Abstract
Purpose
The aim of our work is to develop an in situ ocular gellan gum–based nanoemulsion (NE) of tamoxifen TAM as an alternative drug delivery system to the oral route for the treatment of photoreceptor degeneration disorder.
Method
Six pseudoternary phase diagrams were developed using oil (oleic acid), surfactants (Tween 80 or Tween 20), a co-surfactant (polyethylene glycol 400), and water. The particle size, polydispersity index, and zeta potential of the developed systems were all measured. The safety of ocular application of the optimum system was established via in vivo histopathological investigation. To track the biodistribution of the optimum gel, iodine-131 (131I) was incorporated into the gel via coupling with TAM via direct electrophilic substitution reaction.
Results
Based on the obtained results, TAMNE-1 was chosen as the optimal system, with PS = 140.20 ± 1.50 nm, ZP = − 27.86 ± 1.13 mV, and PDI = 0.20 ± 0.00%. In vitro release displayed a prolonged and sustained release of TAMNE-1 gel compared to TAM solution (plain eye drop). Transparent in situ TAMNE-1 gel was developed after the incorporation of the TAMNE-1 system into gellan gum aqueous solution (0.3% w/w). In this study, TAM was successfully radiolabeled with 131I for subsequent evaluation of the efficacy of the developed in situ gel system (TAMNE-1 gel) in vivo. The developed TAMNE-1 gel system was nonirritant and safe and the biodistribution studies showed better retention of TAMNE-1 gel than plain TAM eye drops.
Conclusion
The developed TAMNE-1 gel is able to enhance the ocular bioavailability of TAM and can go further with clinical evaluation.
Graphic Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Photoreceptor degeneration is a common feature in retinal disorders and contributes to photoreceptor death and permanent blindness [1, 2]. Photoreceptor degeneration develops in a number of retinal disorders, such as atrophic age-related macular degeneration (AMD) and diabetic maculopathy, wherein the degradation of macular photoreceptors contributes to central vision loss and RP, which leads to widespread loss of photoreceptors throughout the entire retina and complete blindness. The exact cellular mechanisms causing photoreceptor degeneration in these disorders remain unknown, and systematic therapies to delay or stop the degeneration process are still lacking [3, 4]. Typically, patients with RP and atrophic AMD currently receive no therapy and progress with time to visual problems that range from significant vision loss to complete blindness.
Studies of animal models and human diseases of photoreceptor degeneration have revealed that loss of photoreceptors is frequently associated with chronic neuroinflammatory alterations, involving raised retinal levels of proinflammatory cytokines and infiltration of retinal microglia into the photoreceptor layer, allowing them to be in close proximity to degenerating photoreceptors [5]. It was reported that these infiltrating retinal microglia play a significant role in photoreceptor degradation by phagocytosing viable photoreceptors and triggering the release of proinflammatory cytokines that potentiate photoreceptor apoptosis [6]. It was stated that factors that alter microglial phagocytic expression or activation status can significantly slow the rate of photoreceptor damage [6, 7]. Consequently, agents that can limit the contributions of microglia to photoreceptor degeneration are appealing as potential therapeutic agents, specifically if these drugs are licenced and have desirable biodistribution profiles [8].
Tamoxifen (TAM), a well-established and authorized medication, is commonly used for the therapy of metastatic breast cancer. It was reported that TAM can offer promising neuroprotection to photoreceptors in animal models of photoreceptor degeneration [9]. It was reported that TAM is able to decrease the release of inflammatory cytokines and retinal microglia activation, resulting in less microglial mediated toxicity to photoreceptors [10]. These microglial effects were linked with significant restoration of photoreceptor function and structure in models of light-induced photoreceptor deterioration as well as in a genetic model for RP. Consequently, the aim of our research was to develop an eye preparation that would increase the effectiveness and ocular delivery of TAM.
Several studies have investigated nanoemulsions (NEs) as a potential drug delivery system in ophthalmology [11]. Many NEs were developed for the ophthalmic delivery of dorzolamide [12], timolol maleate [13], and pilocarpine [14]. As mentioned, NEs have distinct physicochemical properties, including a high solubilizing potential for different drugs as well as the ability to serve as permeation enhancers to promote corneal drug delivery [15]. Moreover, the low surface tension of NEs will ensure a strong spreading effect on the cornea as well as better mixing with the precorneal film constituents, potentially improving the contact between the corneal epithelium and drug [16].
One of the most common issues with topical ophthalmic drug delivery is the rapid and severe precorneal leakage caused by high tear fluid turnover and fast drainage. As a result, traditional eye drops have a few minutes of ocular residence time and the ocular penetration of a topically applied drug is limited to around 5% [25, 26]. In situ gelling systems are able to form a sol–gel phase transition once implemented in the body, owing to a change in a physicochemical parameter such as pH, ionic strength, or temperature [28]. Consequently, they are able to prolong the residence time of the drug on the corneal surface [29]. Gellan gum has recently been recognized as a material for medicinal applications owing to its safety and biocompatibility [30, 31].
