Abstract
Psychological interventions can alleviate posttraumatic stress symptoms (PTSS). However, further development of treatment approaches calls for understanding the mechanisms of change through which diverse interventions affect PTSS. We systematically searched the literature for controlled studies of mechanisms of change in psychological interventions for PTSS. We aimed to detect all empirically studied mechanisms and evaluate the level of evidence for their role in the alleviation of PTSS. We identified 34 studies, of which nine were among children. We found evidence for improvements in maladaptive posttraumatic cognitions as a general mechanism of change involved in diverse interventions, among both adults and children. We also found some preliminary evidence for increases in mindfulness as a mechanism of change in mindfulness- and spiritually-oriented interventions among adults. We found scant, mixed empirical evidence for other mechanisms of change. Notably, studies on changes in traumatic memories as a mechanism of change were lacking, despite clinical emphasis on their importance. A major limitation across reviewed studies was that most could not establish temporal order of changes in mechanisms and PTSS. Including thorough analyses of mechanisms of change beyond cognitions in all future trials and improving the reporting of findings would aid the development and implementation of even more effective interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Psychological interventions are able to alleviate posttraumatic stress symptoms (PTSS) among adults (Cusack et al. 2016) as well as children and adolescents (Dorsey et al. 2017; Gillies et al. 2016). Meta-analyses among adults find large effects for symptom reduction with trauma-focused psychological treatments, which directly address memories, thoughts, and feelings related to the traumatic event (Cusack et al. 2016; Watts et al. 2013). Trauma-focused interventions may perform better than nontrauma-focused psychological treatments or pharmacotherapy (Lee et al. 2016), but there is also some evidence for the effectiveness of nontrauma-focused interventions (e.g., Forst et al. 2014; Markowitz et al. 2015). Questions vital to advancing both the further development of treatment approaches and our understanding of recovery from PTSS include how these different treatments lead to their beneficial effects and what might explain the superior effectiveness of some interventions over others in particular contexts. Indeed, numerous authors have called for moving beyond studying mere effectiveness of psychological interventions to a more productive agenda of focusing on the mechanisms and processes by which they have their effects (Johansson and Høglend 2007; Hyman 2000; Kazdin 2007; Kraemer et al. 2002; Shapiro 1995). Here, we contribute to such an agenda by systematically reviewing all controlled studies of mechanisms of change involved in the treatment of PTSS by psychological interventions.
There are at least five main reasons for studying the mechanisms through which psychological treatments lead to symptom reduction (Kazdin 2009). First, such research allows us to separate general mechanisms from more specific ones. Identifying shared key mechanisms of change may explain how differing approaches may all lead to reduction in symptoms. At the same time, isolating more treatment-specific mechanisms can boost our confidence in particular interventions, as we are able to ascertain that their effectiveness is indeed due to the mechanisms of change they specifically target (Kazdin 2007; Overbeek et al. 2017). Such particular evidence may also help persuade clinicians to adopt empirically supported treatments (Tryon 2005).
Second, identifying the most important mechanisms of change assists us in the evaluation, optimization, and development of treatment approaches to tap into precisely such mechanisms better, improving their efficacy and increasing rates of response. In the implementation phase, understanding mechanisms of change also helps us clarify which treatment elements are essential and critical, and should be emphasized in training, and which might be more peripheral (Kazdin 2001). Put another way, understanding mechanisms may help both clinicians and researchers focus more appropriately on empirically supported principles of treatment, rather than individual treatment packages (Rosen and Davison 2003).
Third, understanding mechanisms of change can aid in identifying conditions on which the effectiveness of treatments depend and improve targeting of treatment. Patients’ susceptibility to change via specific mechanisms may differ. Thus, mechanism research may also answer questions of what works for whom and under what circumstances (Shapiro 1995).
Fourth, psychological treatments can lead to positive outcomes beyond the reduction of symptoms of individual disorders. Treatment protocols are indeed increasingly transdiagnostic. Accordingly, there is growing focus and interest in identifying mechanisms of change that may be common to several disorders and be of transdiagnostic importance (Gallagher 2017). This is highly relevant for PTSS, where comorbidity with other disorders, especially depression, anxiety, and substance abuse, is more the rule than the exception (Kessler et al. 1995; Rytwinski et al. 2013). Even beyond disorders, understanding the mechanisms of change of psychological treatments may help us clarify the connections between what happens in treatment and more wide-ranging positive changes in areas such as social functioning, physical health, or quality of life.
Finally, empirical evidence for the role, or lack thereof, of particular mechanisms in recovery from mental health symptoms is highly informative for refining or refuting models of psychopathology. For instance, if a model claims a particular mechanism to be crucial to maintaining a disorder, yet we observe alleviation of symptoms without a change in that mechanism, we have a strong suggestion that the mechanism may not be so central to the condition, after all.
Investigating Mechanisms of Change
Change and change processes in psychological interventions can be understood and studied in a variety of ways at different levels, and clear definitions are essential (Doss 2004; Zalta 2015). This review focuses exclusively on mechanisms of change, defined as changes that have occurred in the abilities, skills, functions, capacities, or characteristics of the client as the result of an intervention, which have generalized beyond the therapeutic context and have led to alleviation of symptoms (Doss 2004; see also Johansson and Høglend 2007). Thus, research on elements such as treatment components or active ingredients of treatment as well as patient responses during treatment sessions lies outside the scope of this review.
In intervention trials, mechanisms of change are typically studied as mediators of treatment effects on final outcomes, such as PTSS. A variety of methods exist to demonstrate the mediating role of a hypothesized mechanism of change in an intervention’s effects (Hayes and Scharkow 2013; MacKinnon et al. 2002; Preacher and Hayes 2008). However, not all mediators may represent mechanisms of change. Demonstrating that a purported mechanism acts as a mediator of treatment effects is just one part of establishing its role (Kazdin 2007). A mediation analysis in a controlled trial can show that the suggested mechanism is associated with both treatment and outcome and (partially) accounts for their connection, but other conditions have also been presented:
First, there must be a clear rationale for the proposed mechanism (Kraemer et al. 2002). Mechanisms must be non-trivial in that they have potential explanatory value and are theoretically sensible and/or empirically supported (Johansson and Høglend 2007). We may propose mechanisms of change for study based on over-arching theories or models of psychological disorders or more specifically on the theoretical thinking regarding therapeutic change in the particular intervention in question. Notably, higher-level theories and more intervention-specific reasoning may sometimes suggest different mechanisms (Kazdin 1999; Tryon 2005). Potential mechanisms may also be identified based on earlier empirical results on their significant role in symptom reduction, whether naturalistically or by treatment (Johansson and Høglend 2007). Studying empirically justified potential mechanisms that the intervention in question is specifically not expected to draw on for its effects may also be valuable (Kazdin 2007; Kazdin and Nock 2003) to reinforce arguments for another mechanism’s specific role. Analyzing any potential mechanisms is defensible as long as hypotheses about their role in the intervention’s effects, or lack thereof, are clearly stated. Second, evidence for the temporal sequence of change should be provided (Kazdin 2009). Without evidence that changes in the mechanism precede those in the outcome, and not, e.g., vice versa, the claim that changes in the mechanism caused changes in the outcome is seriously weakened (Johansson and Høglend 2007). In practice, this means taking measurements of both the mechanism and the outcome several times during and/or after the intervention and conducting analyses accordingly (Doss 2004). Finally, findings on mechanisms of change need to be robustly reproduced in several studies to be credible (Johansson and Høglend 2007; Kazdin 2009). For this reason, systematic reviews may be particularly useful for verifying mechanisms.
Mechanisms of Change in Treating PTSS
Two non-systematic reviews have explored psychological mechanisms of change in posttraumatic stress disorder (PTSD) treatment by interventions based on cognitive-behavioral therapy (CBT). Zalta (2015) reviewed findings on mechanisms of change in three trauma-focused interventions: cognitive processing therapy (CPT; Resick et al. 2014), cognitive therapy for PTSD (CT-PTSD; Ehlers et al. 2005) and prolonged exposure (PE; Foa et al. 2007). She found evidence from two studies that reductions in maladaptive posttraumatic cognitions (PTCs) are a mechanism of change in PE and CT-PTSD. Such PTCs have been defined as “problematic appraisals of the trauma and/or its sequelae that maintain [a] sense of current threat” (Ehlers and Clark 2000, p. 355) or as trauma-affected erroneous perceptions of the self and the world and self-blame (Foa et al. 1999). Further, two studies suggested that increased hope might be a mechanism of change involved in CPT, but could not establish the temporal order of changes in hope and PTSS.
