Abstract
Background
Heart-to-mediastinum ratios (HMRs) of 123I-metaiodobenzylguanidine (MIBG) have usually been applied to prognostic evaluations of heart failure and Lewy body disease. However, whether these ratios depend on patient age has not yet been clarified using normal databases.
Methods
We analyzed 62 patients (average age 57 ± 19 years, male 45%) derived from a normal database of the Japanese Society of Nuclear Medicine working group. The HMR was calculated from early (15 min) and delayed (3–4 h) anterior planar 123I-MIBG images. All HMRs were standardized to medium-energy general purpose (MEGP) collimator equivalent conditions using conversion coefficients for the collimator types. Washout rates (WR) were also calculated, and we analyzed whether early and late HMR, and WR are associated with age.
Results
Before standardization of HMR to MEGP collimator conditions, HMR and age did not significantly correlate. However, late HMR significantly correlated with age after standardization: late HMR = − 0.0071 × age + 3.69 (r2 = 0.078, p = 0.028), indicating that a 14-year increase in age corresponded to a decrease in HMR of 0.1. Whereas the lower limit (2.5% quantile) of late HMR was 2.3 for all patients, it was 2.5 and 2.0 for those aged ≤ 63 and > 63 years, respectively. Early HMR tended to be lower in subjects with the higher age (p = 0.076), whereas WR was not affected by age.
Conclusion
While late HMR was slightly decreased in elderly patients, the lower limit of 2.2–2.3 can still be used to determine both early and late HMR.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
The prognoses of patients with heart failure (HF) and Lewy body diseases including dementia with Lewy body (DLB) and Parkinson disease have been predicted based on the uptake of 123I-metaiodobenzylguanidine (MIBG). Decreased heart-to-mediastinum ratio (HMR), such as 1.6, 1.68, and 1.74 are predictors of serious cardiac events and cardiac death among patients with HF [1,2,3,4,5]. Reports indicate that decreased HMR (< 1.74 and 2.2) is one variable for differentiating Alzheimer disease (AD) from Lewy body diseases [6,7,8,9]. Although some threshold values have been proposed for diagnostic purposes, the influence of age on 123I-MIBG parameters has not been clarified. While age is a significant predictor of cardiac events [3, 5, 10, 11] due to higher comorbidities such as diabetes, hypertension, and other coronary risk factors, the impact of age on HMR in patients with a very low likelihood of cardiac disease has not been established. Furthermore, the prognosis of patients with HF has been estimated using washout rates (WR), which also require standardization [12,13,14].
The present study aimed to determine the effect of age on HMR and WR using the Japanese Society of Nuclear Medicine (JSNM) working group normal database [15, 16], in which potential clinical causes of decreased 123I-MIBG uptake are minimized.
Methods
JSNM working group database
The JSNM working group database for 123I-MIBG included patients with a low likelihood of cardiac disease in whom cardiac MIBG study was indicated as well as routine cardiac examinations [16]. The exclusion criteria comprised patients with electrocardiographic evidence of myocardial ischemia, baseline cardiac diseases including coronary artery disease, valvular heart disease and severe arrhythmia, a history of HF, severe liver dysfunction, renal dysfunction, hypertension, diabetes and dyslipidemia managed with medications. Patients who had coronary stenosis of < 50% and those who had no indications for coronary angiography could be included if they had none of the exclusion criteria listed above. Patients with neurological disorders were also excluded.
The databases (average age, 57 ± 19 years; median age, 63 years; range 20–84 years) contained 37 patients who were assessed using low-energy (LE) collimators (50 ± 19 years, 16 males) and 25 who were assessed using low-medium-energy (LME) or medium-energy (ME) collimator (68 ± 13 years, 12 males) [17]. The HMR determined using LE collimator and a calibration phantom was corrected based on multicenter phantom experiments [18, 19].