Based on these findings, the current study aimed to develop in situ ocular gellan gum–based NE gels of TAM as potential alternative delivery systems to oral therapy for the management of photoreceptor degeneration disorder. Due to their size, these NEs are supposed to be able to deliver adequate drug doses into the aqueous humor and the cornea. The developed in situ NE gels might control the release rate of the drug in a manner that eliminates the need for repeated drop instillation and enhances ocular drug bioavailability as a result of prolonged drug contact time. The in vivo evaluation of the developed gel for the propensity of ocular retention was another objective.
Materials and Methods
Materials
Tamoxifen was generously donated by El Amirya Pharmaceutical Co. (Alexandria, Egypt). Oleic acid, Tween 80, PEG 400, methanol (HPLC grade), sodium metabisulfite (Na2S2O3), and chloramine-T (CAT) were purchased from Sigma Aldrich Chemical Co. (St. Louis, MO, USA). The radioisotope production facility (RPF) of the Egyptian Atomic Energy Authority (Cairo, Egypt) provided iodine-131 (131I) as a no-carrier-added solution. Normal saline was supplied by El Nasr Pharmaceutical Chemicals Company (Al Kalyubia, Egypt). All other chemicals and solvents were of high purity and technical grade and were used exactly as provided.
Development of Tamoxifen Nanoemulsion (TAMNE) Systems
Construction of Pseudoternary Phase Diagrams
The water titration technique was used to construct twelve pseudoternary systems that were composed of oleic acid, Tween 80 or Tween 20, and PEG400 [32]. Tri-plot software (Ver. 4.1.2, D. Graham and N. Midgley, Loughborough University, Leicestershire, UK) was used to create the accompanying pseudoternary phase diagrams. Briefly, homogenous and clear mixes of oleic acid and surfactant/co-surfactant (S/CoS) mixtures (1:1, 1:2, and 1:3, respectively) spanning from 1:9 to 9:1 (w/w) were obtained by vortexing at 1400 rpm for 3 min. Following each addition of water drops, samples were allowed to equilibrate before being visually inspected for phase clarity and flowability. The samples were marked on the phase diagram as points, and the area occupied by these points was assumed to be the area of the NE. The area under the curve (AUC) representing the transparent zone was calculated by using AutoCAD software (version 16.0, Autodesk, Inc., San Rafael, CA, USA). The data was statistically analyzed using one-way analysis of variance (ANOVA) using SPSS software 19.0 (SPSS Inc., Chicago, IL, USA). The variation was found to be significant at P ≤ 0.05. The system was chosen at the acceptable ratios after defining the NE region. All three phases’ amounts were expressed in %w/w [33, 34]. The desired NE system was obtained by combining the weighted ingredients and stirring to produce a transparent and clear NE [35]. The composition of the prepared systems is shown in Table 1. All systems contained 0.5% w/v of TAM.
Characterization and Optimization of TAMNE Formulae
Determination of PS, PDI, and ZP
The mean PS, PDI, and ZP of the developed TAMNE systems were determined using Nanotrac Wave II (Malvern Instruments Ltd., Malvern, England) by means of the photon dynamic light scattering technique (DLS). All experiments were done three times at room temperature, and the average of the obtained results was reported.
Transmission Electron Microscopy (TEM)
TEM (Joel JEM 1230, Tokyo, Japan) was used to investigate the morphological characteristics of the optimum NE system (TAMNE-1). A copper grid was filled with one drop of TAMNE-1 and the excess was removed with filter paper. The system was stained by using an aqueous solution of phosphotungstic acid (2% w/v) for 3 min before examination.
Preparation of Drug-Loaded NE Gel Solutions
Gellan gum concentrations of 0.1, 0.2, and 0.30% w/w were stirred in demineralized water for 10 min at 50° C. The mixture that resulted was then allowed to cool at room temperature. Following ocular application, gellan gum interacted with fluid electrolytes and tear proteins, resulting in gelling formation [36]. To mimic this condition, artificial tear fluid at a 25:7 ratio (volume of application, 25 µl; standard ocular fluid volume, 7 µl) was mixed with gellan gum solutions and gelation was inspected visually [37]. The simulated tear fluid was developed by using NaHCO3 (2.2 g), NaCl (6.8 g), KCl (1.4 g), and CaCl2.2H2O (0.084 g) in 1 l of demineralized water. These weights are equivalent to K+ (19 mM), Na+ (142 mM), and Ca2+ (0.6 mM) with an osmolality of 288 ± 5 mmol/kg [38]. A drug-loaded NE gel (0.5%, w/v) was produced by incorporating NEs into the desired gellan gum solution for gelling.
The In Vitro Release Study
The in vitro release profile of the optimum in situ gel (TAMNE-1 gel) compared to plain tamoxifen solution (TAMS) was determined using the dialysis bag method. Briefly, TAMNE-1 gel and TAMS were placed in a dialysis tube (Sigma Chemicals, USA), which was positioned in a separate beaker. The beaker was then loaded with 100 ml of the simulated tear fluid (STF), pH 7.4, and stirred continuously at 75 rpm at 37 °C ± 0.5 °C. At various time points, 1 ml was taken from the release medium to estimate the drug concentration using ultraviolet spectrophotometry at 269 nm. To replace the taken samples, the same volumes of fresh media were recruited. All experiments were performed three times.
