Abstract
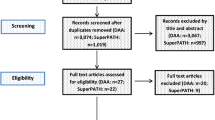
Despite the numerous studies, there is no consensus concerning the best approach for total hip arthroplasty (THA), and debates are ongoing. The purpose of this study was to perform a Bayesian network meta-analysis (NMA) comparing several approaches for primary THA. The focus was on peri-operative outcomes: surgical duration, total estimated blood loss, and length of the hospitalization. This Bayesian network meta-analysis was conducted according to the PRISMA extension statement for reporting systematic reviews incorporating network meta-analyses of health care interventions. In October 2019, the main databases were accessed. All the clinical trials comparing two or more different approaches for primary THA were assessed. For the methodology quality assessment, the PEDro score was performed. The Software STATA MP was used for the statistical analyses. The NMA was performed through the routine for Bayesian hierarchical random-effects analysis with the inverse variance statistic method for continuous variables. Data from 4843 procedures was analysed. Between patient’s demographic, good baseline comparability was found. The comparison total estimated blood loss detected statistically significant inconsistency (P = 0.01). The posterolateral approach reported the lowest value for the surgical duration. The test for overall inconsistency was statistically significant (P = 0.4). The posterolateral approach reported the shortest hospitalization length. The test for overall inconsistency was statistically significant (P = 0.9). The posterolateral approach reported shorter surgical duration and hospitalization length. Concerning the analysis of total estimated blood loss, no significant result was obtained. Data must be considered in the light of the limitations of the present study.




Similar content being viewed by others
Change history
04 November 2020
The original version of this article unfortunately contained a mistake
References
Kurtz S, Ong K, Lau E, Mowat F, Halpern M (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Jt Surg Am 89(4):780–785. https://doi.org/10.2106/JBJS.F.00222
Inacio MCS, Graves SE, Pratt NL, Roughead EE, Nemes S (2017) Increase in total joint arthroplasty projected from 2014 to 2046 in Australia: a conservative local model with international implications. Clin Orthop Relat Res 475(8):2130–2137. https://doi.org/10.1007/s11999-017-5377-7
Wu P, Liu Q, Fu M, Zhang Z, He S, Liao W, Kang Y (2018) Value of computed tomography-based three-dimensional pre-operative planning in cup placement in total hip arthroplasty with dysplastic acetabulum. J Invest Surg. https://doi.org/10.1080/08941939.2018.1444828
Hung CC, Wang CY, Fu SH, Yang RS, Hsiao FY (2018) Effects of anti-osteoporosis medications on total hip arthroplasty risks in osteoporotic patients with hip osteoarthritis in Taiwan: a nationwide cohort study. Arch Osteoporos 13(1):107. https://doi.org/10.1007/s11657-018-0522-9
Shigemura T, Yamamoto Y, Murata Y, Sato T, Tsuchiya R, Mizuki N, Toki Y, Wada Y (2018) Total hip arthroplasty after failed transtrochanteric rotational osteotomy for osteonecrosis of the femoral head: a systematic review and meta-analysis. Orthop Traumatol Surg Res. https://doi.org/10.1016/j.otsr.2018.06.019
Migliorini F, Biagini M, Rath B, Meisen N, Tingart M, Eschweiler J (2018) Total hip arthroplasty: minimally invasive surgery or not? Meta-analysis of clinical trials. Int Orthop. https://doi.org/10.1007/s00264-018-4124-3
Moretti VM, Post ZD (2017) Surgical approaches for total hip arthroplasty. Indian J Orthop 51(4):368–376. https://doi.org/10.4103/ortho.IJOrtho_317_16
Connolly KP, Kamath AF (2016) Direct anterior total hip arthroplasty: comparative outcomes and contemporary results. World J Orthop 7(2):94–101. https://doi.org/10.5312/wjo.v7.i2.94
Miller LE, Gondusky JS, Kamath AF, Boettner F, Wright J, Bhattacharyya S (2018) Influence of surgical approach on complication risk in primary total hip arthroplasty. Acta Orthop 89(3):289–294. https://doi.org/10.1080/17453674.2018.1438694
