Abstract
Introduction
Post hoc analyses (two single-arm studies) were conducted to determine the impact of once-monthly injection of paliperidone palmitate on functioning in adult patients with schizophrenia in the Asia–Pacific region.
Methods
Study 1 enrolled hospitalized patients with acute exacerbation of schizophrenia, and study 2 enrolled patients with recently diagnosed schizophrenia unsatisfactorily treated with oral antipsychotics. Patients received paliperidone palmitate, 150 mg eq. on day 1, 100 mg eq. on day 8, then once monthly (50–150 mg eq.) (study 1, days 36 and 64; study 2, 18 months). Functional status was evaluated by Personal and Social Performance score in both studies and employment only in study 2.
Results
In study 1, 54 of 184 patients (29.4%) with an unfavorable level of functioning at the baseline improved to a favorable level (Personal and Social Performance score greater than 70) at day 92. This improvement was significantly greater among patients with recently diagnosed schizophrenia (5 years or less) compared with patients with chronic schizophrenia (more than 5 years): 40% versus 22% (p < 0.0001). Improvements were observed in all four domains (socially useful activities, personal and social relationships, self-care, disturbing/aggressive behavior). In study 2, significant (p < 0.0001) improvement in functioning was observed at all visits, beginning at week 5. Almost half (48.7%, 247/507) of patients showed clinically meaningful improvement in functioning (i.e., 10 point or greater increase in Personal and Social Performance score) at month 18. The proportion of patients fully/partially employed was greater at all postbaseline visits (134 of 280, 47.9%, at month 18) as compared with the baseline.
Conclusion
Functioning, including employment, was improved after short-term, once-monthly paliperidone palmitate injection, and was sustained to 18 months in Asia–Pacific patients with schizophrenia.
Funding
Janssen-Cilag Asia–Pacific Medical Affairs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Schizophrenia is a chronic mental illness characterized by a range of severe psychotic symptoms that may recur and progress over time [1, 2], adversely affecting the lives of patients and their caregivers [3, 4]. Furthermore, deficits in social functioning are a core feature of schizophrenia; therefore, not surprisingly, deterioration (or failure to achieve adequate levels) of social functioning is a diagnostic criterion of schizophrenia [5]. In addition to social functioning, occupational aspects of patient functioning may also be affected, as is independent living [6, 7].
Functional disability is recognized as an important long-term outcome of patients with schizophrenia [8, 9]. Most patients (up to two thirds) cannot perform basic social roles, even during periods of remission, few marry, and only a minority (less than one third) are able to maintain everyday employment [10]. According to Rosenheck et al. [11], only one in every seven patients with schizophrenia reported regular, paid employment, and those who were unemployed reported lower quality-of-life scores. Social dysfunction is an important aspect in the overall disability of schizophrenia, causing great distress for not only patients but also their family [10]. Taken together, the societal (including economic) burden of poor functioning among those with schizophrenia is sizable [10].
Beyond control of characteristic positive and negative symptoms and delaying/prevention of recurrence, functional recovery is also a requisite goal of schizophrenia treatment and an important determinant of treatment success [12,13,14]. Affected patients as well as their families acknowledge the importance of improved functioning among their expectations for treatment [10], which is therefore included in schizophrenia treatment guidelines [4, 15, 16]. However, evidence of the effect of antipsychotic agents on social and occupational functioning in schizophrenia patients, especially those in the Asia–Pacific region, is limited.
Paliperidone palmitate 1-month formulation (PP1M), a once-monthly long-acting injectable (LAI) atypical antipsychotic, is approved in the USA, Europe, and major Asia–Pacific countries for acute and maintenance treatment of schizophrenia. Proof of its efficacy and safety for treatment of schizophrenia was established on the basis of results of numerous studies conducted across these geographic regions [17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34], including the Asia–Pacific region [35,36,37,38,39,40]. Improvement in function among PP1M-treated patients as assessed by the Personal and Social Performance (PSP) scale [41], a validated, clinician-reported instrument for assessing personal and social functioning of patients with schizophrenia [42], was reported in several global studies [17,18,19, 22, 24,25,26, 28,29,30,31,32,33] and in Asia–Pacific regional studies [35,36,37,38].
