Abstract
Background
Breast cancer (BC) is the second most common cause of brain metastasis in the United States. Compared to whole brain radiation therapy (WBRT), treatment with gamma-knife radiosurgery (GKRS) offers a better chance at neurocognitive preservation. The goal of our retrospective study is to report the overall survival (OS) in patients receiving GKRS and to identify factors that improve survival outcomes.
Methods
The records of 80 patients with primary BC treated with GKRS at the Yale Comprehensive Cancer Center between 2000 and 2013 were reviewed. OS was calculated from the date of first GKRS treatment. Other factors studied were age, Karnofsky performance status (KPS), tumor subtype, having WBRT and/or surgical resection pre- or post-GKRS, and number of brain metastases treated with GKRS.
Results
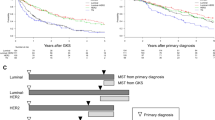
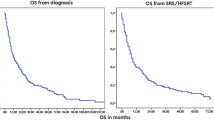
Median age was 56.2 years. OS from first GKRS was 13.1 months (95% CI 7.6–21.9). On univariate analysis, improved survival was associated with HER-2 subtype (p = 0.026), KPS score > 80 (p = 0.009), and good control of systemic disease at time of GKRS (p = 0.020). Multivariable analysis detected a significantly longer survival with HER-2 positivity (HR 0.22, 95% CI 0.06–0.76, p = 0.017) and a strong trend in patients with craniotomy prior to GKRS (HR 0.13, 95% CI 0.01–1.11, p = 0.06).
Conclusions
GKRS is a promising therapy for treating brain metastasis from BC, particularly in those with HER-2 positivity and high-performance scores even in those patients with > 5 brain metastases. Furthermore, GKRS may also be a useful adjunct to surgical resection in such patients. High rates of neurological death remain from BC brain metastases; however, and need further investigation.


Similar content being viewed by others
References
Howlader N, Noone AM, Krapcho M, Miller D, Bishop K, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA, editors. SEER Cancer Statistics Review, 1975–2013, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2013/, based on November 2015 SEER data submission, posted to the SEER web site. Accessed April 2016.
Metastatic Brain Tumors. American Brain Tumor Association, 2016. PDF.
Jaboin JJ, Ferraro DJ, Dewees TA, et al. Survival following gamma knife radiosurgery for brain metastasis from breast cancer. Radiat Oncol. 2013;8:131.
Niikura N, Hayashi N, Masuda N, et al. Treatment outcomes and prognostic factors for patients with brain metastases from breast cancer of each subtype: a multicenter retrospective analysis. Breast Cancer Res Treat. 2014;147(1):103–12.
Niwińska A, Murawska M, Pogoda K. Breast cancer brain metastases: differences in survival depending on biological subtype, RPA RTOG prognostic class and systemic treatment after whole-brain radiotherapy (WBRT). Ann Oncol. 2010;21(5):942–8.
Roehrig AT, Ferrel EA, Benincosa DA, et al. Pretreatment clinical prognostic factors for brain metastases from breast cancer treated with Gamma Knife radiosurgery. Surg Neurol Int. 2016;7(suppl 35):830–6.
Brown P, Asher A, Ballman K, et al. NCCTG N0574 (Alliance): a phase III randomized trial of whole brain radiation therapy (WBRT) in addition to radiosurgery (SRS) in patients with 1 to 3 brain metastases. J Clin Oncol. 2015;33(18_suppl):LBA4
Chang EL, Wefel JS, Hess KR, et al. Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomized controlled trial. Lancet Oncol. 2009 10(11):1037–44.
Yamamoto M. Serizawa T, Shuto T, et al. Stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): a multi-institutional prospective observational study. Lancet Oncol. 2014;15(4):387–95.
Cho E, Rubinstein L, Redman M, et al. Differentiation of overall survival by breast cancer tumor subtype following stereotactic radiosurgery for brain metastasis. J Clin Oncol. 2014;32(15_suppl):e1184.
Matsunaga S, Shuto T, Kawahara N, et al. Gamma Knife surgery for metastatic brain tumor for primary breast cancer: treatment indication based on numbers of tumor and breast cancer phenotype. J Neurosurg. 2010;113:65–72.
Dijkers EC, Oude munnink TH, Kosterink JG, et al. Biodistribution of 89Zr-trastuzumab and PET imaging of HER2-positive lesions in patients with metastatic breast cancer. Clin Pharmacol Ther. 2010;87(5):586–92.
Stemmler HJ, Schmitt M, Willems A, Bernhard H, Harbeck N, Heinemann V. Ratio of trastuzumab levels in serum and cerebrospinal fluid is altered in HER2-positive breast cancer patients with brain metastases and impairment of blood-brain barrier. Anticancer Drugs. 2007;18(1):23–8.
Kondziolka D, Martin JJ, Flickinger JC, et al. Long-term survivors after gamma knife radiosurgery for brain metastases. Cancer. 2005;104(12):2784–91.
Goyal S, Prasad D, Harrell F, Matsumoto J, Rich T, Steiner L. Gamma knife surgery for the treatment of intracranial metastases from breast cancer. J Neurosurg. 2005;103(2):218–23.
Sperduto PW, Chao ST, Sneed PK, et al. Diagnosis-specific prognostic factors, indexes, and treatment outcomes for patients with newly diagnosed brain metastases: a multi-institutional analysis of 4,259 patients. Int J Radiat Oncol Biol Phys. 2010;77(3):655–61.
Sperduto PW, Kased N, Roberge D, et al. The effect of tumor subtype on survival and the graded prognostic assessment (GPA) for patients with breast cancer and brain metastases. Int J Radiat Oncol Biol Phys 2012 April 1;82(5):2111–2117.
Yamamoto M, Kawabe T, Hiquchi Y, et al. Validity of three recently proposed prognostic grading indexes for breast cancer patients with radiosurgically treated brain metastases. Int J Radiat Oncol Biol Phys. 2012;84(5):1110–5.
Kased N, Binder DK, Mcdermott MW, et al. Gamma Knife radiosurgery for brain metastases from primary breast cancer. Int J Radiat Oncol Biol Phys. 2009;75(4):1132–40.
Park J-Y, Moon K-S, Lee K-H, et al. Gamma knife radiosurgery for elderly patients with brain metastases: evaluation of scoring systems that predict survival. BMC Cancer. 2015;15:54.
Patel KR, Prabhu RS, Kandula S, et al. Intracranial control and radiographic changes with adjuvant radiation therapy for resected brain metastases: whole brain radiotherapy versus stereotactic radiosurgery alone. J NeuroOncol. 2014;120(3):657–63.
Oh BC, Pagnini PG, Wang MY, et al. Stereotactic radiosurgery: adjacent tissue injury and response after high-dose single fraction radiation: Part I—Histology, imaging and molecular events. Neurosurgery. 2007;60(1):31–44.
Chao ST, Ahluwahlia MS, Barnett GH, et al. Challenges with the diagnosis and treatment of cerebral radiation necrosis. Int J Radiat Oncol Biol Phys. 2013;87(3):449–57.
Nath SK, Sheridan AD, Rauch PJ, et al. Significance of histology in determining management of lesions regrowing after radiosurgery. J NeuroOncol. 2014;117(2):303–10.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
James B. Yu: Research funding from twenty-first Century Oncology.
About this article
Cite this article
Abu-Khalaf, M., Muralikrishnan, S., Hatzis, C. et al. Breast cancer patients with brain metastasis undergoing GKRS. Breast Cancer 26, 147–153 (2019). https://doi.org/10.1007/s12282-018-0903-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-018-0903-3