Abstract
Introduction
Despite advances in tobacco dependence treatment in the past two decades, progress has been inconsistent and slow. This paper reviews pervasive methodological issues that may contribute to the lack of timely progress in tobacco treatment science including the lack of a dynamic model or framework of the cessation process, inefficient study designs, and the use of distal outcome measures that poorly index treatment effects. The authors then present a phase-based cessation framework that partitions the cessation process into four discrete phases based on current theories of cessation and empirical data. These phases include: (1) Motivation, (2) Precessation, (3) Cessation, and (4) Maintenance.
Discussion
Within this framework, it is possible to identify phase-specific challenges that a smoker would encounter while quitting smoking, intervention components that would address these phase-specific challenges, mechanisms via which such interventions would exert their effects, and optimal outcome measures linked to these phase-specific interventions. Investigation of phase-based interventions can be accelerated by using efficient study designs that would permit more timely development of an optimal smoking cessation treatment package.

Similar content being viewed by others
Notes
There is evidence that as abstinence continues there may be intrinsic processes that thwart lapsing or relapsing and that this results in a point at which relapse becomes relatively unlikely [28]. Thus, it is possible that with very long interventions, treatment will take the majority of individuals past this point and result in very durable effect sizes (e.g., [11, 47]).
Some smokers make quit attempts in an apparently spontaneous manner. They do not select a quit day nor formally state an intention to quit [52–54]. The current model is designed to organize and assess interventions and intervention evaluations. Obviously, there would be little opportunity to organize Precessation interventions for the person who makes an unplanned quit attempt, and the framework would not, by itself, indicate the motivational factors that resulted in such a quit attempt. A theory such as the transtheoretical model would be more appropriate for that purpose.
Other bases could have been used for the demarcation of phases. For instance, the Transtheoretical model defines stages based upon both pragmatic considerations, such as a person’s willingness or attempt to quit, and upon patterns of change processes over time [51]. We also emphasize a pragmatic strategy, one based on clinically useful distinctions, in order to promote more general buy-in by diverse investigators, which might lead to greater adoption of a common framework and complementary research efforts.
References
Thornton M. The next front on the war on cancer. Wall Street Journal. 2009;Sect. A17.
Fiore MC, Jaen CR, Baker TB, et al. Treating tobacco use and dependence: 2008 update. Rockville, MD: U.S. Department of Health and Human Services, U.S. Public Health Service; 2008.
Lancaster T, Stead LF. Individual behavioural counselling for smoking cessation. Cochrane Database Syst Rev. 2005(2):CD001292.
Stead L, Perera R, Lancaster T. Telephone counselling for smoking cessation. Cochrane Database Syst Rev. 2006;3:CD002850.
Biener L, Reimer RL, Wakefield M, Szczypka G, Rigotti NA, Connolly G. Impact of smoking cessation aids and mass media among recent quitters. Am J Prev Med. 2006;30(3):217–24.
Cokkinides VE, Ward E, Jemal A, Thun MJ. Under-use of smoking-cessation treatments: Results from the National Health Interview Survey, 2000. Am J Prev Med. 2005;28(1):119–22.
Solberg LI, Asche SE, Boyle R, McCarty MC, Thoele MJ. Smoking and cessation behaviors among young adults of various educational backgrounds. Am J Public Health. 2007;97(8):1421–6.
Fiore MC, Bailey WC, Cohen SJ. Smoking cessation: Clinical practice guideline No. 18. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research; 1996.
Fiore MC, Bailey WC, Cohen SJ. Treating tobacco use and dependence: Clinical Practice Guideline. Rockville, MD: U.S. Department of Health and Human Services, U.S. Public Health Service; 2000.
Shiffman S. Smoking cessation treatment: Any progress? J Consult Clin Psychol. 1993;61(5):718–22.
Hall SM, Humfleet GL, Reus VI, Munoz RF, Cullen J. Extended nortriptyline and psychological treatment for cigarette smoking. Am J Psychiatry. 2004;161(11):2100–7.
Carroll KM. Relapse prevention as a psychosocial treatment: A review of controlled clinical trials. Exp Clin Psychopharmacol. 1996;4(1):46–54.