In clinical practice, many physicians use an LAI as the last choice rather than the first choice. Given the importance of personal, social, and occupational functioning and the aim of improving outcomes of schizophrenia patients, additional PSP analyses were conducted to examine the effect of PP1M on the various dimensions of functioning in patients with schizophrenia across the Asia–Pacific region. Further analyses were performed to evaluate the effects of PP1M in patients with recently diagnosed schizophrenia (5 years or less) as compared with chronic disease (more than 5 years). The results for Positive and Negative Syndrome Scale (PANSS) total score, the primary efficacy end point, and other prespecified secondary end points (e.g., PANSS domain/symptom factor scores, Clinical Global Impression–Schizophrenia, Clinical Global Impression–Severity, symptom remission) of the studies are reported elsewhere [36, 40].
Methods
An independent ethics committee or institutional review board at the study sites approved the study protocol of each study, and both studies were conducted in accordance with the ethical principles that have their origin in the Declaration of Helsinki and that are consistent with good clinical practices and applicable regulatory requirements. All patients or their legally acceptable representatives provided written informed consent before the patients entered one of the studies. Study 1 [36] (NCT01527305) and study 2 [40] (NCT01051531) are registered at ClinicalTrials.gov.
Study 1
Patients
Asian patients of either sex, between 18 and 65 years old, with a diagnosis of schizophrenia (based on Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV), criteria [43]), with a PANSS total score of 60 or greater or a Clinical Global Impression–Severity score of 4 or greater, and hospitalized with an acute exacerbation within the previous 4 weeks were enrolled. Those with a primary active DSM-IV Axis I diagnosis other than schizophrenia, a history of substance dependence within 6 months of screening, at significant suicide risk, and who used clozapine or long-acting antipsychotics (including PP1M) within 1 month of screening were excluded.
Study Design and Treatment
This nonrandomized, single-arm, open-label, multicenter study was conducted between June 2012 and December 2013 across four Asian countries including China (six sites), Korea (ten sites), Malaysia (three sites), and Taiwan (eight sites). The study consisted of an up to 7-day screening period, followed by an open-label treatment period (13 weeks), and an end-of-study visit on day 92 (week 13), 1 month after the last PP1M injection.
On day 1, eligible patients were switched to treatment with PP1M from their existing oral antipsychotic medication. Patients without documented tolerability to orally administered risperidone, extended-release paliperidone, risperidone LAI, or PP1M underwent oral tolerability testing during the screening period with extended-release paliperidone, 3 mg/day, or orally administered risperidone, 1 mg/day, for at least 2 days. Treatment with PP1M was initiated at a dose of 150 mg eq. on day 1, followed by 100 mg eq. on day 8 (both doses in the deltoid muscle) and flexible once-monthly injections of 75, 100, or 150 mg eq. in the deltoid or gluteal muscle, at the investigator’s discretion, on days 36 and 64.
Assessment of Functioning
Functional status was evaluated by PSP, which was administered to patients by a trained and qualified clinician/rater at the baseline and at visits conducted on days 4, 8, 36, 64, and 92.
PSP is a clinician-rated instrument that provides an overall rating of personal and social functioning in patients with schizophrenia [41]. The scale, which ranges from 1 to 100, defines a continuum of functioning from grossly impaired, in which total lack of autonomy in basic functioning and survival risk is evident, to excellent functioning. Higher scores represent better functioning. Four domains of functioning are considered in the rating: (1) socially useful activities, including work and study; (2) personal and social relationships; (3) self-care; and (4) disturbing and aggressive behavior. For each domain, the degree of dysfunction a patient exhibits during the month before a visit is rated on a six-point severity scale (absent, mild, manifest, marked, severe, and very severe).
Study 2
Patients
Adults (between 18 and 50 years old) with a recent (5 years or less) diagnosis of schizophrenia (based on DSM-IV criteria [43]) who had not responded adequately to previous oral antipsychotics (because of lack of efficacy, tolerability/safety, or adherence) were enrolled. Key exclusion criteria were as follows: treatment resistance; DSM-IV diagnosis of substance dependence in the 6 months before entry to the study; treatment with an LAI antipsychotic within three injection cycles before the baseline or clozapine within the most recent prior 3 months.
Study Design and Treatment
This 18-month, nonrandomized, single-arm, open-label, multicenter study was conducted between April 2010 and May 2013 across nine countries in the Asia–Pacific region, including Australia (nine sites), China (six sites), Hong Kong (two sites), Korea (ten sites), Malaysia (nine sites), New Zealand (one site), Philippines (two sites), Taiwan (six sites), and Thailand (three sites). The study consisted of an up to 7-day screening period, followed by an 18-month open-label treatment period, and an end-of-study/early-withdrawal visit 1 month after the last PP1M injection.