Sripada et al. (2016) further reviewed evidence from 2013 to 2016 on the relevance of particular mechanisms, more loosely defined, to PTSD treatment by CBT interventions. They, too, found substantial evidence for changes in PTCs as a mechanism of change across treatment modalities, as well as some evidence for between-session habituation and fear reduction as a mechanism in exposure therapies, but little to no empirical evidence for emotional engagement, contextualization, or distress tolerance as mechanisms.
Beyond these two reviews, Gallagher (2017) provided an overview of evidence on mechanisms of change that might have transdiagnostic importance in CBT interventions. Besides again identifying a number of studies on negative PTCs as a mechanism of change in CBT interventions for PTSS, he found some preliminary evidence from individual studies on hope, emotion regulation, and anxiety sensitivity as other possible mechanisms with transdiagnostic relevance. Finally, Cooper et al. (2017a) reviewed evidence on mechanisms in PE, finding clear evidence for cognitive change and between-session habituation and some evidence for inhibitory learning and emotional engagement as mechanisms, but little for narrative organization or within-session habituation.
To our knowledge, no systematic reviews exist on mechanisms of change in PTSS interventions, even as systematic methods may be particularly well suited for elucidating such mechanisms (Shadish 1996; Kazdin 2007). These previous reviews have also limited themselves to CBT treatments and particular pre-defined putative mechanisms. Here, we consider the available evidence from controlled studies on all mechanisms of change that fit the definition detailed above, in all types of psychological interventions for PTSS.
The Current Study
The present review has three objectives. First, we aim to identify all mechanisms of change that have been evaluated in controlled trials of psychological interventions for PTSS, and describe the interventions, contexts, populations, and research designs they have been studied in. Second, for each mechanism identified, we describe the strength and consistency of the evidence for the role of the mechanism in the alleviation of PTSS by these interventions. Finally, based on our findings, we provide recommendations and suggestions for future research on mechanisms of change in PTSS interventions.
Method
Registration
This review was registered with PROSPERO (#CRD42017064837) with its protocol described in detail before any work on it commenced, in line with the Preferred Reporting Items for Systematic reviews and Meta-Analyses recommendation (PRISMA; Moher, Liberati, Tetzlaff, Altman, and The PRISMA Group 2009).
Eligibility Criteria
To be eligible for inclusion in this review, studies had to be 1) based on randomized controlled trials 2) of a psychological or cognitive intervention 3) delivered in person 4) with a primary or a secondary aim of alleviating PTSS, and to include 5) a PTSS outcome specified in terms of reduction in the severity or frequency of symptoms, and 6) an explicit examination of the role of a hypothesized mechanism of change in the effects of the intervention on PTSS. Studies had to be 7) prospective, 8) with at least two points of measurement (pre-post), and 9) published in a peer-reviewed academic journal. Studies on tele-health, e-medicine or other forms of “therapy at a distance” were excluded. Studies on clearly non-psychological (e.g., pharmacological or physiological) interventions were excluded. Studies on populations with traumatic brain injury were excluded.
Identification and Selection of Studies
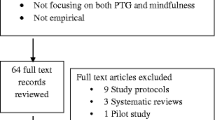
This review follows the recommendations of the PRISMA statement and guidelines where applicable (Moher et al. 2009). Figure 1 presents a PRISMA flow chart of study selection.
We conducted a comprehensive search of the electronic databases MEDLINE, PsycINFO, Scopus, Web of Science, Cochrane Central Register of Controlled Trials, and Published International Literature on Traumatic Stress for studies published by or available online on 31/08/2018. The search term was of the form (PTSD* OR posttraumatic stress* OR post-traumatic stress* OR traumatic stress*) AND (intervention* OR therap* OR psychotherap* OR treatment*) AND (mechanism* OR mediat* OR via or path*), with adaptations appropriate for each database. To maximize sensitivity, additional filters were not used. We further examined lists of references from studies meeting the inclusion criteria and from recent reviews and other major contributions in the field by hand to locate additional studies.
The first author screened titles and abstracts of studies found using the defined research strategy and those from other sources to identify studies potentially meeting the inclusion criteria. The two authors then assessed these potential studies for eligibility. In case of dissenting opinions, a third outside expert familiar with trauma research was consulted, and inclusion decided by majority decision.
Quality Assessment
We assessed the included studies for quality of evidence using a pre-developed checklist and scoring system (0–13) (Online Resource 2). We based items of the checklist on the Cochrane Handbook for Systematic Reviews of Interventions, the Jadad scale (Jadad et al. 1996) and Kazdin’s (2007) design requirements for mediation. Some items were also adopted from a systematic review by Gu et al. (2015). We classified as high quality / low risk of bias those studies that scored at least 8/13 on this scale and, crucially, were able to show that changes in mechanisms took place before changes in outcomes (item 10). Otherwise, we classified studies scoring at least 6/13 on the scale as average quality / moderate risk of bias, and those scoring 0–5 as low quality / high risk of bias.
Data Extraction
We used a data extraction form prepared beforehand. We extracted the following data from the included studies: authors, year of publication, intervention(s), control condition(s), study design, sample characteristics (sample size, age, gender distribution, nationality, type(s) of trauma experienced, share of participants with PTSD), proposed mechanism(s) of change, measures and measurement time points for outcome and mechanism(s) used in analysis, type of statistical analysis and main results.
We calculated descriptive statistics on the included studies, their characteristics, and quality. We assessed the effect of year of publication on study quality by correlation. We carried out all data processing and analyses using R 3.4.3 (R Core Team 2017).
Results
Study Selection
The search strategy identified 18,240 articles, of which 8726 were duplicates. Twelve potential articles were identified from other sources. Based on title or abstract, 9232 articles were excluded, with 294 full-text articles thus assessed for inclusion. Finally, 34 articles met the inclusion criteria and were included in the review.
Study Characteristics and Results
Online Resource 1 provides a detailed overview of the characteristics and results of the 34 studies included in the review, based on 31 separate samples, with 4117 participants in total. Sample sizes of the studies ranged widely from 24 to 483 (M = 127.8; SD = 110.4). The main characteristics of the studies are summarized in Table 1 below.
A variety of approaches to the statistical analysis of mechanisms was taken, ranging from the outdated Baron and Kenny (1986) steps approach to examinations of the indirect effect employing the product of coefficients method with bootstrapped estimates for standard errors, latent growth curve analyses, and lagged multilevel models. A common problem was lack of reported estimates of the indirect effects or path coefficients, and ambiguity in whether reported coefficients and effects were standardized or not. Notably, while most studies examined the indirect effect of participation in the intervention on PTSS via some mechanism, in some designs, it was the indirect effect of the passage of time on PTSS that was quantified, with differences between conditions examined by their moderating effects on this path. Thirty studies (88.2%) claimed evidence for at least one examined mechanism explaining a treatment’s effects on PTSS, while four found no such evidence.
Quality of Studies
Online Resource 2 presents the quality assessment of the included studies. On the scale from 0 to 13, the mean Quality Score (QS) was 6.41 (SD = 2.03), with a range of 3–10. We observed a positive correlation between year of publication and QS (r = .47, 95% CI [.15, .70], p = .005). Eleven studies could be described as providing low quality evidence (QS 0–5), 13 as average quality (QS 6–7 or QS > 8 and item 10 negative) and ten as high quality (QS > 8 and item 10 positive).
Only thirteen studies (38.2%) could assess temporal precedence in their analyses of mechanisms of change, i.e., that changes in mechanisms occurred before changes in outcomes. Studies that could not assess the temporal order of changes provide clearly weaker evidence. Thus, in describing the results below, we speak of mediation or changes in mechanisms driving improvements in symptoms only in relation to these thirteen studies. We interpret the more cross-sectional evidence as just explaining the association between treatment and outcome. Blinded assessment of both outcomes and mechanisms was also rare, present in just seven studies (20.6%). Usually, this was because measures of mechanisms were self-reports, and participants were not blinded as to the type of intervention they received.