123I-MIBG imaging
Early and late anterior planar images were acquired in 256 × 256 matrices at 15 and at 180–240 min after an intravenous injection of 111 MBq of 123I-MIBG. The acquisition time was 180–300 s. The energy for 123I was centered at 159 keV with a window of 20%. Early and late planar anterior images were assessed in this study. Early and late HMR (HMRE and HMRL) were calculated from circular and rectangular regions of interest (ROI) set on images of the heart and mediastinum, respectively, using a semi-automated ROI setting software [20].
Conversion of institutional HMR to standardized HMR
According to published phantom-based findings, average conversion coefficients (CC) of various collimators were used to calculate standardized HMR. That is
where 0.88 is a CC of ME general purpose collimator, Ki is the CC of the institutional camera-collimator, and HMRi is the institutional HMR.
Washout rate
Washout rates were calculated from early and late heart counts (HE and HL) and mediastinal counts (ME and ML) using the following formulae for WRBDC, WRDC and WRHMR:
WRBDC, with background (mediastinal counts) and time-decay corrections:
where DCF is a decay correction factor calculated as 0.5^(time [h] between early and late images/13).
WRDC, decay correction for late image:
WRHMR, WR was calculated from early and late HMR values after standardization of collimators:
Statistics
Data are expressed as means and standard deviation (SD). Goodness-of-fit to the Normal distribution was examined for distribution of HMR using the hypothesis that the data are from Normal distribution (small p values reject the hypothesis by Shapiro–Wilk test). Relationships between 123I-MIBG parameters and age were calculated using linear regression analysis. Regression lines and confidence intervals [CI] are shown when values were significant at p < 0.10. Differences in variables between groups were determined using T tests and analyses of variance. Since the median age was 63 years, the patients were divided into groups according to age ≥ 63 (n = 31) and < 63 (n = 31) years, respectively. P < 0.05 was considered significant.
Results
Before standardization, distributions of HMRE and HMRL were not Normal distribution (p = 0.014 and 0.0003, respectively), whereas after the standardization both distributions of HMRE and HMRL became Normal distributions (p = 0.99 and 0.84, respectively) by goodness-of-fit test. Table 1 summarizes the normal values determined from the JSNM working group databases. The normal values were 3.10 ± 0.43 and 3.29 ± 0.48 for HMRE and HMRL, respectively. The lower limits (2.5% quantile) of HMRE and HMRL were 2.18 and 2.26, respectively. The mean clearance from the heart or washout calculated using early and late HMR was − 6.5%, indicating that mean HMRL was higher than mean HMRE. In fact, HMRL was higher than HMRE in 50 (81%) of 62 of the patients.
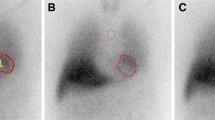
The HMRE and HMRL did not significantly correlate with age before standardization of collimators. However, a weakly positive correlation emerged after phantom-based correction to the standardized MEGP condition was applied (Fig. 1) for HMRL (p = 0.028), whereas the p value was marginal for HMRE (p = 0.076).
Relationships between age and early and late HMR. a, b Early and late HMR before correction of collimator types. c, d Early and late HMR after standardization to medium-energy general purpose collimator conditions. Red and blue symbols, female and male individuals, respectively. Unfilled and filled symbols, younger (age < 63 years) and older (age ≥ 63 years) individuals, respectively
When patients were divided into groups based on a median age (63 years), mean ages of the two groups were 41 ± 14 years and 73 ± 6 years. Goodness-of-fit test showed that HLRE and HMRL were Normal distribution for the two groups (for age < 63 year, p = 0.63 and 0.18, respectively; for age ≥ 63 year, p = 0.60 and 1.00, respectively). Both HMRE and HMRL were lower in patients aged ≥ 63 years than in those who were < 63 years (p = 0.0097 and 0.016 for HMRE and HMRL, respectively; Fig. 2). If the lower limit is defined as the 2.5% quantile of 2.3 HMRL for all patients, then 2.5 and 2.0 would be the lower limits in patients with median ages of < 63 and ≥ 63 years, respectively. The lower limit of HMRE was 2.2 for all patients, and 2.4 and 2.1 in patients with age < 63 and ≥ 63 years, respectively. Washout rates calculated using the three formulae did not significantly correlate with age (Fig. 3).