Accelerated Physical Stability Studies
The stability of the optimum NE system (TAMNE-1) and in situ gel (TAMNE-1 gel) was studied through performing three freeze–thaw cycles (− 21 °C and 25 °C), six heating–cooling cycles (4 °C and 40 °C), and centrifugation (13,000 rpm for 30 min). After each experiment, samples were visually inspected for any signs of instability such as phase separation, changes in transparency, creaming, aggregation, coalescence, or cracking [39].
Clinical Evaluation of Rabbit Eyes
The clinical evaluation of rabbit eyes was done using a modified Draize test [40]. Testing was carried out using a scale ranging from 0 (absence) to 3 (highest) to evaluate the level of conjunctival chemosis, discharge, and conjunctival redness following ocular application of TAMNE-1 gel as described in Table 1.
Histopathological Assessment
Four male albino rabbits (2 ± 0.2 kg) were classified into two groups of the same size. Using a micropipette, the rabbits in the first group were given TAMNE-1 gel (0.5% w/v, 50 l) in two instillations at 5-min intervals. The second group received equivalent volumes of normal saline (a negative control). The tested formulation was applied to the cornea of the rabbit three times daily for 1 week. At the end of day 7, all the rabbits were decapitated. Specimens from the eyes of rabbits were obtained and preserved in 10% formalin saline for 24 h. After washing with tap water, dehydration was accomplished using serial dilutions of alcohol (absolute ethyl, methyl alcohol). Samples were purified in xylene before being fixed in paraffin in a hot air oven (56 °C) for sledge microtome segmentation at 4 μ thickness. Sections were placed on glass slides and deparaffinized, then stained with hematoxylin and eosin (H&E) and examined microscopically for histopathological abnormalities [41].
Radioiodination of TAM
In this study, TAM was radiolabeled with 131I via direct electrophilic substitution reaction, and CAT was used as an oxidizing agent [, 42, 43]. In brief, the requisite concentration of TAM was transferred to a penicillin vial, followed by the required CAT concentration. With continuous stirring, approximately 18–37 MBq of 131I was applied to the above combination. A drop of sodium metabisulfite solution (10 mg/mL H2O) was used to stop the reaction by converting excess iodine (I2) to iodide (I−) [44]. The radiochemical yield percentage of 131I-TAM was reported by using ascending paper chromatography and paper electrophoresis [45, 46].
Paper Chromatography Analysis
A Whatman paper sheet with a 1-cm width and a 13-cm length was used to assess the labeling efficiency of 131I-TAM. In brief, about 1 to 2 µL of the reaction mixture was placed 1 cm away from the lower edge of the sheet. A mixture of methylene chloride and ethyl acetate (2:1 v/v) was used as the mobile phase. Once the mobile phase had fully developed, the sheet was dried and chopped into small pieces (each piece was 1 cm). Each piece was taken to be counted on a well-type gamma counter (Scalar Ratemeter SR7) (Nuclear Enterprises Ltd., USA). Whereas free radioiodine settles at Rf = 0–0.1, the 131I-TAM was detected at Rf = 1. The radiochemical yield percentage was calculated using the following formula:
Electrophoresis
This analysis was done by using EC-3000 p-series programmable power (E.C. apparatus corporation) (Frederick, MD, USA) and chamber supply units. On a cellulose acetate sheet, about 1–2 mL of the preparation was placed 12 cm away from the cathode side of the paper sheet. After the separation process was completed, the sheet was dried and cut into small strips (1 cm in length). Each small strip was counted separately using a well-type gamma counter. The radiochemical yield percentage was calculated according to Eq. (1) as mentioned earlier.
Factors Influencing Radiochemical Yield Efficiency
The effects of TAM concentration (10–300 µg/mL), pH (1–9), temperature (ambient (27–60 °C), CAT concentration (10–200 µg/µL), and reaction time (5–250 min) on the radiochemical yield efficiency of 131I-TAM were investigated. The findings were statistically done by one-way ANOVA using SPSS software 19.0 (SPSS Inc., Chicago, IL, USA). Post-hoc analysis was done using Tukey’s HSD test. The difference at P ≤ 0.05 was considered significant.