Lichtenstein E, Hollis J. Patient referral to a smoking cessation program: Who follows through? J Fam Pract. 1992;34(6):739–44.
Niaura R, Abrams DB. Smoking cessation: Progress, priorities, and prospectus. J Consult Clin Psychol. 2002;70(3):494–509.
Piasecki TM, Baker TB. Any further progress in smoking cessation treatment? Nicotine Tob Res. 2001;3(4):311–23.
Velicer WF, Rossi JS, Diclemente CC, Prochaska JO. A criterion measurement model for health behavior change. Addict Behav. 1996;21(5):555–84.
Friend K, Levy DT. Smoking treatment interventions and policies to promote their use: A critical review. Nicotine Tob Res. 2001;3(4):299–310.
Hollis JF, Bills R, Whitlock E, Stevens VJ, Mullooly J, Lichtenstein E. Implementing tobacco interventions in the real world of managed care. Tob Control. 2000;9(Suppl 1):i18–24.
Collins LM, Baker TB, Mermelstein RJ, et al. The Multiphase Optimization Strategy for engineering effective tobacco use interventions. Ann Behav Med. 2011 (in press).
Strecher VJ, McClure J, Alexander G, et al. Web-based smoking cessation components and tailoring depth: Results of a randomized trial. Am J Prev Med. 2008;34:373–81.
Collins LM, Murphy SA, Nair VN, Strecher VJ. A strategy for optimizing and evaluating behavioral interventions. Ann Behav Med. 2005;30(1):65–73.
Glasgow RE, Lichtenstein E, Marcus AC. Why don’t we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. Am J Public Health. 2003;93(8):1261–7.
Gonzales D, Rennard SI, Nides M, et al. Varenicline, an alpha4beta2 nicotinic acetylcholine receptor partial agonist, vs sustained-release bupropion and placebo for smoking cessation: A randomized controlled trial. JAMA. 2006;296:47–55.
Jorenby DE, Hays JT, Rigotti NA, et al. Efficacy of varenicline, an alpha4beta2 nicotinic acetylcholine receptor partial agonist, vs placebo or sustained-release bupropion for smoking cessation: A randomized controlled trial. JAMA. 2006;296(1):56–63.
Hughes JR, Keely J, Naud S. Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction. 2004;99(1):29–38.
Kenford SL, Fiore MC, Jorenby DE, Smith SS, Wetter D, Baker TB. Predicting smoking cessation. Who will quit with and without the nicotine patch. JAMA. 1994;271(8):589–94.
Hughes JR, Peters EN, Naud S. Relapse to smoking after 1 year of abstinence: A meta-analysis. Addict Behav. 2008;33(12):1516–20.
Kirshenbaum AP, Olsen DM, Bickel WK. A quantitative review of the ubiquitous relapse curve. J Subst Abuse Treat. 2009;36(1):8–17.
Carey MP, Snel DL, Carey KB, Richards CS. Self-initiated smoking cessation: A review of the empirical literature from a stress and coping perspective. Cogn Ther Res. 1989;13:323–41.
Carey MP, Kalra DL, Carey KB, Halperin S, Richards CS. Stress and unaided smoking cessation: A prospective investigation. J Consult Clin Psychol. 1993;61(5):831–8.
Weaver K, Campbell R, Mermelstein R, Wakschlag L. Pregnancy smoking in context: The influence of multiple levels of stress. Nicotine Tob Res. 2008;10(6):1065–73.
Derby CA, Lasater TM, Vass K, Gonzalez S, Carleton RA. Characteristics of smokers who attempt to quit and of those who recently succeeded. Am J Prev Med. 1994;10(6):327–34.
Homish GG, Leonard KE. Spousal influence on smoking behaviors in a US community sample of newly married couples. Soc Sci Med. 2005;61(12):2557–67.
Mermelstein R, Cohen S, Lichtenstein E, Baer JS, Kamarck T. Social support and smoking cessation and maintenance. J Consult Clin Psychol. 1986;54(4):447–53.
Shiffman S. Coping with temptations to smoke. J Consult Clin Psychol. 1984;52(2):261–7.