Early and late HMR in younger and older individuals. Early (a) and late (b) HMR in younger (age < 63 years) and older (≥ 63 years) individuals. Red and blue symbols, female and male individuals, respectively. Unfilled and filled symbols, younger (age < 63 years) and older (age ≥ 63 years) individuals, respectively. Box plot indicates median, 25 and 75% quartiles with whiskers at both ends. Green lines, mean values. Dotted line, HMR = 2.2 (lower limit of normal) as used in Japan using the JSNM working group database [15]
Discussion
A weak age-dependent decline in HMR was revealed in the JSNM working group 123I-MIBG normal databases. Since HMR has been used as a basis for the prognostic evaluation of patients with HF [1, 3, 5, 11] and differential diagnoses of Lewy body diseases [6, 8], this tendency should be considered to appropriately understand clinical results of 123I-MIBG uptake. The effect of age notably appeared only after standardization for collimator differences, which showed the importance of correction for collimator types when different studies include various camera-collimator types [18, 19, 21].
Although age was considered as an important factor for the prognosis of HF, the incidence of comorbidities such as diabetes, hypertension ischemic heart disease, and renal dysfunction might also increase with age. Therefore, the tendency of only age versus HMR should be examined in near-normal individuals. The JSNM working group database includes multicenter data, and patients with underlying cardiac disease and those with medications for diabetes, hypertension and neurological diseases were carefully excluded [15, 16]. Therefore, although the patients were not truly as normal as volunteers, the possibility of primary and secondary cardiac diseases was excluded as far as possible in clinical practice.
Few studies have examined HMR in near-normal individuals. As part of the ADMIRE-HF trial, a cohort comprising 94 control individuals with a 10% likelihood of having coronary artery disease according to normal stress myocardial perfusion imaging, stress echocardiography or coronary angiography findings has been investigated [22]. Correlation analyses did not identify a significant relationship between age and planar HMR values, and suggested only a slightly lower HMR for persons aged > 70 years. Another study of 180 patients with HF also found significantly lower early and late HMR compared with younger patients (p < 0.05), although values were adjusted for all remaining significant variables [23]. The uptake of 123I-MIBG with respect to HMR in a baseline study of 39 patients with cancer before undergoing chemotherapy, found a decrease in 123I-MIBG uptake with aging [24]. However, the mean HMR was 1.85 ± 0.29 (range 1.31–2.62) in that study, and much lower than that in the JSNM working group database (HMRL range 2.12–4.52). Although HMRL was significantly lower among older individuals in the JSNM working group database, the average degree of HMRL decline was ~ 0.2 over 30 years (0.07 for 10 years). Therefore, caution might be required to interpret the findings of studies that include patients with a large age range.
Medications taken by elderly patients might have affected HMR. Although a threshold HMR of 1.6 was set in the ADMIRE-HF study, the effects of several medications determined using heart failure medication scores were not significant, whereas the event group had low HMR [25]. Whether the effect of age and medications affect threshold values for the prognostic application of 123I-MIBG should be further examined.
The lower limit of HMR 2.1–2.2 has been used to differentiate DLB from AD in a Japanese multicenter study [8]. A lower limit of 2.2 remained valid for general use according to an assessment of HMR distribution in the JSNM working group database. However, in patients aged ≥ 63 years, the HMRL was lower by 0.2–0.3 compared with patients aged < 63 years. Only one 64-year-old female patient had HMR of < 2.2 in this database, and HMRE and HMRL were 2.1 and 2.0, respectively (decay and background-corrected WR = 17%). Whether this difference is critical to differentially diagnose DLB from AD has not been investigated.