In Vivo Biodistribution Precorneal Drainage
All animal experiments were compliant with the ARRIVE guidelines and were carried out in accordance with the U.K. Animals (Scientific Procedures) Act, 1986, and associated guidelines, EU Directive 2010/63/EU for animal experiments, or the National Institutes of Health guide for the care and use of laboratory animals (NIH Publications No. 8023, revised 1978). All animal procedures were approved and reviewed by the animal ethics committee of the Egyptian Atomic Energy Authority (approval no. 2021–201), which established regulations for the use of radioactivity and laboratory animals. The studies were done on male Wister albino rats (200–250 g). The animals used were kept in standard laboratory conditions with normal light and dark conditions at room temperature and furnished with water and food. Prior to and during the ocular application of the formulations, each rat was anaesthetized by injection with a ketamine/xylazine combination [47]. Sixty rats were classified into two groups of the same size; the first one (group A) received 131I-TAMNE gel, and the second one (group B) received 131I-TAMS. Each rat was then sacrificed at different time intervals (0.25, 0.50, 1, 6, and 8 h) via cervical dislocation. Various body organs were separated, and the eyeballs were enucleated from each rat. The organs were rinsed with saline to retrieve any adhering fluid or tissue and then weighed [48]. The radioactivity existing in each organ or tissue was assessed via a shielded well-type gamma scintillation counter. The findings were displayed as percentage injected dose per gram of organ (%ID/g ± S.D) in a population of six rats [49]. The level of significance was set at P ≤ 0.05.
Result and Discussion
Pseudoternary Phase Diagrams
Phase diagrams consisting of oil (oleic acid), Tween 80 or Tween 20 as surfactant, PEG400 as co-surfactant with different surfactant/co-surfactant ratios (S/CoS) (1:1, 1:2, and 1:3), and water are graphically shown in Fig. 1. The AUCs for the clear zones are accurately determined and illustrated in Fig. 2. Compared to the Tween 20 systems, the Tween 80 systems showed the largest clear zone (Fig. 2). This observation may be correlated to the hydrophilic-lipophilic balance (HLB) value of the used surfactants. Reports indicate that the solubilization potential of oil increases as the length of the hydrophobic chain increases [50, 51]. Therefore, the AUC of Tween 80 (HLB = 15.0) was higher than that of Tween 20 (HLB = 16.7). The AUC of systems developed at a ratio of 1:2 and 1:3 was lower than the AUC of systems developed at a ratio of 1:1 (Fig. 2). This may be due to the fact that the co-surfactant can be precisely encapsulated in the cavity between the surfactant molecules when the Smix ratio is 1:1 [52].
Characterization and Optimization of TAMNE Systems
Determination of PS, PDI, and ZP
The mean PS, PDI, and ZP of the formulated TAMNE systems were measured through the use of Nanotrac Wave II (Malvern Instruments, Malvern, UK). All measurements were performed three times at room temperature, and the mean values obtained were reported. The nanoscale spectrum of all systems ranged from 140.20 ± 1.50 to 370.4 ± 12.40 nm. As illustrated in Table 2, the PS values of the systems generated by the Smix ratio (1:1) were lower than those of the systems generated by the ratio (1:2). This can be explained by the fact that an excessive amount of co-surfactant causes this film to swell [53, 54]. A 1:1 Smix ratio allows co-surfactant molecules to be effectively incorporated into the cavities between the surfactant molecules [53].
The PDI results ranged from 0.20 ± 0.00 to 0.37 ± 0.00 (Table 2). Low PDI values mean that the vesicles are evenly dispersed [44]. The PDI values of the systems prepared with the Smix ratio (1:1) were lower than those prepared with ratio (1:2). The increased PDI values could be associated with the increase in PS depending on the co-surfactant concentration [55]. PS may have increased as a result of the extension of the interfacial film as described earlier [51, 53, 54].
Because of the electric repulsion between particles, systems are generally considered stable when the ZP value is about 30 mV [56]. The ZP values of the prepared systems ranged from − 9.13 ± 0.33 to − 27.86 ± 1.13 mV (Table 2). The ZP values of the systems prepared with Tween 20 were significantly lower than those prepared with Tween 80. It might be due to the fact that Tween 80 has lower HLB than Tween 20. According to De Lima et al. [57], increasing the surfactant’s HLB value lowers the ZP value. The compression of the electrical double layer around the droplets may cause the decrease in ZP value [51, 58].
Transmission Electron Microscopy (TEM)
The TEM image of TAMNE-1 (the optimal system) clearly indicates that the particles are spherical in shape and have a consistent droplet size distribution (Fig. 3). Furthermore, the PS of the particles observed using TEM was in agreement with the PS value measured using DLS by the Malvern instrument (Table 2).
TAM-Loaded Nanoemulsion Gels
The concentration of gellan gum solution was proportional to the extent of gel strength. On the other hand, low concentrations of gellan gum solution (0.1 or 0.2% w/w) failed to produce a promising gel. TAMNE-1 was added to the appropriate gellan gum solution (0.3% w/v) and then mixed with tear fluid (25:7) until clear gels were obtained.