Eligible patients were switched to treatment with PP1M from their existing oral antipsychotic treatment that was discontinued before day 1, with the exception that those pretreated with high doses of oral antipsychotics having sedating and/or anticholinergic properties could taper off these medications through the first month of the study. Treatment with PP1M was initiated at a dose of 150 mg eq. on day 1, followed by 100 mg eq. on day 8 (both doses in the deltoid muscle) and flexible once-monthly injections of 50, 75, 100, or 150 mg eq. in the deltoid or gluteal muscle, at the investigator’s discretion.
Assessments of Functioning and Employment
In a manner similar to that in study 1, functional status was evaluated by PSP, which a trained and qualified clinician/rater administered to patients at the baseline and at visits conducted on days 38, 188, 368, and 548 (or at early withdrawal) in study 2.
Specifically for study 2, employment status (full-time, part-time, casual, sheltered, unemployed but seeking or not seeking work, retired, housewife or dependent spouse, student) was recorded at every 3-month visits during the 18-month study.
Statistical Analyses
Analyses were performed on an intent-to-treat population, which included all patients who received at least one injection of PP1M. For efficacy, the last observation carried forward approach was used for end point analyses.
In study 1, baseline demographic and clinical characteristics of patients with recently diagnosed schizophrenia (5 years or less) were compared with those of patients with chronic disease (more than 5 years) by analysis of variance or chi-square tests. The breakpoint of 5 years, differentiating recently diagnosed schizophrenia from chronic schizophrenia, was based on findings from recently published schizophrenia research [44, 45].
The mean change from the baseline in PSP total score to each visit was analyzed with a paired t test and two-sided 95% confidence intervals in both studies. In study 1, the mean change in PSP total score between the duration of schizophrenia (5 years or less and more than 5 years) was compared with an analysis of covariance (ANCOVA) model with group as a factor and baseline score as a covariate.
Between-group differences for the categorical summaries of PSP total score (and PSP domain scores in study 1) were compared by a chi-square test (or Fisher’s test when cell counts were less than 5), as was clinically meaningful improvement defined by improvement of one or more categories (classified as a 10-point interval) [46, 47]. Shifts from the baseline to each visit by PSP total score category (unfavorable level 70 or less; favorable level more than 70) were summarized, and the change was analyzed at each postbaseline assessment with McNemar’s test. In study 2, the shift from the baseline to month 18 in employment status (full employment, partial employment, unemployment, and out of employment) was analyzed by the Bowker (chi-square) test of symmetry.
Results
Study 1
Patient Disposition and Clinical Characteristics
Study 1 enrolled 212 patients, 152 (71.7%) of whom completed the 13-week treatment. The study population comprised all Asian patients, and was balanced by sex (Table 1). The mean age was approximately 37 years. With few exceptions, study patients had functional disability at study enrolment (75.5% with varying functioning and 23.6% with a poor level of function that required intensive supervision).
Change in Functioning with PP1M Treatment
Significant and clinically meaningful improvement in personal and social functioning from the baseline was observed for PP1M-treated patients. Significantly greater benefit for the mean change in PSP total score at week 13 from the baseline was observed in patients with recently diagnosed (5 years or less) compared with chronic (more than 5 years) schizophrenia [difference between subgroups with 95% confidence interval of 10.4 (6.14–14.73); p < 0.0001, Table 2]. In this study, 78.7% of patients (59/75) with recent-onset schizophrenia (5 years or less) and 57.8% or patients (63/109) with chronic schizophrenia (5 years or more) (p = 0.033 for difference between subgroups) showed clinically meaningful improvement in functioning (i.e., 10 point or greater increase in PSP total score).
Of the 184 patients who had an unfavorable level of functioning at the baseline (PSP score of 70 or less), 54 (29.4%) improved to a favorable level (PSP score greater than 70) after 13 weeks of treatment with PP1 M. Patients with recently diagnosed schizophrenia demonstrated a greater improvement compared with those with chronic disease (30 of 75, 40%, vs 24 of 109, 22.0%, respectively; p < 0.0001).
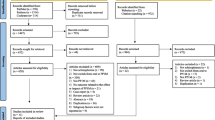
Improvements were demonstrated in all PSP domains (Fig. 1); the improvement was significantly (p < 0.05) greater among those with recently diagnosed schizophrenia compared with those with chronic schizophrenia for all domains except disturbing/aggressive behavior.