Mechanisms of Change Identified and Evidence for Them
We may divide the putative mechanisms of change examined by the included studies into six broad categories: 1) Posttraumatic cognitions and emotions; 2) attentional processes; 3) coping strategies and behaviors; 4) traumatic memories and centrality of traumatic event; 5) mindfulness and spirituality; and 6) emotion regulation and depressive mood.
Posttraumatic Cognitions and Emotions
Eighteen studies (52.9%), of which five were of low quality, seven of average, and six of high quality, examined changes in maladaptive or problematic posttraumatic cognitions (PTCs), broadly defined, or posttraumatic emotions, as a mechanism of change in PTSS reduction. PTCs were studied as aggregates of various types of appraisals in ten studies, while three studies separated different types of appraisals related to the self as incompetent or weak, others as untrustworthy or dangerous, the world as unpredictable or threatening, or self-blame. Two studies examined hope or hopelessness. Two studies looked at the self-conscious emotions of shame and guilt, and two more at anxiety sensitivity or “fear of fear”.
Eleven of these studies were conducted among adults. Of these, seven studies provide varying levels of evidence that improvements in PTCs may act as a mechanism of change in reducing PTSS. In a detailed time-lagged analysis with mechanism and outcome measured at each session, Zalta et al. (2014; average quality) showed changes in overall PTCs to drive changes in PTSS during PE among female survivors of sexual or other assaults. Changes in PTCs were not observed in a minimal attention control group. In a similar time-lagged analysis, Cooper et al. (2017b; high quality) also found changes in PTCs to drive later reductions in PTSS during PE, but not sertraline treatment, among adult civilians exposed to mainly interpersonal traumas. Importantly, effects were not observed in the opposite direction. With female assault survivors, Foa and Rauch (2004; low quality) found PTCs to be reduced similarly in prolonged exposure (PE) treatment with and without cognitive restructuring elements, and changes in appraisals of self as incompetent and weak specifically to associate with improvements in PTSS. Changes in appraisals relating to the world or self-blame were not associated with such improvements. As both forms lead to similar changes in PTCs, this cannot be claimed to reflect mediation of treatment effects. In an all-female sample of recent assault survivors, Zoellner, Feeny, Eftekhari, and Foa (2011; low quality) found posttreatment changes in self-related appraisals to mediate the effects of a brief CBT intervention on PTSS at a medium-term follow-up, as compared with supportive counseling and repeated assessment. The CBT also affected appraisals of the world as dangerous, but changes in such beliefs did not mediate treatment effects. There was no evidence of effects on appraisals about others, self-worth or benevolence of the world.
Some studies among more specialized populations also examined PTCs as mechanisms of change. McLean et al. (2015a; high quality) studied a four-arm randomized controlled trial (RCT) among alcohol abusing adults with severe PTSS comparing PE with and without naltrexone pharmacotherapy to supportive counseling with or without the drug. Changes in overall PTCs drove changes in PTSS in all conditions except the supportive counseling and placebo condition. The indirect effect on PTSS via PTCs was strongest in the PE and naltrexone condition, but significant in the naltrexone plus placebo group as well, suggesting that this form of pharmacotherapy may also have a beneficial effect via changes in PTCs. The reverse pathway was also significant for all groups except supporting counseling plus placebo, i.e., changes in PTSS also lead to subsequent changes in PTCs. Mueser et al. (2008; average quality) compared a customized CBT program and TAU among adult civilians suffering from PTSD and a comorbid severe psychiatric disorder and found changes in overall PTCs to associate with the program’s effects on PTSS.
Most studies examined PTCs or emotions as mechanisms of change during and immediately after treatment. In one significant exception, Scher, Suvak, and Resick (2017; medium quality) demonstrated that among female survivors of rape, changes in self-, world- and other-related PTCs as well as trauma-related guilt could partially explain the effects of time on PTSS up to ten years after treatment, with similar effects seen in both CPT and PE.
Gallagher and Resick (2012; low quality) studied hope, a cognitive-emotional construct, as a mechanism of change, and found cognitive processing therapy (CPT) among female rape survivors to lead to greater decreases in hopelessness, compared with PE, and changes in hopelessness to associate with the effects of CPT on PTSS, as compared with PE. This head-to-head analysis tentatively suggests increased hope might be a specific mechanism more involved in CPT than in PE. Regarding shame and guilt, Ginzburg et al. (2009; low quality) found among adult child sexual abuse (CSA) survivor women at risk for HIV that the effects of a 6-month weekly group-based therapy on PTSS, as compared with waitlist, were partially explained by decreases in shame, but not guilt, for both trauma- and present-focused therapy.
Finally, two studies provide evidence for anxiety sensitivity as mechanism of change in reducing PTSS. In a non-clinical, but trauma-exposed sample of undergraduates, Allan, Short, Albanese, Keough, and Schmidt (2015; average quality) found the effects of a single-session anxiety sensitivity training on PTSS one month later to be mediated by reductions in overall anxiety sensitivity a week after the intervention, as well as in its more specific social concerns domain, as compared with a general education session on physical health. Studying another computerized anxiety sensitivity training among US adults with elevated risk of suicide, Short et al. (2017; high quality) found its effects, compared with repeated contact, on PTSS at one-month follow-up to be likewise mediated by changes in overall anxiety sensitivity, but also in its cognitive concerns domain, at posttreatment.
Seven studies examined PTCs or posttraumatic emotions as a mechanism of change among children and adolescents, with five providing evidence of the role of PTCs in reducing PTSS. In a small sample of underage survivors of a single traumatic event, Smith et al. (2007; low quality) found changes in overall PTCs to explain part of a CBT intervention’s effects on PTSS, as compared with a waitlist. In CT-PTSD, changes in PTCs from start of treatment to halfway through it were found to mediate treatment effects on PTSS among UK children and adolescents with fairly recent trauma, as compared with waitlist (Meiser-Stedman et al. 2017; high quality). No evidence of self-blame mediating treatment effects was found. Among female adolescent survivors of rape or CSA, McLean et al. (2015b; high quality) found changes in overall PTCs to significantly mediate improvements in PTSS during PE, but not during client-centered therapy. In contrast to the McLean et al. (2015a) study, changes in PTSS did not lead to subsequent changes in PTCs, demonstrating directional effects. For mostly female children and adolescents in Norway, Jensen et al. ( 2018; high quality) found TF-CBT to lead to greater improvements in PTCs compared with TAU. Effects of TF-CBT on posttreatment PTSS were associated with changes in PTCs, when pre-post or mid-post changes were examined, but not when pre-mid change was considered, precluding claims about direction of effect. In another mostly female sample of children and adolescents in Germany, Pfeiffer, Sachser, de Haan, Tutus, and Goldbeck (2017; average quality) also found the effects of TF-CBT on PTSS to be partly explained by changes in PTCs. However, the outcome was not controlled for pretreatment levels of PTSS, and the direction of effect could not be established.
Two studies reported negative findings among children. Among war-affected Palestinian children, a psychosocial group intervention was not found to lead to changes in PTCs, and there was thus no evidence of such changes mediating the intervention’s effects on PTSS (Kangaslampi et al. 2016; average quality). Another group-based psychosocial treatment did lead to increased hope among Indonesian schoolchildren after experiences of communal violence and conflict (Tol et al. 2010; average quality), but such increases were not associated with effects on PTSS.
Coping Strategies and Behaviors
Six studies, four of average and two of high quality, looked at changes in coping strategies or behaviors as potential mechanisms of change. Two studies provide evidence for their role, while the findings of the other four were mixed or negative. Oman and Bormann (2015; high quality) studied the role of improved self-efficacy in the effects of a six-week group-based mantram repetition programme on PTSS among older male US combat veterans, and found self-efficacy to mediate treatment effects, as compared with TAU. However, in this otherwise high-quality study, self-efficacy was assessed by just a single question referring to the participant’s ability to manage PTSD symptoms. Sikkema et al. (2013; average quality) found that among HIV-positive survivors of CSA, the effects of a group-based coping intervention on PTSS, as compared with a therapeutic support group, were associated with reductions in the use of avoidant coping. With Chinese HIV-positive men who have sex with men, Ye, Yu, Zhu, Chen, and Lin (2018; average quality) found a group-based coping intervention to lead to more use of problem-focused coping strategies, as compared with waitlist, but such improved coping did not associate with reductions in PTSS. Emotion-focused coping behaviors were not affected.