Wang Z, Hou JZ, Wu CH, Zhou YJ, Gu XM, Wang HH, Feng W, Cheng YX, Sheng X, Bao HW (2018) A systematic review and meta-analysis of direct anterior approach versus posterior approach in total hip arthroplasty. J Orthop Surg Res 13(1):229. https://doi.org/10.1186/s13018-018-0929-4
Huang SG, Chen B, Lv D, Zhang Y, Nie FF, Li W, Lv Y, Zhao HL, Liu HM (2017) Evaluation of shoulder function in clavicular fracture patients after six surgical procedures based on a network meta-analysis. Disabil Rehabil 39(2):105–112. https://doi.org/10.3109/09638288.2016.1140827
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, Ioannidis JP, Straus S, Thorlund K, Jansen JP, Mulrow C, Catala-Lopez F, Gotzsche PC, Dickersin K, Boutron I, Altman DG, Moher D (2015) The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med 162(11):777–784. https://doi.org/10.7326/M14-2385
Howick JCI, Glasziou P, Greenhalgh T, Heneghan C, Liberati A, Moschetti I, Phillips B, Thornton H, Goddard O, Hodgkinson M (2011) The 2011 Oxford CEBM levels of evidence. Oxford Centre for Evidence-Based Medicine. https://www.cebm.net/index.aspx?o=5653. Accessed Oct 2019
de Morton NA (2009) The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother 55(2):129–133
Chaimani A, Higgins JP, Mavridis D, Spyridonos P, Salanti G (2013) Graphical tools for network meta-analysis in STATA. PLoS One 8(10):e76654. https://doi.org/10.1371/journal.pone.0076654
Alecci V, Valente M, Crucil M, Minerva M, Pellegrino CM, Sabbadini DD (2011) Comparison of primary total hip replacements performed with a direct anterior approach versus the standard lateral approach: perioperative findings. J Orthop Traumatol 12(3):123–129. https://doi.org/10.1007/s10195-011-0144-0
Barrett WP, Turner SE, Leopold JP (2013) Prospective randomized study of direct anterior vs postero-lateral approach for total hip arthroplasty. J Arthroplast 28(9):1634–1638. https://doi.org/10.1016/j.arth.2013.01.034
Bergin PF, Doppelt JD, Kephart CJ, Benke MT, Graeter JH, Holmes AS, Haleem-Smith H, Tuan RS, Unger AS (2011) Comparison of minimally invasive direct anterior versus posterior total hip arthroplasty based on inflammation and muscle damage markers. J Bone Jt Surg Am 93(15):1392–1398. https://doi.org/10.2106/JBJS.J.00557
Biau DJ, Porcher R, Roren A, Babinet A, Rosencher N, Chevret S, Poiraudeau S, Anract P (2015) Neither pre-operative education or a minimally invasive procedure have any influence on the recovery time after total hip replacement. Int Orthop 39(8):1475–1481. https://doi.org/10.1007/s00264-015-2802-y
Dienstknecht T, Luring C, Tingart M, Grifka J, Sendtner E (2014) Total hip arthroplasty through the mini-incision (micro-hip) approach versus the standard transgluteal (Bauer) approach: a prospective, randomised study. J Orthop Surg Hong Kong 22(2):168–172. https://doi.org/10.1177/230949901402200210
Fink B, Mittelstaedt A (2012) Minimally invasive posterior approach for total hip arthroplasty. Orthopade 41(5):382–389. https://doi.org/10.1007/s00132-011-1893-4
Fransen B, Hoozemans M, Vos S (2016) Direct anterior approach versus posterolateral approach in total hip arthroplasty: one surgeon, two approaches. Acta Orthop Belg 82(2):240–248
Goebel S, Steinert AF, Schillinger J, Eulert J, Broscheit J, Rudert M, Noth U (2012) Reduced postoperative pain in total hip arthroplasty after minimal-invasive anterior approach. Int Orthop 36(3):491–498. https://doi.org/10.1007/s00264-011-1280-0
Goosen JH, Kollen BJ, Castelein RM, Kuipers BM, Verheyen CC (2011) Minimally invasive versus classic procedures in total hip arthroplasty: a double-blind randomized controlled trial. Clin Orthop Relat Res 469(1):200–208. https://doi.org/10.1007/s11999-010-1331-7
Gore DR, Murray MP, Sepic SB, Gardner GM (1982) Anterolateral compared to posterior approach in total hip arthroplasty: differences in component positioning, hip strength, and hip motion. Clin Orthop Relat Res 165:180–187