Shiffman S. Maintence and relapse: Coping with temptation. In: Nirenberg TD, ed. Advances in the treatment of addictive behaviors. Norwood, NJ: Ablex; 1987:353–85.
Dollar KM, Homish GG, Kozlowski LT, Leonard KE. Spousal and alcohol-related predictors of smoking cessation: A longitudinal study in a community sample of married couples. Am J Public Health. 2009;99(2):231–3.
Krall EA, Garvey AJ, Garcia RI. Smoking relapse after 2 years of abstinence: Findings from the VA Normative Aging Study. Nicotine Tob Res. 2002;4:95–100.
Bolt DM, Piper ME, McCarthy DE, et al. The Wisconsin Predicting Patients’ Relapse questionnaire. Nicotine Tob Res. 2009;11(5):481–92.
Lee CW, Kahende J. Factors associated with successful smoking cessation in the United States, 2000. Am J Public Health. 2007;97(8):1503–9.
Piasecki TM, Fiore MC, McCarthy DE, Baker TB. Have we lost our way? The need for dynamic formulations of smoking relapse proneness. Addiction. 2002;97(9):1093–108.
Loh W-Y, Piper ME, Schlam TR, et al. Which patients will succeed and fail with smoking cessation pharmacotherapies? Towards a treatment assignment algorithm. Subst Use Misuse. 2011 (in press). http://www.ncbi.nlm.nih.gov/pubmed/20397871.
Hughes JR, Callas PW. Errors in interpreting abstinence curves in studies of smoking cessation. Nicotine Tob Res. 2006;8(1):7–12.
Medioni J, Berlin I, Mallet A. Increased risk of relapse after stopping nicotine replacement therapies: A mathematical modelling approach. Addiction. 2005;100(2):247–54.
Shiffman S, Scharf DM, Shadel WG, et al. Analyzing milestones in smoking cessation: Illustration in a nicotine patch trial in adult smokers. J Consult Clin Psychol. 2006;74(2):276–85.
Japuntich SJ, Piper ME, Leventhal AM, Bolt DM, Baker TB. The effect of five smoking cessation pharmacotherapies on smoking cessation milestones. J Consult Clin Psychol. 2011 (in press).
Hall SM, Humfleet GL, Munoz RF, Reus VI, Robbins JA, Prochaska JJ. Extended treatment of older cigarette smokers. Addiction. 2009;104(6):1043–52.
Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: Toward an integrative model of change. J Consult Clin Psychol. 1983;51(3):390–5.
Prochaska JO, DiClemente CC. Stages of change in the modification of problem behaviors. Newbury Park, CA: Sage; 1992.
Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12(1):38–48.
Prochaska JO, Wright JA, Velicer WF. Evaluating theories of health behavior change: A hierarchy of criteria applied to the Transtheoretical Model. Appl Psychol. 2008;57(4):561–88.
Nielsen A, Hannibal CG, Lindekilde BE, et al. Maternal smoking predicts the risk of spontaneous abortion. Acta Obstet Gynecol Scand. 2006;85(9):1057–65.
Ockene J, Ma Y, Zapka J, Pbert L, Valentine Goins K, Stoddard A. Spontaneous cessation of smoking and alcohol use among low-income pregnant women. Am J Prev Med. 2002;23(3):150–9.
Bauld L, Chesterman J, Ferguson J, Judge K. A comparison of the effectiveness of group-based and pharmacy-led smoking cessation treatment in Glasgow. Addiction. 2009;104(2):308–16.
Piasecki TM, Fiore MC, Baker TB. Profiles in discouragement: Two studies of variability in the time course of smoking withdrawal symptoms. J Abnorm Psychol. 1998;107(2):238–51.
Piasecki TM, Niaura R, Shadel WG, et al. Smoking withdrawal dynamics in unaided quitters. J Abnorm Psychol. 2000;109(1):74–86.
Piasecki TM, Jorenby DE, Smith SS, Fiore MC, Baker TB. Smoking withdrawal dynamics: I. Abstinence distress in lapsers and abstainers. J Abnorm Psychol. 2003;112(1):3–13.
McCarthy DE, Piasecki TM, Fiore MC, Baker TB. Life before and after quitting smoking: An electronic diary study. J Abnorm Psychol. 2006;115(3):454–66.