Study 2
Patient Disposition and Clinical Characteristics
Study 2 enrolled 585 patients, 510 (87.2%) of whom were from Asian countries, and the remainder (75, 12.8%) were from Australia and New Zealand. The intent-to-treat population comprised 521 patients (64 patients were excluded because of screening failure or their having been enrolled at a site in Australia that was determined to be noncompliant with good clinical practice), 303 (58.2%) of whom completed the study. PSP data were available for 516 patients and employment data were available for 469 patients at the baseline.
Enrollees were primarily men (65.5%) and had a mean age of approximately 29 years. In this study of patients with recently diagnosed schizophrenia, most (68.9%) had received a diagnosis within the past 3 years (mean 2.0 years). Most of the study patients had functional disability at study enrolment (68.4% with varying functioning and 6.8% with a poor level of function that required intensive supervision).
Change in Functioning with PP1M Treatment
Significant improvement in functioning from the baseline was observed at all visits (Table 3). At month 18, the mean increase (representing improvement) from the baseline in PSP total score was 10.5, resulting in almost half of patients (48.7%, 247/507) showing clinically meaningful improvement in functioning (i.e., 10 point or greater increase in PSP total score).
Of the 382 patients who had an unfavorable level of functioning at the baseline (PSP score of 70 or less), 153 (30.2%) improved to a favorable level (PSP score greater than 70) after 6 months of treatment with PP1 M, which was sustained after 18 months of treatment (176, 34.78%) (Table 4). This shift to a more favorable level of functioning was observed irrespective of the baseline severity of illness (i.e., baseline PANSS score; data not shown).
Functional improvement during treatment with PP1M was also reflected in significantly increased employment levels at all postbaseline visits (p ≤ 0.0036). The proportion of patients fully/partially employed was 50% greater at month 18 (47.9%, 134/280) as compared with the baseline (31.8%, 89/280). Sixty-six patients (of 280, 23.6%) with unemployment/out of employment status at the baseline had shifted to full employment/partial employment status at month 18, and of these patients, 52 (of 280, 18.6%; Table 5) with unemployment/out of employment status at the baseline had shifted to full employment.
Discussion
Despite favorable effects on psychopathological symptoms, many patients with schizophrenia treated with antipsychotic agents remain functionally impaired [5]. As deficits in psychosocial domains are a core feature of schizophrenia, efficient long-term treatment of patients with schizophrenia must effect psychosocial reintegration as well as reduce psychotic symptoms [12].
The results reported herein, based on a large cohort (total N = 729) of patients with schizophrenia in the Asia–Pacific region, show that most patients achieved significant and clinically meaningful improvement in function in the initial 3 months of PP1M treatment. All domains of personal and social functioning were improved. These early results were sustained for 18 months among patients with recently diagnosed disease. Improvement in employment status confirmed these functional gains. Taken together, these results underscore the importance of early initiation of effective treatment for functional improvement in schizophrenia. These findings confirm and extend the primary analyses [36, 40], and are consistent with other LAI antipsychotic studies that have reported similar effects on functioning in patients with schizophrenia. Further, examination of the domain scores reported here allows a more detailed understanding of functioning over time.
The open-label design and lack of a comparator group are limitations of these studies and may have contributed to confounding as well as observational bias of the investigators and from high expectations of patients. With this in mind, we did not evaluate if a relationship exists between improvement in functioning (PSP score) and improvement in symptom scores, although others have reported improvements in social functioning to be independent of concurrent reduction of the patients’ symptoms [48, 49]. Furthermore, the subgroup analyses by duration of illness were conducted on a post hoc basis, and should therefore be considered exploratory.
Our results of early and sustained functional improvement with PP1M treatment of Asia–Pacific patients with schizophrenia are consistent with the results from other studies of primarily Western patients with schizophrenia [17,18,19, 22, 24,25,26, 28,29,30,31,32,33]. For example, in a 13-week, double-blind, global study of patients (94.5% non-Asian patients, 5.5% Asian patients) with acute schizophrenia, Pandina et al. [30] noted a mean increase in PSP total score from the baseline to the study end point of 8.5 points among 453 patients treated with PP1M. Hargarter et al. [25] reported functional improvement of a similar magnitude (based on an increase in mean PSP total score) in an open-label 6-month study of 568 patients with nonacute schizophrenia treated with PP1M.