In Vitro Drug Release Studies
The drug release profile of TAM from the developed in situ gel (TAMNES-1 gel), TAM solution (TAMS), and TAMNE-1 is illustrated in Fig. 4. The release rate of TAM from TAMNES-1 gel was significantly lower than that of TAMNE-1 and TAM solution (TAMS). The sustained release pattern of TAMNES-1 gel may be due to the increased viscosity generated with the aid of using in situ gels in the presence of tear fluid cations, particularly the divalent calcium ions [59]. This pattern of drug release confirms the controlled release behavior of the developed in situ NE gels. After 2 h, the in situ gel released 22.45% of the total drug, 60.23% after 6 h, and 88.08% after 24 h. On the other hand, there was a rapid drug release of 75.12% in the first 2 h, followed by 98.9% at 6 h in the case of TAMS (Fig. 4). The release rate of TAMNE-1 showed an initial rapid release rate (burst) followed by a constant release for the rest of the time. It showed a cumulative release of 66.34% after 2 h, 82.23% after 6 h, and 93.11% after 8 h. This initial burst effect might be attributed to small globule size and eventually higher surface area that allows a faster rate of drug release [59].
Accelerated Physical Stability Studies
When formulas were kept at − 21 °C during freeze–thaw cycles, they became frozen, but after 30 min at room temperature, clarity was restored. The formulas were also stable during heating–cooling cycles. After 30 min of centrifugation, visual examination revealed the high stability of TAMNE-1 and TAMNE-1 gel.
Clinical Evaluation
There was no rabbit with a score of 3 for each parameter after ocular administration of TAMNE-1 gel. Great caution must be given while integrating penetration enhancers because of the high sensitivity of the eye tissue to such chemicals. Excipients like surfactants are commonly used to enhance the penetration of drugs [60]. Surfactants are crucial compounds because of their toxicity and irritancy potential. Tween 80 was chosen as the surfactant in our formulation since it is extensively used in ocular preparations due to its safety [61]. Tween 80 is listed in the United States Pharmacopeia-National Formulary (USP–NF), the Japanese Pharmacopeia, and the European Pharmacopeia [17]. The safety of Tween 80 in ocular preparations was reported by Alany et al. [18]
Histopathological Assessment
There was no histopathological change in the investigated ocular tissues (cornea, iris, retina, or sclera) after treatment with TAMNE-1 gel. The cornea of rabbits showed a normal histological structure of the columnar epithelium, underlying stroma, and last endothelial layer, as shown in Fig. 5 (1a). Iris showed a normal histological structure of the epithelium and underlying stroma (Fig. 5, 2c). The retina of a rabbit’s eye showed normal inner, intermediate, and outer layers (Fig. 5, 3e). Moreover, the choroid and sclera of the rabbit eye showed normal histological structure (Fig. 5, 4g). Based on these findings, the developed gel was suggested to be a promising nonirritant system.
Micrographs of rabbit ocular tissues of rabbits treated with TAMNE-1 gel (group I) and normal saline (group II) showing normal histological structure of cornea with normal columnar epithelium and underlying stroma and last endothelial one (1 a), normal iris with normal histological structure of epithelium and underlying stroma (2 c), normal retina that showing different layers of inner and intermediate with outer one (3 e), and normal histological structure of retina, choroid, and sclera of rabbit eye (4 g)
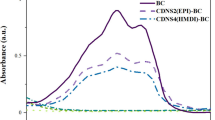
Radioiodination of TAM
TAM was effectively radiolabeled with 131I via the direct labeling method. Figure 6 depicts the effect of several factors on the percentage of radiochemical yield. The best yield (93.62 ± 0.25%) was achieved at CAT concentration of 150 µg/mL, pH 7, at ambient temperature, TAM concentration of 50 µg/ml, and reaction time of 30 min.
Factors Affecting Radiochemical Yield Percentage
Effect of Substrate Concentration
As shown in Fig. 6, the radiochemical yield percentage of 131I-TAM at a low concentration of TAM (10 µg/ml) was 71.30 ± 0.27%. At a TAM concentration of 50 g/mL, the maximum radiochemical yield percentage of 93.65 ± 0.17% was achieved. Further increases in TAM concentration beyond 50 µg/ml had no distinct influence on the radiochemical yield percentage. This is probably because 50 µg/ml of TAM is sufficient to capture all the iodonium ions produced [19, 20].
Effect of pH
It was noted that when the pH of the reaction medium was acidic (pH 3), the yield was low (73.22 ± 0.60%). This may be attributed to the predominance of iodine monochloride (ICl) species, which have a lower oxidation potential than hypochlorous acid (HOCl) species [27]. At pH 7, the maximum radiochemical yield percentage of 131I-TAM (93.65 ± 0.55%) was obtained. Increasing the pH of the reaction medium to the alkaline side (pH 9) reduced the yield to 89.22 ± 0.83%. This decrease in the radiochemical yield may be due to the formation of ClO− at high concentrations of hydroxyl ions. This further oxidizes the iodide to hypoiodite, which makes it unable to participate in the electrophilic substitution reaction [19].
Effect of Temperature
At ambient temperature, the maximum radiochemical yield percentage of 131I-TAM (93.66 ± 0.35%) was achieved (Fig. 6c). The radiochemical yield percentage of 131I-TAM was reported to be 80.35 ± 0.15 and 65.27 ± 0.16% at 40 and 60 °C, respectively. The significant drop in the labeling efficiency at higher temperatures might be attributed to the thermal decomposition of [21].