Hughes JR. Effects of abstinence from tobacco: Etiology, animal models, epidemiology, and significance: A subjective review. Nicotine Tob Res. 2007;9(3):329–39.
Welsch SK, Smith SS, Wetter DW, Jorenby DE, Fiore MC, Baker TB. Development and validation of the Wisconsin Smoking Withdrawal Scale. Exp Clin Psychopharmacol. 1999;7(4):354–61.
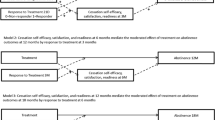
McCarthy DE, Piasecki TM, Lawrence DL, Jorenby DE, Shiffman S, Baker TB. Psychological mediators of bupropion sustained-release treatment for smoking cessation. Addiction. 2008;103(9):1521–33.
Piper ME, Federman EB, McCarthy DE, et al. Mediators of bupropion treatment effects. In: 14th Annual Meeting for the Society for Research in Nicotine and Tobacco; 2008 Feb 27–Mar 1; Portland, OR; 2008.
Etter JF, Perneger TV, Ronchi A. Distributions of smokers by stage: International comparison and association with smoking prevalence. Prev Med. 1997;26(4):580–5.
Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychol Rev. 2004;111(1):33–51.
Curry S, Wagner EH, Grothaus LC. Intrinsic and extrinsic motivation for smoking cessation. J Consult Clin Psychol. 1990;58(3):310–6.
Curry SJ, McBride C, Grothaus L, Lando H, Pirie P. Motivation for smoking cessation among pregnant women. Psychol Addict Behav. 2001;15(2):126–32.
Hatsukami D, Baker, TB. Nicotine addiction: Past and present. In: How tobacco causes disease: The biology and behavioral bases for tobacco-attributable disease: Report of the Surgeon General, U. S. Government Priority Office: Washington D.C. 2011 (in press).
McBride CM, Curry SJ, Stephens RS, Wells EA, Roffman RA, Hawkins JD. Intrinsic and extrinsic motivation for change in cigarette smokers, marijuana smokers, and cocaine users. Psychol Addict Behav. 1994;8:243–50.
Williams GC, Gagne M, Ryan RM, Deci EL. Facilitating autonomous motivation for smoking cessation. Health Psychol. 2002;21(1):40–50.
Williams GC, McGregor HA, Sharp D, et al. Testing a self-determination theory intervention for motivating tobacco cessation: Supporting autonomy and competence in a clinical trial. Health Psychol. 2006;25(1):91–101.
Hughes JR, Carpenter MJ. Does smoking reduction increase future cessation and decrease disease risk? A qualitative review. Nicotine Tob Res. 2006;8(6):739–49.
Rose JE, Herskovic JE, Trilling Y, Jarvik ME. Transdermal nicotine reduces cigarette craving and nicotine preference. Clin Pharmacol Ther. 1985;38(4):450–6.
Rose JE. New findings on nicotine addiction and treatment. Nebr Symp Motiv. 2009;55:131–41.
LeSage MG, Keyler DE, Shoeman D, Raphael D, Collins G, Pentel PR. Continuous nicotine infusion reduces nicotine self-administration in rats with 23-h/day access to nicotine. Pharmacol Biochem Behav. 2002;72(1–2):279–89.
Cinciripini PM, Lapitsky L, Seay S, Wallfisch A, Kitchens K, Van Vunakis H. The effects of smoking schedules on cessation outcome: Can we improve on common methods of gradual and abrupt nicotine withdrawal? J Consult Clin Psychol. 1995;63(3):388–99.
Cinciripini PM, Wetter DW, McClure JB. Scheduled reduced smoking: Effects on smoking abstinence and potential mechanisms of action. Addict Behav. 1997;22(6):759–67.
Hughes JR, Carpenter MJ. The feasibility of smoking reduction: An update. Addiction. 2005;100(8):1074–89.
Stead LF, Lancaster T. Interventions to reduce harm from continued tobacco use. Cochrane Database Syst Rev. 2007(3):CD005231.