Treatment of acutely ill patients with PP1M was associated with improvement in all four domains of functioning. There was a substantial shift from severe/moderate toward mild/absent to absent impairment in socially useful activities, including work and study, personal/social relationships, self-care, and disturbing and aggressive behavior. These shifts are noteworthy because improvements in these domains may potentially be indicators of improved productivity, integration into society, and recovery, and they are especially important to patients and their families.
Notwithstanding these benefits, hurdles to early introduction of LAIs in the treatment of schizophrenia still exist [50]. Some patients express misgivings with injectable treatment based on fear of injection site pain, higher treatment cost (although studies prove otherwise [51, 52]), and perceived stigma [53], the latter particularly relevant for Asian patients. Slow adoption among physicians may stem from practical issues such as dose selection, inexperience with switching from an oral to an injectable formulation, and lack of institutional structure and trained staff to provide treatment [54–57]. Nevertheless, the results of this study and those of others [58] underscore the benefits of initiating treatment with LAIs early in the course of the disease for patients with schizophrenia.
Conclusion
In summary, PP1M treatment was associated with prompt and sustained improvement in functioning as well as increased employment levels among Asia–Pacific patients with schizophrenia. Improvement in functionality as observed with PP1M treatment may be an important clinical consideration when an antipsychotic agent is being selected for Asia–Pacific patients with schizophrenia.
References
Lieberman J, Chakos M, Wu H, et al. Longitudinal study of brain morphology in first episode schizophrenia. Biol Psychiatry. 2001;49:487–99.
McGlashan TH. A selective review of recent North American long-term followup studies of schizophrenia. Schizophr Bull. 1988;14:515–42.
Awad AG, Voruganti LN. The burden of schizophrenia on caregivers: a review. Pharmacoeconomics. 2008;26:149–62.
Falkai P, Wobrock T, Lieberman J, Glenthoj B, Gattaz WF, Möller HJ, WFSBP Task Force on Treatment Guidelines for Schizophrenia. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of schizophrenia, part 1: acute treatment of schizophrenia. World J Biol Psychiatry. 2005;6:132–91.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington: American Psychiatric Association; 2013.
Harvey PD, Green MF, Keefe RS, Velligan DI. Cognitive functioning in schizophrenia: a consensus statement on its role in the definition and evaluation of effective treatments for the illness. J Clin Psychiatry. 2004;65:361–72.
Harvey PD, Bellack AS. Toward a terminology for functional recovery in schizophrenia: is functional remission a viable concept? Schizophr Bull. 2009;35:300–6.
Burns T, Patrick D. Social functioning as an outcome measure in schizophrenia studies. Acta Psychiatr Scand. 2007;116:403–18.
Priebe S. Social outcomes in schizophrenia. Br J Psychiatry. 2007;191:s15–20.
Bellack AS, Green MF, Cook JA, et al. Assessment of community functioning in people with schizophrenia and other severe mental illnesses: a white paper based on an NIMH-sponsored workshop. Schizophr Bull. 2007;33:805–22.
Rosenheck R, Leslie D, Keefe R, et al. Barriers to employment for people with schizophrenia. Am J Psychiatry. 2006;163:411–7.
Juckel G, Morosini PL. The new approach: psychosocial functioning as a necessary outcome criterion for therapeutic success in schizophrenia. Curr Opin Psychiatry. 2008;21:630–9.
Nasrallah HA, Lasser R. Improving patient outcomes in schizophrenia: achieving remission. J Psychopharmacol. 2006;20:57–61.
Ventura J, Subotnik KL, Guzik LH, et al. Remission and recovery during the first outpatient year of the early course of schizophrenia. Schizophr Res. 2011;132:18–23.
National Institute for Health and Care Excellence. Psychosis and schizophrenia in adults: prevention and management. https://www.nice.org.uk/guidance/cg178 (2014). Accessed 26 Nov 2016.
Lehman AF, Lieberman JA, Dixon LB, et al. Practice guideline for the treatment of patients with schizophrenia, second edition. Am J Psychiatry. 2004;161:1–56.
Alphs L, Bossie CA, Sliwa JK, Ma YW, Turner N. Onset of efficacy with acute long-acting injectable paliperidone palmitate treatment in markedly to severely ill patients with schizophrenia: post hoc analysis of a randomized, double-blind clinical trial. Ann Gen Psychiatry. 2011;10:12.