Three studies were identified among children and adolescents. Among UK children and adolescents with single-incident trauma, Meiser-Stedman et al. (2017; high quality) observed changes in rumination and safety-seeking behavior to associate with the effects of individual CT-PTSD on PTSS. When temporal order was established by only looking at changes from start of treatment to midway through it, only changes in safety-seeking remained a significant mediator of pre-post effects on PTSS. Among Indonesian schoolchildren, Tol et al. (2010; average quality) found a group-based psychosocial intervention to lead to more use of positive coping methods, but not to less use of negative ones. Positive coping methods did not, however, associate with treatment effects on PTSS. A similar intervention among Sri Lankan schoolchildren (Tol et al. 2012; average quality) did not lead to expected changes in coping method repertoire or satisfaction with coping strategies, either. The overall limited effectiveness of this intervention to reduce PTSS might explain these findings, but, contrariwise, failure to affect coping mechanisms may also explain some of the mixed results.
Attentional Processes
Three low-quality studies considered changes in attentional processes as mechanisms of change in PTSS reduction, with mixed findings. Improvements in attentional bias plasticity, though not in static attention bias, were found to partially explain the effectiveness of attention bias modification (ABM) over an attention control condition on PTSS among young US veterans (Kuckertz et al. 2014; low quality). In contrast, Badura-Brack et al. (2015; low quality) found that, among Israeli and US male combat veterans, computerized attention control training sessions, but not an ABM regimen, lead to reductions in attentional bias variability, which associated with reductions in PTSS. Among civilian female US sexual assault survivors, Bomyea, Stein, and Lang (2015; low quality) found an eight-session interference control training program to lead to improvements in working memory capacity (interpreted as evidence of proactive interference control ability) and re-experiencing symptoms. However, change in the proposed mechanism did not associate with effects on symptoms.
Traumatic Memories and Centrality of Traumatic Event
A single high-quality study was identified examining changes in traumatic memories as a mechanism of change. Meiser-Stedman et al. (2017; high quality) found pre-post changes in self-perceived quality of traumatic memories to be associated with CT-PTSD effects on PTSS among children and adolescents. However, when changes from pretreatment to midway through only were included, in order to establish temporal precedence of changes, no significant mediation was observed. One study examined perceived centrality of a traumatic event to one’s life as a potential mechanism. Among mainly female US adult civilians, Boals and Murrell (2016; low quality) found that four weekly sessions of acceptance and commitment therapy lead to greater reductions in PTSS compared to TAU, and that these reductions were associated with changes in perceptions of (traumatic) event centrality.
Mindfulness and Spirituality
Three average-quality studies examined increases in mindfulness as mechanisms of change in PTSS reduction, and one additional low-quality study considered spiritual well-being, all with positive findings. In the same sample as Oman and Bormann (2015), a mantram repetition program lead to increases in mindful attention among US combat veterans, as compared with TAU, and this increase partially explained treatments effects on PTSS (Bormann et al. 2014; average quality). A third analysis of the data found increases in spiritual well-being to also account for some of the program’s effects (Bormann et al. 2012; low quality).
Among older Swedish women with a cancer diagnosis, mindfulness-based stress reduction delivered in groups lead to increases in mindfulness from pretreatment to a three-month follow-up, compared with a waitlist, and increases in mindfulness associated with intervention effects on avoidance symptoms (Bränström et al. 2010; average quality). Intrusion and hyperarousal symptoms were not affected. In a pragmatic trial among US substance dependent civilians with traumatic experiences, a group-based program combining elements of mindfulness training and CBT lead to additional reductions in PTSS compared with a CBT program and TAU that were associated with increased dispositional mindfulness (Garland et al. 2016; average quality).
Emotion Regulation and Depressive Mood
Two high-quality, one average-quality and one low-quality study examined changes in emotion regulation or depressive symptoms as mechanisms of change in PTSS reduction. All studies had positive findings on these mechanisms, but methodological quality and measurement issues restrict the level of evidence they provide. Among a small sample of survivors of the Cambodian genocide now residing in the US and suffering from PTSD and orthostatic panic attacks, Hinton, Hofmann, Pollack, and Otto (2009; average quality) found the effects of a culturally adapted CBT treatment on PTSS to be associated with both improvements in emotion regulation capacity and decreases in orthostatic panic severity. They linked these changes to the involvement of decreased vagal tone in both processes. Sautter et al. (2016; low quality) found changes in emotion regulation problems and fears of intense emotions to explain intervention effects on PTSS among US combat veterans receiving structured approach therapy, as compared with family education.
Studying active duty US soldiers, Norr, Smolenski, and Reger (2018; high quality) found the effects of PE on PTSS at posttreatment to be mediated by reductions in share of suicidal ideation at midtreatment. While there was no evidence of reduction in PTSS similarly mediating effects on suicidal ideation, treatment effects on midtreatment PTSS did mediate posttreatment effects on overall depressive symptoms. The findings are limited by the use of a single-item dichotomous measure for the mechanism. Employing the same sample of female adolescent survivors of rape or CSA as McLean et al. (2015b), McLean, Su, Carpenter, and Foa (2017; high quality) found that reductions in depressive symptoms partially mediated the effects of time on PTSS during PE, but not during client-centered therapy. However, in both conditions, changes in PTSS also lead to subsequent changes in depression, suggesting a reciprocal relation, rather than a clear mechanism.
Discussion
Our aim was to identify mechanisms of change involved in psychological interventions for PTSS by systematically reviewing all available controlled studies. We also aimed to assess the strength and consistency of the evidence for their role in the alleviation of PTSS. The 34 controlled studies located examined a host of potential mechanisms of change in PTSS reduction that we roughly divided into six categories: posttraumatic cognitions and emotions; coping strategies and behaviors; attentional processes; traumatic memories and centrality of event; mindfulness and spirituality; and emotion regulation and depression.
Evidence for Different Mechanisms
Improvements in maladaptive trauma-related beliefs and appraisals appear to be a core mechanism of change involved in the effectiveness of many interventions for PTSS. We found the most evidence for this mechanism in relation to CBT interventions, but improvements in posttraumatic cognitions (PTCs) may be a rather general mechanism. Both treatments explicitly focusing on cognitive restructuring, such as CPT and TF-CBT, and those including fewer such elements, such as PE, appear to exert a significant part of their effects via this mechanism. It is possible that exposure leading to recollection of aspects of the trauma memory that contradict maladaptive PTCs may be enough to change them, even if they are not directly contested by cognitive strategies (Ehlers and Clark 2000; Foa et al. 2006). Our findings are consistent with previous results on how different trauma-focused CBT interventions are able to affect PTCs (Diehle et al. 2014; Hagenaars et al. 2010; Kumpula et al. 2017). We further found some suggestions that non-traumafocused interventions may partly work through change in posttraumatic cognitions and emotions by, e.g., reducing shame or sensitivity to anxiety. Overall findings on affecting shame or guilt were, however, limited to individual studies.
Cognitive-emotional models of PTSD (Ehlers and Clark 2000; Foa et al. 2006) suggest overly generalizing, catastrophizing or otherwise maladaptive posttraumatic appraisals to be crucial to the development and maintenance of and recovery from PTSS. This is supported by empirical evidence demonstrating that such PTCs feature heavily in the development and maintenance of PTSS both among adults (Hansen et al. 2014; Karl et al. 2009; LoSavio et al. 2017; Nixon and Bryant 2005) and children (Mitchell et al. 2017). Our findings here and those of previous reviews (Sripada et al. 2016; Zalta 2015) lend further credence to this view. Especially among female (sexual) assault survivors, evidence about the importance of cognitive changes in the treatment of PTSS is already robust. For children, we also found increasing evidence for cognitive change as a mechanism of change in individual trauma-focused therapies, while the limited findings for group-based psychosocial interventions were negative. Exactly what types of posttraumatic appraisals or beliefs might be most important to target in PTSS treatment remains less clear. We did find, however, some evidence of changing cognitions related to the self as incompetent or weak to be particularly relevant, as compared with appraisals of others or the world.