Williams G, Minicucci D, Kouides R, et al. Self-determination, smoking, diet and health. Health Educ Res. 2002;17(5):512–21.
Rose JE, Behm FM, Westman EC, Kukovich P. Precessation treatment with nicotine skin patch facilitates smoking cessation. Nicotine Tob Res. 2006;8(1):89–101.
Etter JF, Laszlo E, Zellweger JP, Perrot C, Perneger TV. Nicotine replacement to reduce cigarette consumption in smokers who are unwilling to quit: A randomized trial. J Clin Psychopharmacol. 2002;22(5):487–95.
McCarthy DE, Bolt DM, Baker TB. The importance of how: A call for mechanistic research in tobacco dependence treatment studies. In: Treat T, Bootzin RI, Baker TB, eds. Psychological clinical science: Recent advances in theory and practice: Integrative perspectives in honor of Richard M McFall. New York: Lawrence Erlbaum Associates; 2007:133–63.
Piper ME, Federmen EB, McCarthy DE, et al. Using mediational models to explore the nature of tobacco motivation and tobacco treatment effects. J Abnorm Psychol. 2008;117(1):94–105.
Schuurmans MM, Diacon AH, van Biljon X, Bolliger CT. Effect of pre-treatment with nicotine patch on withdrawal symptoms and abstinence rates in smokers subsequently quitting with the nicotine patch: A randomized controlled trial. Addiction. 2004;99(5):634–40.
Collins LM, Murphy SA, Strecher V. The Multiphase Optimization Strategy (MOST) and the Sequential Multiple Assignment Randomized Trial (SMART): New methods for more potent eHealth interventions. Am J Prev Med. 2007;32(5 Suppl):S112–8.
Abrams DB, Monti PM, Carey KB, Pinto RP, Jacobus SI. Reactivity to smoking cues and relapse: Two studies of discriminant validity. Behav Res Ther. 1988;26(3):225–33.
Ferguson SG, Shiffman S. The relevance and treatment of cue-induced cravings in tobacco dependence. J Subst Abuse Treat. 2009;36(3):235–43.
Shiffman S, Gwaltney CJ, Balabanis MH, et al. Immediate antecedents of cigarette smoking: An analysis from ecological momentary assessment. J Abnorm Psychol. 2002;111(4):531–45.
Garvey AJ, Bliss RE, Hitchcock JL, Heinold JW, Rosner B. Predictors of smoking relapse among self-quitters: A report from the Normative Aging Study. Addict Behav. 1992;17(4):367–77.
Ferguson SG, Shiffman S, Gwaltney CJ. Does reducing withdrawal severity mediate nicotine patch efficacy? A randomized clinical trial. J Consult Clin Psychol. 2006;74(6):1153–61.
Rose JE, Uhl GR. Disrupting nicotine reinforcement: From cigarette to brain. In: Uhl GR, ed. Addiction reviews 2008 Annals of the New York Academy of Sciences. Malden: Blackwell Publishing; 2008:233–56.
Bullen C, Whittaker R, Walker N, Wallace-Bell M. Pre-quitting nicotine replacement therapy: Findings from a pilot study. Tobacco Induced Diseases. 2006;3(2):35–40.
Lam TH, Abdullah AS, Chan SS, Hedley AJ. Adherence to nicotine replacement therapy versus quitting smoking among Chinese smokers: A preliminary investigation. Psychopharmacology (Berl). 2005;177(4):400–8.
Waldroup WM, Gifford EV, Kalra P. Adherence to smoking cessation treatments. In: O’Donohue WT, R.Eric, eds. Promoting treatment adherence: A practical handbook for health care providers. Thousand Oaks, CA: Sage Publications, Inc.; 2006:235–52.
Donny EC, Houtsmuller E, Stitzer ML. Smoking in the absence of nicotine: Behavioral, subjective and physiological effects over 11 days. Addiction. 2007;102(2):324–34.
Donny EC, Jones M. Prolonged exposure to denicotinized cigarettes with or without transdermal nicotine. Drug Alcohol Depend. 2009;104(1–2):23–33.
Droungas A, Ehrman RN, Childress AR, O’Brien CP. Effect of smoking cues and cigarette availability on craving and smoking behavior. Addict Behav. 1995;20(5):657–73.
