009;1:131-40.
Jacobson AF, Senior R, Cerqueira MD, Thomas GS, Agostini D, Weiland W, et al. Myocardial 123I-mIBG imaging and cardiac events in heart failure: Results of the prospective ADMIRE-HF study. J Am Coll Cardiol 2010;55:2212-21.
Strauss HW, Johnson MN, Schoder H, Tamaki N. Metaiodobenzylguanidine imaging comes of age. J Am Coll Cardiol 2010;55:2222-4.
Boogers MJ, Borleffs JW, Henneman MM, van Bommel RJ, van Ramshort J, Boersma E, et al. Cardiac sympathetic denervation assessed with 123-iodine metaiodobenzylguanidine imaging predicts ventricular arrhythmias in implantable cardioverter defibrillator patients. J Am Coll Cardiol 2010;55:2769-77.
Nishisato K, Hashimoto A, Nakata T, Doi T, Yamamopto H, Nagahara D, et al. Impaired cardiac sympathetic innervations and myocardial perfusion are related to lethal arrhythmia: Quantification of cardiac tracers in patients with ICDs. J Nucl Med 2010;51:1241-9.
Knapp FF Jr, Goodman MM, Callahan AP, et al. Radioiodinated 15-(p-iodophenyl)-3,3-dimethylpentadecanoic acid: A useful new agent to evaluate myocardial fatty acid uptake. J Nucl Med 1986;27:521-31.
Tamaki N, Fujibayashi Y, Magata Y, et al. Radionuclide assessment of myocardial fatty acid metabolism by PET and SPECT. J Nucl Cardiol 1995;2:256-66.
Tamaki N, Morita K, Kuge Y, Tsukamoto E. The role of fatty acids in cardiac imaging. J Nucl Med 2000;41:1525-34.
Tamaki N, Morita K, Kawai Y. The Japanese experience with metabolic imaging in the clinical setting. J Nucl Cardiol 2007;14:S145-52.
Kawai Y, Tsukamoto E, Nozaki Y, et al. Use of 123I-BMIPP single-photon emission tomography to estimate areas at risk following successful revascularization in patients with acute myocardial infarction. Eur J Nucl Med 1998;25:1390-5.
Nakajima K, Schimizu K, Taki J, et al. Utility of iodine-123-BMIPP in the diagnosis and follow-up of vasospastic angina. J Nucl Med 1995;36:1934-40.
Takeishi Y, Fujiwara S, Atsumi H, et al. Iodine-123-BMIPP imaging in unstable angina: A guide for interventional therapy. J Nucl Med 1997;38:1407-11.
Fujiwara S, Takeishi Y, Atsumi H, et al. Fatty acid metabolic imaging with iodine-123-BMIPP for the diagnosis of coronary artery disease. J Nucl Med 1997;38:175-80.
Tateno M, Tamaki N, Kudoh T, et al. Assessment of fatty acid uptake in patients with ischemic heart disease without myocardial infarction. J Nucl Med 1996;37:1981-5.
Suzuki A, Takada Y, Nagasaka M, et al. Comparison of resting β-methyl-iodophenyl pentadecanoic acid (BMIPP) and thallium-201 tomography using quantitative polar maps in patients with unstable angina. Jpn Circ J 1997;61:133-8.
Yamabe H, Fujiwara S, Rin K, et al. Resting 123I-BMIPP scintigraphy for detection of organic coronary stenosis and therapeutic outcome in patients with chest pain. Ann Nucl Med 2000;14:187-92.
Kawai Y, Tsukamoto E, Nozaki Y, Morita K, Sakurai M, Tamaki N. Significance of reduced uptake of iodinated fatty acid analogue for the evaluation of patients with acute chest pain. J Am Coll Cardiol 2001;38:1888-94.
Watanabe K, Takahashi T, Miyajima S, et al. Myocardial sympathetic denervation, fatty acid metabolism, and left ventricular wall motion in vasospastic angina. J Nucl Med 2002;43:1476-81.
Inaba Y, Bergmann SR. Diagnostic accuracy of beta-methyl-para-[123I]-iodophenyl-pentadecanoic acid (BMIPP) imaging: A meta-analysis. J Nucl Cardiol 2008;15:345-52.
Kawai Y, Morita K, Nozaki Y, Ohkusa T, Sakurai M, Tamaki N. Diagnostic value of 123I-betamethyl-p-iodophenyl-pentadecanoic acid (BMIPP) single photon emission computed tomography (SPECT) in patients with chest pain—Comparison with rest-stress 99mTc-tetrofosmin SPECT and Coronary angiography. Circ J 2004;68:547-52.
Kontos MC, Dilsizian V, Weiland F, DePuey G, Mahmarian JJ, Iskandrian AE, et al. Iodofiltic acid I-123 (BMIPP) fatty acid imaging improves initial diagnosis in emergency department patients with suspected acute coronary syndromes. J Am Coll Cardiol 2010;56:290-9.
Dilsizian V, Bateman TM, Bergmann SR, Des Prez R, Magram MY, Goodbody AE, et al. Metabolic imaging with beta-methyl-p-[(123)I]-iodophenyl-pentadecanoic acid identifies ischemic memory after demand ischemia. Circulation 2005;112:2169-74.