Ji HM, Kim KC, Lee YK, Ha YC, Koo KH (2012) Dislocation after total hip arthroplasty: a randomized clinical trial of a posterior approach and a modified lateral approach. J Arthroplast 27(3):378–385. https://doi.org/10.1016/j.arth.2011.06.007
Joseph NM, Roberts J, Mulligan MT (2017) Financial impact of total hip arthroplasty: a comparison of anterior versus posterior surgical approaches. Arthroplast Today 3(1):39–43. https://doi.org/10.1016/j.artd.2016.01.002
Laffosse JM, Accadbled F, Molinier F, Chiron P, Hocine B, Puget J (2008) Anterolateral mini-invasive versus posterior mini-invasive approach for primary total hip replacement. Comparison of exposure and implant positioning. Arch Orthop Trauma Surg 128(4):363–369. https://doi.org/10.1007/s00402-007-0385-9
Ilchmann T, Gersbach S, Zwicky L, Clauss M (2013) Standard transgluteal versus minimal invasive anterior approach in hip arthroplasty: a prospective, consecutive cohort study. Orthop Rev Pavia 5(4):e31. https://doi.org/10.4081/or.2013.e31
Martin R, Clayson PE, Troussel S, Fraser BP, Docquier PL (2011) Anterolateral minimally invasive total hip arthroplasty: a prospective randomized controlled study with a follow-up of 1 year. J Arthroplast 26(8):1362–1372. https://doi.org/10.1016/j.arth.2010.11.016
Martin CT, Pugely AJ, Gao Y, Clark CR (2013) A comparison of hospital length of stay and short-term morbidity between the anterior and the posterior approaches to total hip arthroplasty. J Arthroplast 28(5):849–854. https://doi.org/10.1016/j.arth.2012.10.029
Muller M, Tohtz S, Springer I, Dewey M, Perka C (2011) Randomized controlled trial of abductor muscle damage in relation to the surgical approach for primary total hip replacement: minimally invasive anterolateral versus modified direct lateral approach. Arch Orthop Trauma Surg 131(2):179–189. https://doi.org/10.1007/s00402-010-1117-0
Nakata K, Nishikawa M, Yamamoto K, Hirota S, Yoshikawa H (2009) A clinical comparative study of the direct anterior with mini-posterior approach: two consecutive series. J Arthroplast 24(5):698–704. https://doi.org/10.1016/j.arth.2008.04.012
Petis SM, Howard JL, Lanting BA, Marsh JD, Vasarhelyi EM (2016) In-hospital cost analysis of total hip arthroplasty: does surgical approach matter? J Arthroplast 31(1):53–58. https://doi.org/10.1016/j.arth.2015.08.034
Poehling-Monaghan KL, Krych AJ, Levy BA, Trousdale RT, Sierra RJ (2017) Female sex is a risk factor for failure of hip arthroscopy performed for acetabular retroversion. Orthop J Sports Med 5(11):2325967117737479. https://doi.org/10.1177/2325967117737479
Pogliacomi F, De Filippo M, Paraskevopoulos A, Alesci M, Marenghi P, Ceccarelli F (2012) Mini-incision direct lateral approach versus anterior mini-invasive approach in total hip replacement: results 1 year after surgery. Acta Biomed 83(2):114–121
Radoicic D, Zec V, Elassuity WI, Azab MA (2018) Patient’s perspective on direct anterior versus posterior approach total hip arthroplasty. Int Orthop 42(12):2771–2775. https://doi.org/10.1007/s00264-018-4002-z
Rathod PA, Bhalla S, Deshmukh AJ, Rodriguez JA (2014) Does fluoroscopy with anterior hip arthroplasty decrease acetabular cup variability compared with a nonguided posterior approach? Clin Orthop Relat Res 472(6):1877–1885. https://doi.org/10.1007/s11999-014-3512-2
Rittmeister M, Peters A (2006) Comparison of total hip arthroplasty via a posterior mini-incision versus a classic anterolateral approach. Orthopade 35(7):716, 718–722. https://doi.org/10.1007/s00132-006-0963-5
Rodriguez JA, Deshmukh AJ, Rathod PA, Greiz ML, Deshmane PP, Hepinstall MS, Ranawat AS (2014) Does the direct anterior approach in THA offer faster rehabilitation and comparable safety to the posterior approach? Clin Orthop Relat Res 472(2):455–463. https://doi.org/10.1007/s11999-013-3231-0
Rosenlund S, Broeng L, Holsgaard-Larsen A, Jensen C, Overgaard S (2017) Patient-reported outcome after total hip arthroplasty: comparison between lateral and posterior approach. Acta Orthop 88(3):239–247. https://doi.org/10.1080/17453674.2017.1291100