Rose JE, George TP. Nicotine replacement therapies and other nicotinic strategies. In: George TP, ed. Medication treatments for nicotine dependence. Boca Raton, FL: CRC Press; 2007:63–74.
Farkas AJ. When does cigarette fading increase the likelihood of future cessation? Ann Behav Med. 1999;21(1):71–6.
Juliano LM, Brandon TH. Reactivity to instructed smoking availability and environmental cues: Evidence with urge and reaction time. Exp Clin Psychopharmacol. 1998;6(1):45–53.
Levy DT, Romano E, Mumford E. The relationship of smoking cessation to sociodemographic characteristics, smoking intensity, and tobacco control policies. Nicotine Tob Res. 2005;7(3):387–96.
Nides MA, Rakos RF, Gonzales D, Murray RP, Tashkin DP, Bjornson-Benson WM. Predictors of initial smoking cessation and relapse through the first 2 years of the Lung Health Study. J Consult Clin Psychol. 1995;63(1):60–9.
McCarthy DE, Gloria R, Piper ME, Baker TB. A pilot study to test the feasibility of pre-cessation withdrawal exposure and rapid puffing among adult smokers motivated to quit. In: 15th Annual Meeting of the Society for Research on Nicotine & Tobacco; 2009 Apr; Dublin, Ireland; 2009
Piper ME, Federman EB, McCarthy DE, et al. Efficacy of bupropion alone and in combination with nicotine gum. Nicotine Tob Res. 2007;9(9):947–54.
Piper ME, Smith SS, Schlam TR, et al. A randomized placebo-controlled clinical trial of 5 smoking cessation pharmacotherapies. Arch Gen Psychiatry. 2009;66(11):1253–62.
Westman EC, Behm FM, Simel DL, Rose JE. Smoking behavior on the first day of a quit attempt predicts long-term abstinence. Arch Intern Med. 1997;157(3):335–40.
Perkins KA, Stitzer M, Lerman C. Medication screening for smoking cessation: A proposal for new methodologies. Psychopharmacology (Berl). 2006;184(3–4):628–36.
Brandon TH, Tiffany ST, Obremski KM, Baker TB. Postcessation cigarette use: The process of relapse. Addict Behav. 1990;15(2):105–14.
Shiffman S, Balbanis M. Do drinking and smoking go together? Alcohol Health Res World. 1996;20(2):107–10.
Curtin JJ, McCarthy DE, Piper ME, Baker TB. Implicit and explicit drug motivational processes: A model of boundary conditions. In: Weirs RW, Stacy AW, eds. Handbook of implicit cognition and addiction. Thousand Oaks, CA: Sage; 2006:233–50.
Gloria R, Angelos L, Schaefer HS, et al. An fMRI investigation of the impact of withdrawal on regional brain activity during nicotine anticipation. Psychophysiology. 2009;46:681–93.
Zinser MC, Fiore MC, Davidson RJ, Baker TB. Manipulating smoking motivation: Impact on an electrophysiological index of approach motivation. J Abnorm Psychol. 1999;108(2):240–54.
Brandon TH, Meade CD, Herzog TA, Chirikos TN, Webb MS, Cantor AB. Efficacy and cost-effectiveness of a minimal intervention to prevent smoking relapse: Dismantling the effects of amount of content versus contact. J Consult Clin Psychol. 2004;72(5):797–808.
Shiffman S, Paty JA, Gwaltney CJ, Dang Q. Immediate antecedents of unrestricted smoking patterns. J Abnorm Psychol. 2004;113(1):166–71.
Chaudhri N, Caggiula AR, Donny EC, Palmatier MI, Liu X, Sved AF. Complex interactions between nicotine and nonpharmacological stimuli reveal multiple roles for nicotine in reinforcement. Psychopharmacology (Berl). 2006;184(3–4):353–66.
Kenny PJ, Markou A. Conditioned nicotine withdrawal profoundly decreases the activity of brain reward systems. J Neurosci. 2005;25(26):6208–12.
Gwaltney CJ, Shiffman S, Balabanis MH, Paty JA. Dynamic self-efficacy and outcome expectancies: Prediction of smoking lapse and relapse. J Abnorm Psychol. 2005;114(4):661–75.