Effect of CAT Concentration
As shown in Fig. 6d, the maximum radiochemical yield percentage of 131I-TAM (93.56 ± 0.37%) was obtained at a concentration of 150 µg/ml of CAT. Above the maximum concentration (150 µg/ml), a drop in the labeling efficiency was noticed. This might be due to the formation of oxidation by-products such as chlorination or polymerization [19].
Effect of Reaction Time
As shown in Fig. 6e, the radiochemical yield at the reaction time of 5 min was low (79.50 ± 0.40%). This is probably because the reaction time between CAT and iodide was insufficient for the formation of iodide ions. At a reaction time of 30 min, the maximum radiochemical yield percentage of 131I-TAM (93.56 ± 0.43%) was achieved. Further increases in the reaction time did not significantly affect the percentage of radiochemical yield.
In Vivo Biodistribution and the Precorneal Drainage
The developed TAMNE-1 in situ gel showed good spread over the entire precorneal area immediately after administration when compared to plain drug solution. The time-dependent curve of the accumulated activity in the eye ball (time-activity curve) was generated as shown in Fig. 7. The developed TAMNE-1 in situ gel cleared slowly and persisted at the corneal surface for a long time (Fig. 7). This may be due to its ability to increase the wetting time of the cornea and increase the residence time of the drug within the eye. This enables the medicine to penetrate deeper into the internal tissues of the eye [22]. While plain drug solution (TAMS) cleared very rapidly from the eye and entered the circulatory system through the nasolacrimal drainage system, substantial activity was found in the kidney and liver after 1 h of ocular administration, whereas at 1-h post-ocular administration of 131I-TAMS, the radioactivity levels of the kidneys and liver were 4.15 ± 0.02 and 4.00 ± 0.03%, respectively, as shown in Table 3. It is worth noting that the kidney is the crucial organ for the metabolism and excretion of estrogen, as well as estrogen analogues including TAM [23]. In addition, the high hepatic uptake may be due to the presence of high concentrations of specific anti-estrogen binding sites in the liver [24].
Conclusions
This study was successful in developing a potential ocular gellan gum–based nanoemulsion gel of TAM. Transparent in situ TAMNE-1 gel was developed after the incorporation of the TAMNE-1 system into gellan gum aqueous solution (0.3% w/w). In this study, TAM was successfully radiolabeled with 131I for subsequent evaluation of the efficacy of the developed in situ gel system (TAMNE-1 gel) in vivo. The developed TAMNE-1 gel system was nonirritant and safe and showed prolonged retention in the eyeballs with a sustained release pattern. Consequently, TAMNE-1 gel provides more intense treatment of photoreceptor degeneration disorder, as well as increased patient compliance by reducing the number of applications per day. However, future studies should be done to examine the therapeutic potential of the developed TAMNE-1 in situ gel in human volunteers.
References
Congdon N, et al. Causes and prevalence of visual impairment among adults in the United States. Archives of Ophthalmology (Chicago, Ill.: 1960), 2004;122(4):p. 477–85.
Jonas JB, et al. Visual impairment and blindness due to macular diseases globally: a systematic review and meta-analysis. Am J Ophthalmol. 2014;158(4):808–15.
Holz FG, et al. Geographic atrophy: clinical features and potential therapeutic approaches. Ophthalmology. 2014;121(5):1079–91.
Wert KJ, Lin JH, Tsang SH. General pathophysiology in retinal degeneration. Cell-Based Therapy for Retinal Degenerative Disease. 2014;53:33–43.
Yoshida N, et al. Clinical evidence of sustained chronic inflammatory reaction in retinitis pigmentosa. Ophthalmology. 2013;120(1):100–5.
Zabel MK, et al. Microglial phagocytosis and activation underlying photoreceptor degeneration is regulated by CX3CL1-CX3CR1 signaling in a mouse model of retinitis pigmentosa. Glia. 2016;64(9):1479–91.
Scholz R, et al. Minocycline counter-regulates pro-inflammatory microglia responses in the retina and protects from degeneration. J Neuroinflammation. 2015;12(1):1–14.
Amantea D, Bagetta G. Drug repurposing for immune modulation in acute ischemic stroke. Curr Opin Pharmacol. 2016;26:124–30.
Lonard DM, Smith CL. Molecular perspectives on selective estrogen receptor modulators (SERMs): progress in understanding their tissue-specific agonist and antagonist actions. Steroids. 2002;67(1):15–24.
Blank T, et al. Early microglia activation precedes photoreceptor degeneration in a mouse model of CNGB1-linked retinitis pigmentosa. Front Immunol. 2018;8:1930.
Ghosh P, Murthy R. Microemulsions: a potential drug delivery system. Curr Drug Deliv. 2006;3(2):167–80.
Ammar H, et al. Development of dorzolamide hydrochloride in situ gel nanoemulsion for ocular delivery. Drug Dev Ind Pharm. 2010;36(11):1330–9.
Gallarate M, et al. Development of O/W nanoemulsions for ophthalmic administration of timolol. Int J Pharm. 2013;440(2):126–34.