Washout rates did not correlate with age. However, a standard method of calculation is desirable to correctly understand the significance of WR. The third calculation formula using early and late HMR has not been applied in Japan, but it is included in European studies [26] and some studies have used this formula when original heart and mediastinal counts were not available. In this calculation, most of the patients (81%) had higher HMRL than HMRE, which does not necessarily indicate that the actual WR calculated by the heart count shows negative values. This means that when HMRL is lower than HMRE, increased WR or abnormal sympathetic innervation should be suspected.
Immunohistochemical and histochemical analyses have also uncovered age-dependent changes in the human conduction system [27]. Initial sympathetic dominance found in the infant neural supply to the cardiac conduction system in humans is gradually replaced by sympathetic and parasympathetic co-dominance in adulthood, and a reduced density of conduction tissue innervation with aging might also be reflected in 123I-MIBG images [28].
One limitation of the present study is that the number of participants was essentially too small to evaluate physiological changes. Early HMR was not significantly affected by age (p = 0.076) while late HMR was significant (p = 0.028), which might be due to statistical power from the limited number of patients. Although truly normal volunteers were not available, the JSNM working group databases seem to have practical values to visualize age-dependent changes in aged patients using normal ranges. Another limitation was reproducibility of calculating HMR. However, we minimized inter-operator variations using semi-automatic ROI setting software [20, 29]. In this ROI setting algorithm, an operator pointed into the center of the heart, and the following processing was automatically performed. Tomographic studies might be used to integrate whole heart activity, but the present investigation was limited to planar studies.
Conclusion
An age-dependent decline in HMR, particularly late HMR, was found using JSNM working group normal 123I-MIBG databases after collimator standardization. Although the decline in HMR is relatively small, at about 0.2 over 30 years, MIBG results should be interpreted carefully when the study group includes only aged subjects such as in patients with dementia. However, in clinical practice the lower limit of 2.2 and 2.3 for early and late HMR, respectively, can still be used to determine both early and late HMR, and in patients with borderline HMR it would be important to repeat 123I-MIBG studies both in cardiology and neurology during their follow-up periods.
References
Agostini D, Verberne HJ, Burchert W, Knuuti J, Povinec P, Sambuceti G, et al. I-123-mIBG myocardial imaging for assessment of risk for a major cardiac event in heart failure patients: insights from a retrospective European multicenter study. Eur J Nucl Med Mol Imaging. 2008;35:535–46.
Nakata T, Wakabayashi T, Kyuma M, Takahashi T, Tsuchihashi K, Shimamoto K. Cardiac metaiodobenzylguanidine activity can predict the long-term efficacy of angiotensin-converting enzyme inhibitors and/or beta-adrenoceptor blockers in patients with heart failure. Eur J Nucl Med Mol Imaging. 2005;32:186–94.
Jacobson AF, Senior R, Cerqueira MD, Wong ND, Thomas GS, Lopez VA, et al. Myocardial iodine-123 meta-iodobenzylguanidine imaging and cardiac events in heart failure. Results of the prospective ADMIRE-HF (AdreView Myocardial Imaging for Risk Evaluation in Heart Failure) study. J Am Coll Cardiol. 2010;55:2212–21.
Kuwabara Y, Tamaki N, Nakata T, Yamashina S, Yamazaki J. Determination of the survival rate in patients with congestive heart failure stratified by (123)I-MIBG imaging: a meta-analysis from the studies performed in Japan. Ann Nucl Med. 2011;25:101–7.
Nakata T, Nakajima K, Yamashina S, Yamada T, Momose M, Kasama S, et al. A pooled analysis of multicenter cohort studies of 123I-mIBG imaging of sympathetic innervation for assessment of long-term prognosis in heart failure. JACC Cardiovasc Imaging. 2013;6:772 – 84.
King AE, Mintz J, Royall DR. Meta-analysis of 123I-MIBG cardiac scintigraphy for the diagnosis of Lewy body-related disorders. Mov Disord. 2011;26:1218–24.