In contrast to PTCs, evidence on improvements in coping strategies as a mechanism of change in treating PTSS is so far limited. In the current review, the identified controlled studies on coping strategies were heterogeneous and offered mixed results. Theories such as emotional processing theory emphasize the importance of dysfunctional strategies of cognitive processing and behavioral coping that both directly produce PTSS and prevent corrective experiences and thereby improvements in them (Foa et al. 2006). Theories suggest that reduction in maladaptive coping strategies such as rumination, thought suppression and experiential avoidance might lead to the alleviation of PTSS by allowing for disconfirmation of maladaptive cognitions and restructuring of traumatic memories (Ehlers and Clark 2000; Foa et al. 2006). Research has indeed identified strong links between PTSS and maladaptive coping strategies (Ehlers et al. 2003; Meiser-Stedman et al. 2014; Seligowski et al. 2015; Szabo et al. 2017). However, we found little direct evidence so far to support the idea that reduction in the use of rumination, suppression and avoidance or increases in the use of more adaptive problem-focused strategies would account for the effects of successful interventions for PTSS.
Somewhat surprisingly, we found only one controlled study where changes in the nature or quality of traumatic memories were examined as a mechanism of PTSS reduction, that by Meiser-Stedman et al. (2017) among children with single-incident trauma. This is a striking finding, considering the emphasis influential accounts of PTSD, such as dual representation theory (Brewin et al. 1996; Brewin 2014) and the cognitive model of Ehlers and Clark (2000), place on the special nature of traumatic memories. One reason for this lack of research may be the difficulty of operationalizing and measuring the quality of traumatic memories, such as fragmentation versus coherence or level of integration and spatiotemporal contextualization. Outside controlled trials, some previous studies have found fragmentation and disorganization in trauma narratives to correlate with higher levels of PTSS (Halligan et al. 2003; Jones et al. 2007; Kenardy et al. 2007). Meanwhile, the few studies that exist among children have found conflicting results on the link between self-reported trauma memory quality and PTSS (McKinnon et al. 2017; Salmond et al. 2011). Some exposure-based treatments for PTSS explicitly posit that their beneficial effects take place, at least in part, via improved integration, organization or coherence of traumatic memories (Foa et al. 2007; Schauer et al. 2011). However, the few intervention studies available (Bedard-Gilligan et al. 2017; Desrochers et al. 2016) suggest that reduced fragmentation in trauma narratives may be more of a possible additional effect of treatment than a necessary mechanism responsible for symptom reduction (Cooper et al. 2017a; Foa et al. 2006). Besides fragmentation, our findings indicate that contextualization of trauma memories or integrating sensory-based memories into verbally accessible ones remain mostly unstudied empirically as mechanisms of change. Future research on the topic could contribute to both understanding whether the quality of traumatic memories should be a specific target of treatment and to theoretical debates about the special nature of traumatic memories and their relevance for PTSS (e.g., Brewin 2014, 2016; Rubin et al. 2016).
We also found little evidence on correcting attentional biases as a mechanism of change. This may reflect the overall limited effectiveness of attention bias modification programs for PTSS reduction, or, considering the small number of studies identified, simply lack of sustained research efforts in the area. Attentional biases are certainly observed in PTSD and the severity of PTSS and attentional biases appear to correlate (Bar-Haim et al. 2007; Pineles et al. 2009). However, empirical findings differ on whether such biases relate to emotional or threatening stimuli overall (Kimble et al. 2010; Vythilingam et al. 2007), trauma-specific stimuli (Fleurkens et al. 2011; Khanna et al. 2015), or a combination of both (Zinchenko et al. 2017). Though some intervention studies have reported success in diminishing PTSD-related attentional biases (El Khoury-Malhame et al. 2011; Khanna et al. 2015), there is so far scarce evidence of such improvements being a mechanism of change in PTSS reduction.
We found some preliminary evidence that reductions in PTSS achieved by mindfulness and mantram interventions are indeed associated with increases in dispositional mindfulness among adults. Such findings in support of the rationales of these non-traumafocused approaches merit further study. Head-to-head comparisons with trauma-focused methods would be especially valuable to tease apart general and specific mechanisms.
Two studies we included provided evidence for improvements in emotion regulation associating with PTSS reduction, both with war-related trauma among adults (Hinton et al. 2009; Sautter et al. 2016). Emotion regulation difficulties have been found to explain some of the links between trauma and PTSS in several studies (e.g., Tull et al. 2007; Ullman et al. 2014). In relation to treatment, Cloitre et al. (2002) found better emotion regulation skills to predict successful reduction of PTSS during exposure treatment for childhood abuse-related trauma, and Boden et al. (2013) reported reductions in a maladaptive emotion regulation strategy, expressive suppression, to associate with reduction in PTSS during group CBT treatment for combat veterans. In light of such additional findings and theoretical accounts suggesting emotion regulation to be important for recovery from PTSS (Foa et al. 2006), it, too, deserves to be included in future trials. Clear definitions and arguments are essential here, too, especially in separating mechanisms limited to emotion regulation from coping strategies more generally.
Finally, we found two studies suggesting reductions in depressive symptoms may drive PTSS reduction during PE, but also that earlier changes in PTSS may affect later depressive symptoms (McLean et al. 2017; Norr et al. 2018). Including measures of (posttraumatic) depression in future trials and examining the temporal order of recovery from different types of symptoms during interventions would improve understanding of the complex interplay between depressive and more directly stress-related symptoms.
Methodological Issues in Included Studies
The studies included in this review exhibited great heterogeneity in the interventions studied and study designs, as well as high variance in methodological quality. Though we initially planned mediational meta-analyses, we did not identify a sufficient number of adequately homogeneous studies on any mechanism to justify such analyses. The study of mechanisms of change is still nascent and would benefit from more uniform procedures and standards of reporting. Overall, we judged the quality of the included studies to be average. In line with Gallagher’s (2017) observation, we found the methodological quality of mechanism research to be improving over time. Indeed, all studies we classified as high quality had been published between 2015 and 2018. The most essential methodological problems identified relate to the modeling of change processes, especially inability to establish temporal sequence for changes and concerns of causal interpretation.
Nearly two thirds of studies included in this review were unable to show that changes in purported mechanisms preceded changes in PTSS. This substantial limitation weakens the level of evidence these studies provide for causal roles of the mechanisms studied in the interventions’ effects (Johansson and Høglend 2007; Pek and Hoyle 2016). They are not able to separate possible by-products of treatment, reciprocal effects, or indeed reductions in PTSS leading to changes in suggested mechanisms from the mechanism mediating the intervention’s effects on PTSS. Beyond this significant problem, there were few attempts to capture more complex forms of change in mechanisms or outcomes (Tryon 2005). Sudden gains are observed in PTSS treatment (Aderka et al. 2011; Krüger et al. 2014), and beneficial change in psychotherapy overall seems to cluster at the start and towards the end of treatment (Owen et al. 2015), suggesting uneven change trajectories.
More fundamentally, nearly all the studies included in this review relied on the traditional psychological approach to mediation established by Baron and Kenny (1986). Literature based on the potential outcome counterfactuals framework has pointed out that this approach, resting on linear regression or SEM, is in fact estimating the pure natural indirect effect (Muthén 2011) for a special case where problematic assumptions are made, typically without stating or justifying them (Bullock et al. 2010; Shpitser 2013). The indirect effect this approach provides can only be causally interpreted if we assume linear relations between treatment, mechanism and outcome, non-interaction between treatment and mechanism, and lack of confounders in the mechanism to outcome relation (Shpitser 2013). Causal mediation analyses explicitly based on the potential outcome counterfactuals framework have already seen adoption in, e.g., medicine and epidemiology, but there is, as of yet, limited evidence of its use in clinical psychological research.