Tamaki N, Tadamura E, Kudoh T, et al. Prognostic value of iodine-123 labelled BMIPP fatty acid analogue imaging in patients with myocardial infarction. Eur J Nucl Med 1996;23:272-9.
Nakata T, Kobayashi T, Tamaki N, et al. Prognostic value of impaired myocardial fatty acid uptake in patients with acute myocardial infarction. Nucl Med Commun 2000;21:897-907.
Fukuzawa S, Ozawa S, Shimada K, et al. Prognostic values of perfusion-metabolic mismatch in Tl-201 and BMIPP scintigraphic imaging in patients with chronic coronary artery disease and left ventricular dysfunction undergoing revascularization. Ann Nucl Med 2002;16:109-15.
Nanasato M, Hirayama H, Ando A, Isobe S, Nonokawa M, Kinoshita Y, et al. Incremental predictive value of myocardial scintigraphy with 123I-BMIPP in patients with acute myocardial infarction treated with primary percutaneous coronary intervention. Eur J Nucl Med Mol Imaging 2004;31:1512-21.
Matsuki T, Tamaki N, Nakata T, et al. Prognostic value of fatty acid imaging in patients with angina pectoris without prior myocardial infarction: Comparison with stress thallium imaging. Eur J Nucl Med Mol Imaging 2004;31:1585-91.
Chikamori T, Fujita H, Nanasato M, Toba M, Nishimura T. Prognostic value of I-123 15-(p-iodophenyl)-3-(R,S) methylpentadecanoic acid myocardial imaging in patients with known or suspected coronary artery disease. J Nucl Cardiol 2005;12:172-8.
Inaba Y, Bergmann SR. Prognostic value of myocardial metabolic imaging with BMIPP in the spectrum of coronary artery disease: A systemic review. J Nucl Cardiol 2010;17:61-70.
Rostand SG, Rutsky EA. Ischemic heart disease in chronic renal failure: Management considerations. Semin Dial 1989;2:98-101.
Ansell D, Roderick P, Hodsman A, et al. UK Renal Registry 11th annual report (December 2008): Chapter 7 Survival and causes of death of UK adult patients on renal replacement therapy in 2007: National and centre-specific analyses. Nephron Clin Pract 2009;111:c113-39.
Foley RN, Parfrey PS, Sarnak MJ. Epidemiology of cardiovascular disease in chronic renal disease. J Am Soc Nephrol 1998;9:S16-23.
DeFronzo RA, Alvestrand A, Smith D, et al. Insulin resistance in uremia. J Clin Invest 1981;67:563-8.
Wheatcroft SB, Williams IL, Shah AM, et al. Pathophysiological implications of insulin resistance on vascular endothelial function. Diabet Med 2003;20:255-68.
Jiang ZY, Lin YW, Clemont A, et al. Characterization of selective resistance to insulin signaling in the vasculature of obese Zucker (fa/fa) rats. J Clin Invest 1999;104:447-57.
Balletshofer BM, Ritting K, Enderle MD, et al. Endothelial dysfunction is detectable in young normotensive first-degree relatives of subjects with type 2 diabetes in association with insulin resistance. Circulation 2000;101:1780-4.
Jaap AJ, Shore AC, Tooke JE. Relationship of insulin resistance to microvascular dysfunction in subjects with fasting hyperglycemia. Diabetologia 1997;40:238-43.
Serne EH, Stehouwer CD, ter Maaten JC, et al. Microvascular function relates to insulin sensitivity and blood pressure in normal subjects. Circulation 1999;99:896-902.
Dagres N, Saller B, Haude M, et al. Insulin sensitivity and coronary vasoreactivity: Insulin sensitivity relates to adenosine-stimulated coronary flow response in human subjects. Clin Endocrinol 2004;61:724-31.
Nishimura M, Hashimoto T, Kobayashi H, Fukuda T, Okino K, Yamamoto N, et al. Myocardial scintigraphy using a fatty acid analogue detects coronary artery disease in hemodialysis patients. Kidney Int 2004;66:811-29.
Nishimura M, Tsukamoto K, Hasebe N, et al. Prediction of cardiac death in hemodialysis patients by myocardial fatty acid imaging. J Am Coll Cardiol 2008;51:139-45.
Nishimura M, Tokoro T, Nishida M, et al. Prediction of cardiac death after coronary revascularization by myocardial fatty acid imaging in hemodialysis patients. Kidney Int 2008;74:513-20.
Hasebe N, Moroi M, Nishimura M, Hara K, Hase H, Hashimoto A, et al. Prognostic study of cardiac events in Japanese high risk hemodialysis patients using 123I-BMIPP-SPECT: B-SAFE study design. Ther Apher Dial 2008;12:526-30.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Tamaki, N., Yoshinaga, K. Novel iodinated tracers, MIBG and BMIPP, for nuclear cardiology. J. Nucl. Cardiol. 18, 135–143 (2011). https://doi.org/10.1007/s12350-010-9305-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-010-9305-4