Ince, I, et al. A Novel Pilocarpine Microemulsion as an ocular delivery system. 2015, Vitro.
Morsi N, et al. Nanoemulsion-based electrolyte triggered in situ gel for ocular delivery of acetazolamide. Eur J Pharm Sci. 2017;104:302–14.
Ammar HO, et al. Nanoemulsion as a potential ophthalmic delivery system for dorzolamide hydrochloride. AAPS PharmSciTech. 2009;10(3):808–19.
Yamaguchi M, et al. Formulation of an ophthalmic lipid emulsion containing an anti-inflammatory steroidal drug, difluprednate. Int J Pharm. 2005;301(1–2):121–8.
Alany RG, et al. Characterizing colloidal structures of pseudoternary phase diagrams formed by oil/water/amphiphile systems. Drug Dev Ind Pharm. 2001;27(1):31–8.
Motaleb M, Moustapha M, Ibrahim I. Synthesis and biological evaluation of 125I-nebivolol as a potential cardioselective agent for imaging β1-adrenoceptors. J Radioanal Nucl Chem. 2011;289(1):239–45.
Ibrahim I, et al. 125I labeling of clomiphene and biodistribution studies for possible use as a model in breast cancer imaging. Appl Radiat Isot. 2016;115:37–44.
Ibrahim I, et al. 125 I labeling of clomiphene and biodistribution studies for possible use as a model in breast cancer imaging. Appl Radiat Isot. 2016;115:37–44.
Klang S, Abdulrazik M, Benita* S. Influence of emulsion droplet surface charge on indomethacin ocular tissue distribution. Pharmaceut Develop Technol. 2000;5(4):p. 521–32.
Muftuler FB, et al. 131I labeling of tamoxifen and biodistribution studies in rats. Appl Radiat Isot. 2008;66(2):178–87.
Strickland L, et al. Amino and iodotamoxifens: synthesis, estrogen receptor affinity and biodistribution. Drug Des Deliv. 1990;6(3):195–212.
Kumar S, Haglund BO, Himmelstein KJ. In situ-forming gels for ophthalmic drug delivery. J Ocul Pharmacol. 1994;10:47–56.
Gaudana R, Jwala J, Boddu SH, Mitra AK. Recent perspectives in ocular drug delivery. Pharm Res. 2009;26:1197–216.
Mushtaq S, et al. Critical analysis of radioiodination techniques for micro and macro organic molecules. J Radioanal Nucl Chem. 2016;309(2):859–89.
Robinson JR, Mlynek GM. Bioadhesive and phase-change polymers for ocular drug delivery. Adv Drug Deliv Rev. 1995;16:45–50.
Krauland AH, Leitner VM, Bernkop-Schnurch A. Improvement in the in situ gelling properties of deacetylated gellan gum by the immobilization of thiol groups. J Pharm Sci. 2003;92:1234–41.
Oliveira JT, et al. Gellan gum: a new biomaterial for cartilage tissue engineering applications. Journal of Biomedical Materials Research Part A: An Official Journal of The Society for Biomaterials, The Japanese Society for Biomaterials, and The Australian Society for Biomaterials and the Korean Society for Biomaterials. 2010;93(3):852–63.
Silva-Correia J, et al. Gellan gum-based hydrogels for intervertebral disc tissue-engineering applications. J Tissue Eng Regen Med. 2011;5(6):e97–107.
Ammar HO, Salama HA, Ghorab M, Mahmoud AA. Nanoemulsion as a potential ophthalmic delivery system for dorzolamide hydrochloride. AAPS Pharm Sci Tech. 2009;10:808–19.
Chandra A, Sharma P, Irchhiaya R. Microemulsion-based hydrogel formulation for transdermal delivery of dexamethasone. Asian J Pharm. 2009;3(1):30–6.
Rasal A, et al. Development and characterization of nasal mucoadhesive microemulsion of sumatriptan succinate. Indian J Novel Drug Deliv. 2010;2:103–8.
Bagley D, et al. Skin irritation: reference chemicals data bank. Toxicol in Vitro. 1996;10(1):1–6.
Rozier A, Mazuel C, Grove J, Plazonnet B. Gelrite: a novel ion-activated, insitu gelling polymer for ophthalmic vehicles. Effect on bioavailability of timolol. Int J Pharm. 1989;57:163–68.
Carlfors J, Edsman K, Petersson R, Jornving K. Rheological evaluation of Gelrite in situ gels for ophthalmic use. Eur J Pharm Sci. 1998;6:113–9.
Paulsson M, Hagerstrom H, Edsman K. Rheological studies of the gelation of deacetylated gellan gum (Gelrite) in physiological conditions. Eur J Pharm Sci. 1999;9:99–105.
Shafiq S, Shakeel F. Stability and self-nanoemulsification efficiency of ramipril nanoemulsion containing labrasol and plurol oleique. Clin Res Regul Aff. 2010;27(1):7–12.
Baeyens V, et al. Clinical evaluation of bioadhesive ophthalmic drug inserts (BODI®) for the treatment of external ocular infections in dogs. J Control Release. 2002;85(1–3):163–8.