Mechanisms of Change and Therapy Change Processes
This review found evidence that a variety of interventions may exploit similar mechanisms for their effects, particularly change in PTCs. That different interventions might have their effects via the same mechanism does not imply their equivalence (Zalta 2015). Quite different treatment components might draw on the same path to effectiveness, and their success in doing so might differ according to patient characteristics or other contextual factors. For these reasons, we deem it valuable to distinguish between mechanisms of change, representing changes in the client beyond the therapeutic context, and change processes during therapy, representing treatment components and changes in client response or behavior during therapy sessions. This distinction has sometimes been unclear in previous research. Still, all these elements are worth examining closely when we try to untangle how our interventions lead to their desired effects. Limiting ourselves here to mechanisms of change in the strict sense means this review cannot hope to provide a comprehensive account of processes of change in interventions for PTSS.
Mechanisms of change and in-session change processes of therapeutic interventions need not be studied in isolation. On the contrary, we need to integrate results from studying both to understand change in therapeutic interventions. Doss (2004) suggested understanding mechanisms of change was a step to be completed before moving on to study change processes during therapy sessions. For interventions for PTSS, there is much work to be done at this step. However, this does not preclude the study of crucial change processes during therapy, which indeed is also on-going both in terms of examining in-session client responses (e.g., de Kleine et al. 2017; Sripada and Rauch 2015) and particular treatment components (e.g., Deblinger et al. 2011; Sack et al. 2016). Mechanisms of change and treatment elements can also be studied in tandem, as Overbeek et al. (2017) did among children who had experienced interparental violence. Their approach of studying the effects of different degrees of exposure to specific and non-specific treatment elements as potentially mediated via different mechanisms can be recommended as highly informative about the relationships between therapy change processes and mechanisms of change beyond therapy.
Limitations
In addition to the exclusive focus on mechanisms of change strictly defined, some other limitations pertain to this review and its results. First, this review only included controlled studies. We therefore excluded some fine-grained analyses that have examined (mainly cognitive) change processes during therapy for PTSS in detail (e.g., Kleim et al. 2013; Kumpula et al. 2017). The choice to exclude uncontrolled studies does not suggest they cannot contribute to our understanding of change processes. Demonstrating how changes in particular mechanisms lead to changes in symptoms during treatment can be tremendously informative for mechanism research. However, uncontrolled analyses cannot, sensu stricto, provide evidence on the mechanisms of change responsible for an intervention’s effects on outcomes isolated from naturalistic change or a control condition’s effects. Therefore, we chose to exclude them here.
Second, we limited ourselves to studies published in peer-reviewed journals. It is possible we could have missed some individual relevant analyses of mechanisms of change because of this criterion, though we are not aware of any. More widely, publication bias is an important issue not just for effectiveness trials, but also research on mechanisms of change. Bias in findings on mechanisms may have been introduced by mechanisms of change only having been studied for a select minority of trials, often as afterthoughts, by most studies only examining a single favorite mechanism each, and by positive findings being more likely to be published. It is important that negative findings on proposed mechanisms of change continue to be published, too. Preregistration of hypotheses on mechanisms and the inclusion of multiple potential mechanisms in analyses are other important solutions, as suggested below.
Third, there are some challenges in interpreting the increasing evidence found for reduction in maladaptive PTCs as a mechanism of change in PTSS reduction by psychological interventions. To begin with, the concepts and processes presented here under the expansive heading of posttraumatic cognitions represent a wide variety of appraisals, beliefs, and judgments. More detailed analyses on the specific types of posttraumatic cognitions and emotions that should be targeted for change are called for. We may also wonder whether change in cognitions is best understood as a mechanism leading to reduction in “actual PTSS” or just one aspect of a cascade of changes in symptoms. Here, most outcome measures for PTSS were still based on DSM-IV criteria. However, with the DSM-5 (American Psychiatric Association 2013) inclusion of negative alterations in cognitions and emotions as diagnostic criteria for PTSD, the risk of the mechanism being muddled with the outcome may increase going forward (Kraemer et al. 2002).
Fourth, skew in populations of the included studies, as relates to demographics, geography and nature of trauma experienced may limit the generalizability of the results. The great majority of the studies were conducted in the U.S. Even there, studies examining mechanisms of change in PTSS interventions are rare among civilian men. Out of the 31 samples included in this review, only two had a majority of male civilians, while nine samples were exclusively or nearly exclusively women, and seven consisted of combat veteran men. Even though PTSD is more common among women, this disparity in research is notable. Considering the nature of trauma, sexual violence among women and military combat among men are more often studied, while there is less research on mechanisms involved in healing from other types of traumatic experiences. For example, we found just one smaller study (Hinton et al. 2009) on civilian adults traumatized by war.
Overall, the wide range of different types of traumatic events participants in the included studies had experienced, including both single-incident and chronic trauma, is a challenge for interpreting our findings. As evidence accumulates, it is crucial to attempt to disentangle whether PTSS resulting from different types and levels of trauma exposure are indeed susceptible to change via the same or dissimilar mechanisms. The same may be said of those with and without comorbid disorders. Here, inclusion and exclusion criteria varied widely, from studies limited to those with comorbid disorders (McLean et al. 2015a; Mueser et al. 2008) to several that explicitly excluded those with comorbid problems.
We also included studies on mechanisms of change among children and adolescents in this review. With just nine studies found among children and adolescents and most of them focusing on PTCs, the generalizability of our findings to children and adolescents is quite uncertain, especially for mechanisms of change other than PTCs. We did not identify studies with very young children (below the age of nine). Children of school age and older do exhibit fairly similar PTSS (Salmon and Bryant 2002) and arguments have been made that prevailing cognitive models of PTSD would be applicable among children as well (Meiser-Stedman 2002; Mitchell et al. 2017). Still, the on-going and rapid cognitive and emotional development in late childhood and adolescence may well mean that the mechanisms of change most important for PTSS improvement are somewhat different. Additional research among children and adolescents is certainly called for.
Finally, while we evaluated the quality of the included studies systematically with a pre-drafted assessment procedure, our checklist consisted of a novel combination of items. We view the use of a novel checklist as justified, as existing ones such as the Jadad scale (Jadad et al. 1996) do not include facets important to analyses of mechanisms of change. Still, at least the division of studies as providing low, average, or high quality evidence should be interpreted very cautiously.
Recommendations
Based on the findings of this review, we present recommendations for future research on mechanisms of change in Table 2. Some recommendations echo those presented by Lemmens et al. (2016) for research into psychotherapy for depression, but some are more specific to the question of PTSS. We have divided the recommendations into critical, important and helpful categories according to their importance for improving research standards, but this classification is only approximate. We expand on some recommendations below.
First and foremost, as already recommended by Kraemer et al. (2002), gathering evidence on potential mechanisms of change should become a routine part of the design of all trials on psychological interventions, including those for PTSS. Well-conducted clinical trials are expensive and time-consuming, so maximizing the benefit we get from each completed trial in terms of increasing our understanding of the mechanisms underlying successful treatment is crucial. Optimally, plans on the analysis of mechanisms would already be included and described in detail in study protocols during pre-registration in order to decrease publication bias. When they plan analyses of mechanisms of change beforehand, researchers can conduct power analyses on the indirect effect to ensure their studies have enough power to provide meaningful evidence about the mechanisms at work. This can be somewhat more complicated than power analysis for the total effect, but is possible via Monte Carlo methods even for complex mediational models (see, e.g., Muthén 2011; Thoemmes et al. 2010).
Further, it will usually make sense to study several potential mechanisms in analyses and preferably include them in the same models (Hayes and Rockwood 2016). This enables reporting on the role of not just one mechanism appropriate for the treatment in question, but on other putative mechanisms which make theoretical sense or for which previous evidence exists in the reduction of PTSS (Johansson and Høglend 2007; Kazdin 2007). In a multiple mediation model, it is possible to more appropriately quantify and meaningfully compare the magnitudes of effects via different mechanisms (Preacher and Hayes 2008).
For mediational analyses, it is crucial that researchers assess changes in mechanisms and outcomes several times, including at least once during the treatment process, in order to establish the temporal order of changes. To report the effect mediated through a mechanism of change, the indirect effect should be quantified and its significance assessed by the bias-corrected bootstrap confidence interval, the Monte Carlo confidence interval, the distribution of the product method or the percentile bootstrap confidence interval (Hayes and Scharkow 2013). The partially (by the scale of the outcome) standardized indirect effect is an unbiased and consistent measure for meaningfully quantifying its magnitude (Cheung 2009). Several studies in this review reported the proportion mediated, the proportion of the total effect due to an indirect effect via a mechanism, in percentages or shares (Alwin and Hauser 1975). This measure is awkward, as the “percentage mediated” may even exceed 100. Relatedly, claiming full or total mediation when, after the addition of an indirect path, the direct path is no longer statistically significant can be misleading, as this could result from a very small change in the magnitude of the direct effect (Hayes and Rockwood 2016). For example, Oman and Bormann (2015) claimed “full mediation”, even though their estimate for the magnitude of the indirect effect was smaller than for the remaining direct effect.