Alphs L, Bossie CA, Sliwa JK, Fu DJ, Ma YW, Hulihan J. Paliperidone palmitate and risperidone long-acting injectable in subjects with schizophrenia recently treated with oral risperidone or other oral antipsychotics. Neuropsychiatr Dis Treat. 2013;9:341–50.
Alphs L, Benson C, Cheshire-Kinney K, et al. Real-world outcomes of paliperidone palmitate compared to daily oral antipsychotic therapy in schizophrenia: a randomized, open-label, review board-blinded 15-month study. J Clin Psychiatry. 2015;76:554–61.
Attard A, Olofinjana O, Cornelius V, Curtis V, Taylor D. Paliperidone palmitate long-acting injection—prospective year-long follow-up of use in clinical practice. Acta Psychiatr Scand. 2014;130:46–51.
Bossie CA, Fu DJ, Sliwa JK, Ma YW, Alphs L. Tolerability of initiation doses of once-monthly paliperidone palmitate in patients with recently diagnosed schizophrenia in an acute treatment trial. Ther Adv Psychopharmacol. 2011;1:111–24.
Coppola D, Liu Y, Gopal S, et al. A one-year prospective study of the safety, tolerability and pharmacokinetics of the highest available dose of paliperidone palmitate in patients with schizophrenia. BMC Psychiatry. 2012;12:26.
Fu DJ, Bossie CA, Sliwa JK, Ma YW, Alphs L. Paliperidone palmitate versus oral risperidone and risperidone long-acting injection in patients with recently diagnosed schizophrenia: a tolerability and efficacy comparison. Int Clin Psychopharmacol. 2014;29:45–55.
Gopal S, Vijapurkar U, Lim P, Morozova M, Eerdekens M, Hough D. A 52-week open-label study of the safety and tolerability of paliperidone palmitate in patients with schizophrenia. J Psychopharmacol. 2011;25:685–97.
Hargarter L, Bergmans P, Cherubin P, et al. Once-monthly paliperidone palmitate in recently diagnosed and chronic non-acute patients with schizophrenia. Expert Opin Pharmacother. 2016;17:1043–53.
Hough D, Gopal S, Vijapurkar U, Lim P, Morozova M, Eerdekens M. Paliperidone palmitate maintenance treatment in delaying the time-to-relapse in patients with schizophrenia: a randomized, double-blind, placebo-controlled study. Schizophr Res. 2010;116:107–17.
Kramer M, Litman R, Hough D, et al. Paliperidone palmitate, a potential long-acting treatment for patients with schizophrenia. Results of a randomized, double-blind, placebo-controlled efficacy and safety study. Int J Neuropsychopharmacol. 2010;13:635–47.
Markowitz M, Fu DJ, Levitan B, Gopal S, Turkoz I, Alphs L. Long-acting injectable paliperidone palmitate versus oral paliperidone extended release: a comparative analysis from two placebo-controlled relapse prevention studies. Ann Gen Psychiatry. 2013;12:22.
Pandina GJ, Lindenmayer JP, Lull J, et al. A randomized, placebo-controlled study to assess the efficacy and safety of 3 doses of paliperidone palmitate in adults with acutely exacerbated schizophrenia. J Clin Psychopharm. 2010;30:235–44.
Pandina G, Lane R, Gopal S, et al. A double-blind study of paliperidone palmitate and risperidone long-acting injectable in adults with schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35:218–26.
Schreiner A, Aadamsoo K, Altamura AC, et al. Paliperidone palmitate versus oral antipsychotics in recently diagnosed schizophrenia. Schizophr Res. 2015;169:393–9.
Schreiner A, Bergmans P, Cherubin P, et al. Paliperidone palmitate in non-acute patients with schizophrenia previously unsuccessfully treated with risperidone long-acting therapy or frequently used conventional depot antipsychotics. J Psychopharmacol. 2015;29:910–22.
Sliwa JK, Bossie CA, Ma YW, Alphs L. Effects of acute paliperidone palmitate treatment in subjects with schizophrenia recently treated with oral risperidone. Schizophr Res. 2011;132:28–34.
Taylor D, Olofinjana O. Long-acting paliperidone palmitate—interim results of an observational study of its effect on hospitalization. Int Clin Psychopharmacol. 2014;29:229–34.
Li H, Rui Q, Ning X, Xu H, Gu N. A comparative study of paliperidone palmitate and risperidone long-acting injectable therapy in schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35:1002–8.