Bancroft JD, Gamble M. Theory and practice of histological techniques. 2008: Elsevier health sciences.
Richardson VJ, et al. Properties of [99mTc] technetium-labelled liposomes in normal and tumour-bearing rats. Biochem Soc Trans. 1977;5(1):290–1.
Babbar A, Kashyap R, Chauhan U. A convenient method for the preparation of 99mTc-labelled pentavalent DMSA and its evaluation as a tumour imaging agent. J Nucl Biol Med (Turin, Italy), 1991;35(2):p. 100–04.
Aboumanei MH, et al. Design and development of microemulsion systems of a new antineoplaston A10 analog for enhanced intravenous antitumor activity: In vitro characterization, molecular docking, 125I-radiolabeling and in vivo biodistribution studies. Int J Pharm. 2018;545(1–2):240–53.
Ibrahim I, et al. 125I labeling of clomiphene and biodistribution studies for possible use as a model in breast cancer imaging. AppL Radiat Isotopes. 2016;115:37–44.
Rashed H, et al. Preparation of radioiodinated ritodrine as a potential agent for lung imaging. J Radioanal Nucl Chem. 2014;300(3):1227–33.
Hohlbaum K, et al. Impact of repeated anesthesia with ketamine and xylazine on the well-being of C57BL/6JRj mice. PloS one. 2018;13(9):p. e0203559.
Aboumanei MH, Mahmoud AF. Design and development of a proniosomal transdermal drug delivery system of caffeine for management of migraine: In vitro characterization, 131I-radiolabeling and in vivo biodistribution studies. Process Biochem. 2020;97:201–12.
Aboumanei MH, Mahmoud AF, Motaleb MA. Formulation of chitosan coated nanoliposomes for the oral delivery of colistin sulfate: in vitro characterization, 99mTc-radiolabeling and in vivo biodistribution studies. Drug Develop Indust Pharm. 2021;p. 1–10.
Mehta SK, Kaur G, Bhasin KK. Tween-embedded microemulsions–physicochemical and spectroscopic analysis for antitubercular drugs. AAPS PharmSciTech. 2010;11(1):143–53.
Aboumanei MH, Fayez H. Intra-articular formulation of colchicine loaded nanoemulsion systems for enhanced locoregional drug delivery: In vitro characterization, 99mTc coupling and in vivo biodistribution studies. Drug Develop Industrial Pharmacy. 2021(just-accepted);p. 1–24
Kawakami K, et al. Microemulsion formulation for enhanced absorption of poorly soluble drugs. II. In vivo study. J Control Release. 2002;81(1–2):75–82.
Kale NJ, Allen LV. Studies on microemulsions using Brij 96 as surfactant and glycerin, ethylene glycol and propylene glycol as cosurfactants. Int J Pharm. 1989;57(2):87–93.
Tayel SA, et al. Promising ion-sensitive in situ ocular nanoemulsion gels of terbinafine hydrochloride: design, in vitro characterization and in vivo estimation of the ocular irritation and drug pharmacokinetics in the aqueous humor of rabbits. Int J Pharm. 2013;443(1–2):293–305.
Masarudin MJ, et al. Factors determining the stability, size distribution, and cellular accumulation of small, monodisperse chitosan nanoparticles as candidate vectors for anticancer drug delivery: application to the passive encapsulation of [14C]-doxorubicin. Nanotechnol Sci Appl. 2015;8:67–80.
Müller R, Jacobs C, Kayser O. Nanosuspensions as particulate drug formulations in therapy: rationale for development and what we can expect for the future. Adv Drug Deliv Rev. 2001;47(1):3–19.
De Lima LS, et al. Adsorption modeling of Cr, Cd and Cu on activated carbon of different origins by using fractional factorial design. Chem Eng J. 2011;166(3):881–9.
Ibrahim N, Raman IA, Yusop MR. Effects of functional group of non-ionic surfactants on the stability of emulsion. Malay J Anal Sci. 2015;19(1):p. 261–7.
Laxmi M, et al. Development and characterization of nanoemulsion as carrier for the enhancement of bioavailability of artemether. Artificial cells, nanomedicine, and biotechnology. 2015;43(5):334–44.
Lukyanov AN, Torchilin VP. Micelles from lipid derivatives of water-soluble polymers as delivery systems for poorly soluble drugs. Adv Drug Deliv Rev. 2004;56(9):1273–89.
Üstündag-Okur N, et al. Novel ofloxacin-loaded microemulsion formulations for ocular delivery. J Ocul Pharmacol Ther. 2014;30(4):319–32.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Aboumanei, M.H., Mahmoud, A.F. Development of Tamoxifen In Situ Gel Nanoemulsion for Ocular Delivery in Photoreceptor Degeneration Disorder: In Vitro Characterization, 131I-Radiolabeling, and In Vivo Biodistribution Studies. J Pharm Innov 18, 369–380 (2023). https://doi.org/10.1007/s12247-022-09638-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12247-022-09638-w