To improve the causal interpretation of their claims, researchers might wish to frame their analyses in the formal language of counterfactuals (Imai et al. 2015; Pearl 2001; Shpitser 2013). If researchers do not wish to adopt such an approach, justifications for the assumptions made in traditional mediation analysis, e.g., not considering interaction effects and lack of confounders in the mechanism to outcome relation, should be provided. Problems of mechanism-outcome confounding can be examined by sensitivity analysis for the indirect effect (Imai et al. 2015), and a number of design- and analysis-based solutions to overcome them exist (MacKinnon and Pirlott 2015; Valente et al. 2017).
Finally, we would argue that for studying mechanisms of change, the strongest research designs would be three-armed, with two groups receiving active treatments aiming to reduce PTSS (possibly via different mechanisms), and one group acting as a waitlist/minimal attention/TAU control group. With such a design, we can study both the indirect effects of the treatments as compared with the control group via different proposed mechanisms, and contrast the two active treatments with each other in terms of which mechanisms they actually employ. Dismantling designs where one group receives a full intervention and another the same intervention less a particular component are also highly valuable.
Conclusions
Our findings here reinforce the understanding that changes in trauma-related cognitions are a general mechanism of change in treating posttraumatic stress symptoms among both adults and children. Changes in such cognitions can be achieved through several types of interventions and lead to relief from symptoms. The paucity of empirical evidence for other mechanisms postulated by theoretical models and rationales for treatments is striking. In particular, this review highlighted that improvements in the quality, coherence, or integration of traumatic memories have not been empirically shown to be a mechanism of change involved in any psychological intervention aiming to reduce PTSS. Evidence on changes in attentional biases, coping behaviors, or emotion regulation as mechanisms of change is limited to individual studies. However, these findings do not necessarily suggest that these mechanisms are not important for treating PTSS. Instead, they reflect the scarcity of controlled studies on such mechanisms at present.
In terms of mechanisms specific to particular non-traumafocused approaches, a few studies suggest that improvements in PTSS achieved by mindfulness-based interventions may indeed be linked to increased mindfulness and spiritual well-being. There is, as of yet, little evidence for other more specific mechanisms of change.
The study of mechanisms of change should be part of all future trials on psychological interventions for PTSS and plans for such analyses included in preregistered protocols. The field would also benefit from more uniform and modern standards in study design and statistical analysis. We have attempted to contribute to such standards by providing some recommendations based on the findings of this review.
References
Aderka, I. M., Appelbaum-Namdar, E., Shafran, N., & Gilboa-Schechtman, E. (2011). Sudden gains in prolonged exposure for children and adolescents with posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 79(4), 441–446. https://doi.org/10.1037/a0024112.
Allan, N. P., Short, N. A., Albanese, B. J., Keough, M. E., & Schmidt, N. B. (2015). Direct and mediating effects of an anxiety sensitivity intervention on posttraumatic stress disorder symptoms in trauma-exposed individuals. Cognitive Behaviour Therapy, 44(6), 512–524. https://doi.org/10.1080/16506073.2015.1075227.
Alwin, D. F., & Hauser, R. M. (1975). The decomposition of effects in path analysis. American Sociological Review, 40(1), 37–47.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: APA.
Badura-Brack, A. S., Naim, R., Ryan, T. J., Levy, O., Abend, R., Khanna, M. M., … Bar-Haim, Y. (2015). Effect of attention training on attention bias variability and PTSD symptoms: Randomized controlled trials in Israeli and U.S. combat veterans. American Journal of Psychiatry, 172:12. https://doi.org/10.1176/appi.ajp.2015.14121578.
Bar-Haim, Y., Lamy, D., Pergamin, L., Bakermans-Kranenburg, M. J., & van Ijzendoorn, M. H. (2007). Threat-related attentional bias in anxious and nonanxious individuals: A meta-analytic study. Psychological Bulletin, 133(1), 1–24. https://doi.org/10.1037/0033-2909.133.1.1.
Baron, R. M., & Kenny, D. A. (1986). The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51, 1173–1182.
Bedard-Gilligan, M., Zoellner, L. A., & Feeny, N. C. (2017). Is trauma memory special? Trauma narrative fragmentation in PTSD: Effects of treatment and response. Clinical Psychological Science, 5, 212–225. https://doi.org/10.1177/2167702616676581.
Boals, A., & Murrell, A. R. (2016). I am > trauma: Experimentally reducing event centrality and PTSD symptoms in a clinical trial. Journal of Loss and Trauma, 21, 471–483. https://doi.org/10.1080/15325024.2015.1117930.
Boden, M. T., Westermann, S., McRae, K., Kuo, J., Alvarez, J., Kulkarni, M. R., … Bonn-Miller, M. O. (2013). Emotion regulation and posttraumatic stress disorder: A prospective investigation. Journal of Social and Clinical Psychology, 32, 296–314. https://doi.org/10.1521/jscp.2013.32.3.296.
Bomyea, J., Stein, M. B., & Lang, A. J. (2015). Interference control training for PTSD: A randomized controlled trial of a novel computer-based intervention. Journal of Anxiety Disorders, 34, 33–42. https://doi.org/10.1016/j.janxdis.2015.05.010.
Bormann, J. E., Liu, L., Thorp, S. R., & Lang, A. J. (2012). Spiritual wellbeing mediates PTSD change in veterans with military-related PTSD. International Journal of Behavioral Medicine, 19, 496–502. https://doi.org/10.1007/s12529-011-9186-1.
Bormann, J. E., Oman, D., Walter, K. H., & Johnson, B. D. (2014). Mindful attention increases and mediates psychological outcomes following mantram repetition practice in veterans with posttraumatic stress disorder. Medical Care, 12, S13–S18. https://doi.org/10.1097/MLR.0000000000000200.
Bränström, R., Kvillemo, P., Brandberg, Y., & Moskowitz, J. T. (2010). Self-report mindfulness as a mediator of psychological well-being in a stress reduction intervention for cancer patients — A randomized study. Annals of Behavioral Medicine, 39, 151–161. https://doi.org/10.1007/s12160-010-9168-6.
Brewin, C. R. (2014). Episodic memory, perceptual memory, and their interaction: Foundations for a theory of posttraumatic stress disorder. Psychological Bulletin, 140(1), 69–97. https://doi.org/10.1037/a0033722.
Brewin, C. R. (2016). Coherence, disorganization, and fragmentation in traumatic memory reconsidered: A response to Rubin et al. (2016). Journal of Abnormal Psychology, 125, 1011–1017. https://doi.org/10.1037/abn0000154.
Brewin, C. R., Dalgleish, T., & Joseph, S. (1996). A dual representation theory of post-traumatic stress disorder. Psychological Review, 103, 670–686. https://doi.org/10.1037/0033-295X.103.4.670.
Bullock, J. G., Green, D. P., & Ha, S. E. (2010). Yes, but what’s the mechanism? (Don’t expect an easy answer). Journal of Personality and Social Psychology, 98, 550–558. https://doi.org/10.1037/a0018933.
Cheung, M. W. (2009). Comparison of methods for constructing confidence intervals of standardized indirect effects. Behavior Research Methods, 41(2), 425–438. https://doi.org/10.3758/BRM.41.2.425.
Cloitre, M., Koenen, K. C., Cohen, L. R., & Han, H. (2002). Skills training in affective and interpersonal regulation followed by exposure: A phase-based treatment for PTSD related to childhood abuse. Journal of Consulting and Clinical Psychology, 70(5), 1067–1074. https://doi.org/10.1037/0022-006X.70.5.1067.
Cooper, A. A., Clifton, E. G., & Feeny, F. C. (2017a). An empirical review of potential mediators and mechanisms of prolonged exposure therapy. Clinical Psychology Review, 56, 106–121. https://doi.org/10.1016/j.cpr.2017.07.003.