Rykov K, Reininga IHF, Sietsma MS, Knobben BAS, Ten Have B (2017) Posterolateral vs direct anterior approach in total hip arthroplasty (POLADA trial): a randomized controlled trial to assess differences in serum markers. J Arthroplast 32(12):3652–3658 e3651. https://doi.org/10.1016/j.arth.2017.07.008
Schleicher I, Haas H, Adams TS, Szalay G, Klein H, Kordelle J (2011) Minimal-invasive posterior approach for total hip arthroplasty versus standard lateral approach. Acta Orthop Belg 77(4):480–487
Sendtner E, Borowiak K, Schuster T, Woerner M, Grifka J, Renkawitz T (2011) Tackling the learning curve: comparison between the anterior, minimally invasive (micro-hip(R)) and the lateral, transgluteal (Bauer) approach for primary total hip replacement. Arch Orthop Trauma Surg 131(5):597–602. https://doi.org/10.1007/s00402-010-1174-4
Spaans AJ, van den Hout JA, Bolder SB (2012) High complication rate in the early experience of minimally invasive total hip arthroplasty by the direct anterior approach. Acta Orthop 83(4):342–346. https://doi.org/10.3109/17453674.2012.711701
Takada R, Jinno T, Miyatake K, Hirao M, Kimura A, Koga D, Yagishita K, Okawa A (2018) Direct anterior versus anterolateral approach in one-stage supine total hip arthroplasty. Focused on nerve injury: a prospective, randomized, controlled trial. J Orthop Sci 23(5):783–787. https://doi.org/10.1016/j.jos.2018.05.005
Vicente JR, Croci AT, Camargo OP (2008) Blood loss in the minimally invasive posterior approach to total hip arthroplasty: a comparative study. Clin Sao Paulo 63(3):351–356
Yang CF, Zhu QS, Han YS, Zhu JY, Wang HQ, Cong R, Zhang DW (2009) Anterolateral minimally-invasive total hip arthroplasty: a clinical comparative study of 110 cases. Zhonghua Yi Xue Za Zhi 89(1):2–6
Zawadsky MW, Paulus MC, Murray PJ, Johansen MA (2014) Early outcome comparison between the direct anterior approach and the mini-incision posterior approach for primary total hip arthroplasty: 150 consecutive cases. J Arthroplast 29(6):1256–1260. https://doi.org/10.1016/j.arth.2013.11.013
Zhang XL, Wang Q, Jiang Y, Zeng BF (2006) Minimally invasive total hip arthroplasty with anterior incision. Zhonghua Wai Ke Za Zhi 44(8):512–515
Zhao H-Y, Kang P-D, Xia Y-Y, Shi X-J, Nie Y, Pei F-X (2017) Comparison of early functional recovery following total hip arthroplasty using a direct anterior or posterolateral approach: a randomized controlled trial. Arthroplasty 32(11):3421–3428. https://doi.org/10.1016/j.arth.2017.05.056
Rosencher N, Kerkkamp HE, Macheras G, Munuera LM, Menichella G, Barton DM, Cremers S, Abraham IL (2003) Orthopedic surgery transfusion hemoglobin european overview (OSTHEO) study: blood management in elective knee and hip arthroplasty in Europe. Transfusion 43(4):459–469
Spiess BD (2004) Transfusion of blood products affects outcome in cardiac surgery. Semin Cardiothorac Vasc Anesth 8(4):267–281. https://doi.org/10.1177/108925320400800402
Rawn J (2008) The silent risks of blood transfusion. Curr Opin Anaesthesiol 21(5):664–668. https://doi.org/10.1097/ACO.0b013e32830f1fd1
Surgenor SD, Kramer RS, Olmstead EM, Ross CS, Sellke FW, Likosky DS, Marrin CA, Helm RE Jr, Leavitt BJ, Morton JR, Charlesworth DC, Clough RA, Hernandez F, Frumiento C, Benak A, DioData C, O’Connor GT, Northern New England Cardiovascular Disease Study G (2009) The association of perioperative red blood cell transfusions and decreased long-term survival after cardiac surgery. Anesth Analg 108(6):1741–1746. https://doi.org/10.1213/ane.0b013e3181a2a696
Koch CG, Li L, Duncan AI, Mihaljevic T, Cosgrove DM, Loop FD, Starr NJ, Blackstone EH (2006) Morbidity and mortality risk associated with red blood cell and blood-component transfusion in isolated coronary artery bypass grafting. Crit Care Med 34(6):1608–1616. https://doi.org/10.1097/01.CCM.0000217920.48559.D8
Shander A, Hofmann A, Gombotz H, Theusinger OM, Spahn DR (2007) Estimating the cost of blood: past, present, and future directions. Best Pract Res Clin Anaesthesiol 21(2):271–289