Brandon TH, Zelman DC, Baker TB. Effects of maintenance sessions on smoking relapse: Delaying the inevitable? J Consult Clin Psychol. 1987;55(5):780–2.
Helgason AR, Tomson T, Lund KE, Galanti R, Ahnve S, Gilljam H. Factors related to abstinence in a telephone helpline for smoking cessation. Eur J Public Health. 2004;14(3):306–10.
Tonstad S, Tonnesen P, Hajek P, Williams KE, Billing CB, Reeves KR. Effect of maintenance therapy with varenicline on smoking cessation: A randomized controlled trial. JAMA. 2006;296(1):64–71.
Schmitz JM, Sayre SL, Stotts AL, Rothfleisch J, Mooney ME. Medication compliance during a smoking cessation clinical trial: A brief intervention using MEMS feedback. J Behav Med. 2005;28(2):139–47.
Lando HA, Valanis BG, Lichtenstein E, et al. Promoting smoking abstinence in pregnant and postpartum patients: A comparison of 2 approaches. Am J Manag Care. 2001;7(7):685–93.
Hall SM, Munoz RF, Reus VI. Cognitive-behavioral intervention increases abstinence rates for depressive-history smokers. J Consult Clin Psychol. 1994;62(1):141–6.
Haynes RB, Yao X, Degani A, Kripalani S, Garg A, McDonald HP. Interventions to enhance medication adherence. Cochrane Database Syst Rev. 2005(4):CD000011.
Grabowski J, O’Brien CP, Greenstein R, Ternes J, Long M, Steinberg-Donato S. Effects of contingent payment on compliance with a naltrexone regimen. Am J Drug Alcohol Abuse. 1979;6(3):355–65.
Elixhauser A, Eisen SA, Romeis JC, Homan SM. The effects of monitoring and feedback on compliance. Med Care. 1990;28(10):882–93.
Covey LS, Glassman AH, Jiang H, et al. A randomized trial of bupropion and/or nicotine gum as maintenance treatment for preventing smoking relapse. Addiction. 2007;102(8):1292–302.
Hays JT, Hurt RD, Rigotti NA, et al. Sustained-release bupropion for pharmacologic relapse prevention after smoking cessation. A randomized, controlled trial. Ann Intern Med. 2001;135(6):423–33.
Horst WD, Klein MW, Williams D, Werder SF. Extended use of nicotine replacement therapy to maintain smoking cessation in persons with schizophrenia. Neuropsychiatric Dis Treat. 2005;1(4):349–55.
Funding: This research was supported by a grant 9P50CA143188-11 from the National Cancer Institute. Dr. Baker was supported via NCI 1K05CA139871. Dr. Collins was supported via grant P50DA10075, from the National Institute on Drug Abuse. Dr. Piper was supported by grant 1UL1RR025011 from the Clinical and Translational Science Award (CTSA) program of the National Center for Research Resources (NCRR), National Institutes of Health (NIH). Dr. Cook was supported by K08DA021311.
Potential conflicts of interest: Timothy B. Baker, Robin Mermelstein, Linda M. Collins, Megan E. Piper, Stevens S. Smith, Bruce A. Christiansen, Tanya R. Schlam, and Jessica W. Cook have no potential conflicts of interest to disclose. Douglas E. Jorenby has received research support from the National Institute on Drug Abuse, the National Cancer Institute, Pfizer, Inc., Sanofi-Synthelabo, and Nabi Biopharmaceuticals. He has received support for educational activities from the National Institute on Drug Abuse and the Veterans Administration, and consulting fees from Nabi Biopharmaceuticals. Over the last 3 years, Michael C. Fiore served as an investigator on research studies at the University of Wisconsin that were funded by Nabi Biopharmaceuticals.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s12160-011-9281-1
About this article
Cite this article
Baker, T.B., Mermelstein, R., Collins, L.M. et al. New Methods for Tobacco Dependence Treatment Research. ann. behav. med. 41, 192–207 (2011). https://doi.org/10.1007/s12160-010-9252-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12160-010-9252-y