Li H, Turkoz I, Zhang F. Efficacy and safety of once-monthly injection of paliperidone palmitate in hospitalized Asian patients with acute exacerbated schizophrenia: an open-label, prospective, noncomparative study. Neuropsychiatr Dis Treat. 2015;12:15–24.
Kwon JS, Kim SN, Han J, et al. Satisfaction of immediate or delayed switch to paliperidone palmitate in patients unsatisfied with current oral atypical antipsychotics. Int Clin Psychopharmacol. 2015;30:320–8.
Si T, Zhang K, Tang J, et al. Efficacy and safety of flexibly dosed paliperidone palmitate in Chinese patients with acute schizophrenia: an open-label, single-arm, prospective, interventional study. Neuropsychiatr Dis Treat. 2015;11:1483–92.
Takahashi N, Takahashi M, Saito T, et al. Randomized, placebo-controlled, double-blind study assessing the efficacy and safety of paliperidone palmitate in Asian patients with schizophrenia. Neuropsychiatr Dis Treat. 2013;9:1889–98.
Zhang F, Si T, Chiou CF, et al. Efficacy, safety, and impact on hospitalizations of paliperidone palmitate in recent-onset schizophrenia. Neuropsychiatr Dis Treat. 2015;11:657–68.
Morosini PL, Magliano L, Brambilla L, Ugolini S, Pioli R. Development, reliability and acceptability of a new version of the DSM-IV social and occupational social functioning assessment scale (SOFAS) to assess routine social functioning. Acta Psychiatr Scand. 2000;101:323–9.
Kawata AK, Revicki DA. Psychometric properties of the Personal and Social Performance Scale (PSP) among individuals with schizophrenia living in the community. Qual Life Res. 2008;17:1247–56.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington: American Psychiatric Association; 1994.
Alphs L, Nasrallah HA, Bossie CA, Fu DJ, Gopal S, Hough D, Turkoz I. Factors associated with relapse in schizophrenia despite adherence to long-acting injectable antipsychotic therapy. Int Clin Psychopharmacol. 2016;31(4):202–9.
Bossie CA, Turkoz I, Alphs L, Mahalchick L, Fu DJ. Paliperidone palmitate once-monthly treatment in recent onset and chronic illness patients with schizoaffective disorder. J Nerv Ment Dis. 2017;205(4):324–28.
Nasrallah H, Morosini P, Gagnon DD. Reliability, validity and ability to detect change of the personal and social performance scale in patients with stable schizophrenia. Psychiatry Res. 2008;161:213–24.
Patrick DL, Burns T, Morosini P, et al. Reliability, validity and ability to detect change of the clinician-rated Personal and Social Performance scale in patients with acute symptoms of schizophrenia. Curr Med Res Opin. 2009;25:325–38.
Hough D, Nuamah IF, Lim P, et al. Independent effect of paliperidone extended release on social functioning beyond its effect on positive and negative symptoms of schizophrenia – a mediation analysis. J Clin Psychopharmacol. 2009; 29(5):496–97.
Patrick DL, Burns T, Morosini P, et al. Measuring social functioning with the Personal and Social Performance Scale in patients with acute symptoms of schizophrenia: interpretation of results of a pooled analysis of three Phase III trials of paliperidone extended release tablets. Clin Ther. 2010;32:275–92.
Heres S, Lambert M, Vauth R. Treatment of early episode in patients with schizophrenia: the role of long acting antipsychotics. Eur Psychiatry. 2014;29(S2):1409–13.
Achilla E, McCrone P. The cost effectiveness of long-acting/extended-release antipsychotics for the treatment of schizophrenia: a systematic review of economic evaluations. Appl Health Econ Health Policy. 2013;11(2):95–106.
Stevens GL, Dawson G, Zummo J. Clinical benefits and impact of early use of long-acting injectable antipsychotics for schizophrenia. Early Interv Psychiatry. 2016;10:365–77.
Das AK, Malik A, Haddad PM. A qualitative study of the attitudes of patients in an early intervention service towards antipsychotic long-acting injections. Ther Adv Psychopharmacol. 2014;4:179–85.
Correll CU, Citrome L, Haddad PM, et al. The use of long-acting injectable antipsychotics in schizophrenia: evaluating the evidence. J Clin Psychiatry. 2016;77:1–24.
Correll C. Addressing barriers to using long-acting injectable antipsychotics and appropriately monitoring antipsychotic adverse effects. J Clin Psychiatry. 2013;74:e16.