Orimo S, Suzuki M, Inaba A, Mizusawa H. 123I-MIBG myocardial scintigraphy for differentiating Parkinson’s disease from other neurodegenerative parkinsonism: a systematic review and meta-analysis. Parkinsonism Relat Disord. 2012;18:494–500.
Yoshita M, Arai H, Arai H, Arai T, Asada T, Fujishiro H, et al. Diagnostic accuracy of 123I-meta-iodobenzylguanidine myocardial scintigraphy in dementia with Lewy bodies: a multicenter study. PLoS One. 2015;10:e0120540.
Nakajima K, Yoshita M, Matsuo S, Taki J, Kinuya S. Iodine-123-MIBG sympathetic imaging in Lewy-body diseases and related movement disorders. Q J Nucl Med Mol Imaging. 2008;52:378–87.
Nakajima K, Nakata T, Yamada T, Yamashina S, Momose M, Kasama S, et al. A prediction model for 5-year cardiac mortality in patients with chronic heart failure using 123I-metaiodobenzylguanidine imaging. Eur J Nucl Med Mol Imaging. 2014;41:1673–82.
Verschure DO, Veltman CE, Manrique A, Somsen GA, Koutelou M, Katsikis A, et al. For what endpoint does myocardial 123I-MIBG scintigraphy have the greatest prognostic value in patients with chronic heart failure? Results of a pooled individual patient data meta-analysis. Eur Heart J Cardiovasc Imaging. 2014;15:996–1003.
Tamaki S, Yamada T, Okuyama Y, Morita T, Sanada S, Tsukamoto Y, et al. Cardiac iodine-123 metaiodobenzylguanidine imaging predicts sudden cardiac death independently of left ventricular ejection fraction in patients with chronic heart failure and left ventricular systolic dysfunction: results from a comparative study with signal-averaged electrocardiogram, heart rate variability, and QT dispersion. J Am Coll Cardiol. 2009;53:426–35.
Okuda K, Nakajima K, Sugino S, Kirihara Y, Matsuo S, Taki J, et al. Development and validation of a direct-comparison method for cardiac 123I-metaiodobenzylguanidine washout rates derived from late 3-hour and 4-hour imaging. Eur J Nucl Med Mol Imaging. 2016;43:319–25.
Veltman CE, Boogers MJ, Meinardi JE, Al Younis I, Dibbets-Schneider P, Van der Wall EE, et al. Reproducibility of planar 123I-meta-iodobenzylguanidine (MIBG) myocardial scintigraphy in patients with heart failure. Eur J Nucl Med Mol Imaging. 2012;39:1599–608.
Nakajima K, Matsumoto N, Kasai T, Matsuo S, Kiso K, Okuda K. Normal values and standardization of parameters in nuclear cardiology: Japanese Society of Nuclear Medicine working group database. Ann Nucl Med. 2016;30:188–99.
Nakajima K. Normal values for nuclear cardiology: Japanese databases for myocardial perfusion, fatty acid and sympathetic imaging and left ventricular function. Ann Nucl Med. 2010;24:125–35.
Nakajima K, Okuda K, Matsuo S, Yoshita M, Taki J, Yamada M, et al. Standardization of metaiodobenzylguanidine heart to mediastinum ratio using a calibration phantom: effects of correction on normal databases and a multicentre study. Eur J Nucl Med Mol Imaging. 2012;39:113–9.
Nakajima K, Okuda K, Yoshimura M, Matsuo S, Wakabayashi H, Imanishi Y, et al. Multicenter cross-calibration of I-123 metaiodobenzylguanidine heart-to-mediastinum ratios to overcome camera-collimator variations. J Nucl Cardiol. 2014;21:970–8.
Verschure DO, Poel E, Nakajima K, Okuda K, van Eck-Smit BL, Somsen GA, et al. A European myocardial 123I-mIBG cross-calibration phantom study. J Nucl Cardiol. 2017. https://doi.org/10.1007/s12350-017-0782-6.