Fillingham YA, Ramkumar DB, Jevsevar DS, Yates AJ, Shores P, Mullen K, Bini SA, Clarke HD, Schemitsch E, Johnson RL, Memtsoudis SG, Sayeed SA, Sah AP, Della Valle C (2018) The efficacy of tranexamic acid in total hip arthroplasty: a network meta-analysis. J Arthroplast 33(10):3083–3089.e4. https://doi.org/10.1016/j.arth.2018.06.023
Zhou XD, Li J, Xiong Y, Jiang LF, Li WJ, Wu LD (2013) Do we really need closed-suction drainage in total hip arthroplasty? A meta-analysis. Int Orthop 37(11):2109–2118. https://doi.org/10.1007/s00264-013-2053-8
Zan PWW, Fan L, Wu Z, Yu X, Xu T, Li G (2016) Closed-suction drainage versus no drainage in total hip arthroplasty, a meta-analysis of randomized controlled trials. Int J Clin Exp Med 9(2):725–735
de Steiger RN, Lorimer M, Solomon M (2015) What is the learning curve for the anterior approach for total hip arthroplasty? Clin Orthop Relat Res 473(12):3860–3866. https://doi.org/10.1007/s11999-015-4565-6
D’Arrigo C, Speranza A, Monaco E, Carcangiu A, Ferretti A (2009) Learning curve in tissue sparing total hip replacement: comparison between different approaches. J Orthop Traumatol 10(1):47–54. https://doi.org/10.1007/s10195-008-0043-1
Christensen CP, Karthikeyan T, Jacobs CA (2014) Greater prevalence of wound complications requiring reoperation with direct anterior approach total hip arthroplasty. J Arthroplast 29(9):1839–1841. https://doi.org/10.1016/j.arth.2014.04.036
Muller DA, Zingg PO, Dora C (2014) Anterior minimally invasive approach for total hip replacement: five-year survivorship and learning curve. Hip Int 24(3):277–283. https://doi.org/10.5301/hipint.5000108
Epstein AM, Read JL, Hoefer M (1987) The relation of body weight to length of stay and charges for hospital services for patients undergoing elective surgery: a study of two procedures. Am J Public Health 77(8):993–997
Ogonda L, Wilson R, Archbold P, Lawlor M, Humphreys P, O’Brien S, Beverland D (2005) A minimal-incision technique in total hip arthroplasty does not improve early postoperative outcomes. A prospective, randomized, controlled trial. J Bone Jt Surg Am 87(4):701–710. https://doi.org/10.2106/jbjs.d.02645
van Aalst MJ, Oosterhof J, Nijhuis-van der Sanden MW, Schreurs BW (2014) Can the length of hospital stay after total hip arthroplasty be predicted by preoperative physical function characteristics? Am J Phys Med Rehabil 93(6):486–492. https://doi.org/10.1097/PHM.0000000000000054
Epps CD (2004) Length stay, discharge disposition, and hospital charge predictors. AORN J 79(5):975–976, 979–981, 984–997
Hayes JH, Cleary R, Gillespie WJ, Pinder IM, Sher JL (2000) Are clinical and patient assessed outcomes affected by reducing length of hospital stay for total hip arthroplasty? J Arthroplast 15(4):448–452. https://doi.org/10.1054/arth.2000.4346
Bauer R, Kerschbaumer F, Poisel S, Oberthaler W (1979) The transgluteal approach to the hip joint. Arch Orthop Trauma Surg 95(1–2):47–49. https://doi.org/10.1007/bf00379169
Pai VS (2002) A modified direct lateral approach in total hip arthroplasty. J Orthop Surg Hong Kong 10(1):35–39. https://doi.org/10.1177/230949900201000107
Berstock JR, Blom AW, Whitehouse MR (2017) A comparison of the omega and posterior approaches on patient reported function and radiological outcomes following total hip replacement. J Orthop 14(3):390–393. https://doi.org/10.1016/j.jor.2017.06.010
Funding
No external source of funding was used.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Typo in author name. Author name should read: Paolo Aretini and not Paolo Arentini.
Rights and permissions
About this article
Cite this article
Migliorini, F., Trivellas, A., Eschweiler, J. et al. Hospitalization length, surgical duration, and blood lost among the approaches for total hip arthroplasty: a Bayesian network meta-analysis. Musculoskelet Surg 104, 257–266 (2020). https://doi.org/10.1007/s12306-020-00657-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-020-00657-9