Correll C. The role of the extended health care team in successful LAI therapy: education to overcome barriers. J Clin Psychiatry. 2014;75:e25.
Heres S, Hamann J, Kissling W, Leucht S. Attitudes of psychiatrists toward antipsychotic depot medication. J Clin Psychiatry. 2006;67:1948–53.
Kim B, Lee SH, Yang YK, Park JI, Chung YC. Long-acting injectable antipsychotics for first-episode schizophrenia: the pros and cons. Schizophr Res Treatment. 2012;2012:560836.
Acknowledgements
The studies were funded by Janssen-Cilag Asia–Pacific Medical Affairs. The sponsor provided formal review of the manuscript. The sponsor also funded the journal’s article processing charges and the open access fee. The authors thank Sandra Norris (Norris Communications Group LLC) for medical writing assistance and Ellen Baum (Janssen Research & Development LLC) for additional editorial assistance in the preparation of this manuscript. All authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors meet the International Committee of Medical Journal Editors criteria.
Disclosures
Hongyan Zhang has nothing to disclose. Ibrahim Turkoz is an employee of Janssen Research & Development LLC (Titusville, NJ, USA) and holds company stock/stock options. Maju Mathews is an employee of Janssen Research & Development LLC (Titusville, NJ, USA) and holds company stock/stock options. Jianmin Zhuo is an employee of Janssen China Research & Development Center (Shanghai, China). Wilson Tan is an employee of Janssen Pharmaceutical Companies of Johnson and Johnson (Singapore) and holds company stock/stock options. Yu Feng is an employee of Janssen Pharmaceutical Companies of Johnson and Johnson (Singapore).
Compliance with Ethics Guidelines
An independent ethics committee or institutional review board at the study sites approved the study protocol of each study, and both studies were conducted in accordance with the ethical principles that have their origin in the Declaration of Helsinki and that are consistent with good clinical practices and applicable regulatory requirements. All patients or their legally acceptable representatives provided written informed consent before the patients entered one of the studies. The authors thank the study participants, without whom these studies would not have been accomplished, as well as the following investigators for their participation in the studies: X. Chongtao, L. Huafang, Y. Jianqun, S. Jushui, M. Qiyi, and Z. Xingfu (study 1, China); Y.-C. Chung, J.-H. Jeong, I. Jung, J.-W. Kim, Y.-H. Kim, B.-O. Lee, J.S. Lee, K. Lee, M.S. Lee, and W.-J. Lim (study 1, Korea); R. Mohd Salleh, H. Mohd Yusof, and A.H. Sulaiman (study 1, Malaysia); Y.-M. Bai, C.-H. Chan, H.-A. Chang, T. Chen, I.-C. Cheng, T.-J. Hwang, W.-T. Kao, and T. Lu (study 1, Taiwan); S. Damodaran, S. Jespersen, R. Lakshmana, P. Farnbach, H. Hustig, J. Kulkarni, and D. Liu (study 2, Australia); W. Miles (study 2, New Zealand); H. Zhang, G. Wang, Q. Tan, H. Li, J. Fan, and J. Zhang (study 2, China); T.L.W. Lo and M.R.K. Ng (study 2, Hong Kong); C. Lee, H. Jung, I. Jung, S. Cho, I. Chee, S. Lee, B. Lee, C. Han, and J. Yoon (study 2, Korea); J. Singh Gill, M.A. Mohd Yasin, S.S. Jasmit Singh, R. Mohd Yusoff, M.D. Dalip, S. Abdul Aziz, T.S. Tuan Hadi, and M.A. Mohd Noor (study 2, Malaysia); M.M. Cardinez-Tan and B. Sta. Ana-Ponio (study 2, Philippines); C. Liu, T. Su, M. Hsieh, N. Chiu, J. Jang, and T. Tang (study 2, Taiwan); and V. Chantarasak, K. Kittiwattanagul, and W. Pansawat (study 2, Thailand).
Author Contributions
IT and HZ were involved in the design the original studies. All authors were responsible for the approach to the post hoc analyses and data interpretation, and JZ, the project statistician, oversaw data analysis. HZ enrolled patients into the studies. All authors participated in writing the manuscript and approved the final draft for submission.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Zhang, H., Turkoz, I., Zhuo, J. et al. Paliperidone Palmitate Improves and Maintains Functioning in Asia–Pacific Patients with Schizophrenia. Adv Ther 34, 2503–2517 (2017). https://doi.org/10.1007/s12325-017-0638-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-017-0638-0