Okuda K, Nakajima K, Hosoya T, Ishikawa T, Konishi T, Matsubara K, et al. Semi-automated algorithm for calculating heart-to-mediastinum ratio in cardiac Iodine-123 MIBG imaging. J Nucl Cardiol. 2011;18:82–9.
Nakajima K, Verschure DO, Okuda K, Verberne HJ. Standardization of 123I-meta-iodobenzylguanidine myocardial sympathetic activity imaging: phantom calibration and clinical applications. Clin Transl Imaging. 2017;5:255–63.
Jacobson AF, Chen J, Verdes L, Folks RD, Manatunga DN, Garcia EV. Impact of age on myocardial uptake of 123I-mIBG in older adult subjects without coronary heart disease. J Nucl Cardiol. 2013;20:406–14.
Rengo G, Pagano G, Vitale DF, Formisano R, Komici K, Petraglia L, et al. Impact of aging on cardiac sympathetic innervation measured by 123I-mIBG imaging in patients with systolic heart failure. Eur J Nucl Med Mol Imaging. 2016;43:2392–400.
Estorch M, Carrio I, Berna L, Lopez-Pousa J, Torres G. Myocardial iodine-labeled metaiodobenzylguanidine 123 uptake relates to age. J Nucl Cardiol. 1995;2:126–32.
Pina IL, Carson P, Lindenfeld J, Archambault WT, Jacobson AF. Persistence of 123I-mIBG prognostic capability in relation to medical therapy in heart failure (from the ADMIRE-HF Trial). Am J Cardiol. 2017;119:434–9.
Verschure DO, de Groot JR, Mirzaei S, Gheysens O, Nakajima K, van Eck-Smit BLF, et al. Cardiac 123I-mIBG scintigraphy is associated with freedom of appropriate ICD therapy in stable chronic heart failure patients. Int J Cardiol. 2017. https://doi.org/10.1016/j.ijcard.2017.08.003.
Chow LT, Chow SS, Anderson RH, Gosling JA. Autonomic innervation of the human cardiac conduction system: changes from infancy to senility–an immunohistochemical and histochemical analysis. Anat Rec. 2001;264:169–82.
Chen W, Botvinick EH, Alavi A, Zhang Y, Yang S, Perini R, et al. Age-related decrease in cardiopulmonary adrenergic neuronal function in children as assessed by I-123 metaiodobenzylguanidine imaging. J Nucl Cardiol. 2008;15:73–9.
Klene C, Jungen C, Okuda K, Kobayashi Y, Helberg A, Mester J, et al. Influence of ROI definition on the heart-to-mediastinum ratio in planar 123I-MIBG imaging. J Nucl Cardiol. 1–9 2016.
Acknowledgements
Normal databases were created as part of the activity of a Japanese Society of Nuclear Medicine (JSNM) working group (October 2005–November 2007, October 2013–November 2015, PI: K. Nakajima). The authors appreciate Arnold Jacobson for his comments on this manuscript. The authors also thank Reo Usami for help with data analysis and Norma Foster for editorial assistance during manuscript preparation.
Funding
This study was partly funded as a JSNM working group by JSPS Grants-in-Aid for Scientific Research (C) in Japan (PI: K. Nakajima, no. 15 K09947) and FUJIFILM RI Pharma Co. Ltd. (Tokyo, Japan).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
KN and KO have collaborative research studies with FUJIFILM RI Pharma Co. Ltd. (Tokyo, Japan), which supplies 123I-MIBG in Japan.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Nakajima, K., Okuda, K., Matsuo, S. et al. Is 123I-metaiodobenzylguanidine heart-to-mediastinum ratio dependent on age? From Japanese Society of Nuclear Medicine normal database. Ann Nucl Med 32, 175–181 (2018). https://doi.org/10.1007/s12149-018-1231-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-018-1231-6