Cooper, A. A., Zoellner, L. A., Roy-Byrne, P., Mavissakalian, M. R., & Feeny, N. C. (2017b). Do changes in trauma-related beliefs predict PTSD symptom improvement in prolonged exposure and sertraline? Journal of Consulting and Clinical Psychology, 85(9), 873–882. https://doi.org/10.1037/ccp0000220.
Cusack, K., Jonas, D. E., Forneris, C. A., Wines, C., Sonis, J., Middleton, F. C., … Gaynes, B. N. (2016). Psychological treatments for adults with posttraumatic stress disorder: A systematic review and meta-analysis. Clinical Psychology Review, 43, 128–141. https://doi.org/10.1016/j.cpr.2015.10.003.
de Kleine, R. A., Hendriks, L., Becker, E. S., Broekman, T. G., & van Minnen, A. (2017). Harm expectancy violation during exposure therapy for posttraumatic stress disorder. Journal of Anxiety Disorders, 49, 48–52. https://doi.org/10.1016/j.janxdis.2017.03.008.
Deblinger, E., Mannarino, A. P., Cohen, J. A., Runyon, M. K., & Steer, R. A. (2011). Trauma-focused cognitive behavioral therapy for children: Impact of the trauma narrative and treatment length. Depression and Anxiety, 28(1), 67–75. https://doi.org/10.1002/da.20744.
Desrochers, A. B., Beaulieu-Prévost, D., Desautels, J., Békés, V., Belleville, G., Guay, S., & Marchand, A. (2016). Gender and changes in trauma narrative following CBT for PTSD. Journal of Aggression, Maltreatment and Trauma, 25, 974–990. https://doi.org/10.1080/10926771.2016.1231147.
Diehle, J., Schmitt, K., Daams, J. G., Boer, F., & Lindauer, R. J. L. (2014). Effects of psychotherapy on trauma-related cognitions in posttraumatic stress disorder: A meta-analysis. Journal of Traumatic Stress, 27, 257–264. https://doi.org/10.1002/jts.21924.
Dorsey, S., McLaughlin, K., Kerns, S., Harrison, J., Lambert, H., Briggs., E., … Amaya-Jackson, L. (2017). Evidence base update for psychosocial treatments for children and adolescents exposed to traumatic events. Journal of Clinical Child and Adolescent Psychology, 46(3), 303–330. https://doi.org/10.1080/15374416.2016.1220309.
Doss, B. (2004). Changing the way we study change in psychotherapy. Clinical Psychology: Science and Practice, 11, 368–386. https://doi.org/10.1093/clipsy.bph094.
Ehlers, A., & Clark, D. M. (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38, 319–345.
Ehlers, A., Mayou, R. A., & Bryant, B. (2003). Cognitive predictors of posttraumatic stress disorder in children: Results of a prospective longitudinal study. Behaviour Research and Therapy, 41(1), 1–10.
Ehlers, A., Clark, D. M., Hackmann, A., McManus, F., & Fennell, M. (2005). Cognitive therapy for post-traumatic stress disorder: Development and evaluation. Behaviour Research and Therapy, 43(4), 413–431. https://doi.org/10.1016/j.brat.2004.03.006.
El Khoury-Malhame, M., Lanteaume, L., Beetz, E.M., Rogues, J., Reynaud, E., Samuelian, J.C., … Khalfa, S. (2011). Attentional bias in post-traumatic stress disorder diminishes after symptom amelioration. Behavior Research and Therapy, 49, 796–801. https://doi.org/10.1016/j.brat.2011.08.006.
Fleurkens, P., Rinck, M., & van Minnen, A. (2011). Specificity and generalization of attentional bias in sexual trauma victims suffering from posttraumatic stress disorder. Journal of Anxiety Disorders, 25, 783–787. https://doi.org/10.1016/j.janxdis.2011.03.014.
Foa, E. B., & Rauch, S. A. M. (2004). Cognitive changes during prolonged exposure versus prolonged exposure plus cognitive restructuring in female assault survivors with posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 72, 879–884. https://doi.org/10.1037/0022-006X.72.5.879.
Foa, E. B., Ehlers, A., Clark, D. M., Tolin, D. G., & Orsillo, S. M. (1999). The posttraumatic cognitions inventory (PTCI): Development and validation. Psychological Assessment, 11(3), 303–314.
Foa, E. B., Huppert, J. D., & Cahill, S. P. (2006). Emotional processing theory: An update. In B. O. Rothbaum (Ed.), Pathological anxiety: Emotional processing in etiology and treatment. New York: Guilford Press.
Foa, E. B., Hembree, E., & Rothbaum, B. O. (2007). Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences. New York: Oxford University Press.
Forst, N. D., Laska, J. M., & Wampold, B. E. (2014). The evidence for present-centered therapy as a treatment for posttraumatic stress disorder. Journal of Traumatic Stress, 27(1), 1–8. https://doi.org/10.1002/jts.21881.
Gallagher, M. W. (2017). Transdiagnostic mechanisms of change and cognitive-behavioral treatments for PTSD. Current Opinion in Psychology, 14, 90–95. https://doi.org/10.1016/j.copsyc.2016.12.002.
Gallagher, M. W., & Resick, P. A. (2012). Mechanisms of change in cognitive processing therapy and prolonged exposure therapy for PTSD: preliminary evidence for the differential effects of hopelessness and habituation. Cognitive Therapy Research, 36. https://doi.org/10.1007/s10608-011-9423-6.
Garland, E. L., Roberts-Lewis, A., Tronnier, C. D., Graves, R., & Kelley, K. (2016). Mindfulness-oriented recovery enhancement versus CBT for co-occurring substance dependence, traumatic stress, and psychiatric disorders: Proximal outcomes from a pragmatic randomized trial. Behaviour Research and Therapy, 77, 7–16. https://doi.org/10.1016/j.brat.2015.11.012.
Gillies, D., Maiocchi, L., Bhandari, A. P., Taylor, F., Gray, C., & O’Brien, L. (2016). Psychological therapies for children and adolescents exposed to trauma. Cochrane Database of Systematic Reviews, 10, CD012371. https://doi.org/10.1002/14651858.CD012371.
Ginzburg, K., Butler, L. D., Giese-Davis, J., Cavanaugh, C. E., Neri, E., Koopman, C., … & Spiegel, D. (2009). Shame, guilt, and posttraumatic stress disorder in adult survivors of childhood sexual abuse at risk for human immunodeficiency virus - outcomes of a randomized clinical trial of group psychotherapy treatment. Journal of Nervous and Mental Disease, 197, 536–542. https://doi.org/10.1097/NMD.0b013e3181ab2ebd.
Gu, J., Strauss, C., Bond, R., & Cavanagh, K. (2015). How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clinical Psychology Review, 37, 1–12. https://doi.org/10.1016/j.cpr.2015.01.006.
Hagenaars, M., van Minnen, A., & de Rooij, M. (2010). Cognitions in prolonged exposure therapy for posttraumatic stress disorder. International Journal of Clinical and Health Psychology, 10(3), 421–434.
Halligan, S. A., Michael, T., Clark, D. M., & Ehlers, A. (2003). Posttraumatic stress disorder following assault: The role of cognitive processing, trauma memory, and appraisals. Journal of Consulting and Clinical Psychology, 71, 419–431. https://doi.org/10.1037/0022-006X.71.3.419.
Hansen, M., Armour, C., Wittmann, L., Elklit, A., & Shevlin, M. (2014). Is there a common pathway to developing ASD and PTSD symptoms? Journal of Anxiety Disorders, 28, 865–872. https://doi.org/10.1016/j.janxdis.2014.09.019.
Hayes, A. F., & Rockwood, N. J. (2016). Regression-based statistical mediation and moderation analysis in clinical research: Observations, recommendations, and implementation. Behavior Research and Therapy, 98, 39–57. https://doi.org/10.1016/j.brat.2016.11.001.
Hayes, A. F., & Scharkow, M. (2013). The relative trustworthiness of inferential tests of the indirect effect in statistical mediation analysis: Does method really matter? Psychological Science, 24, 1918–1927. https://doi.org/10.1177/0956797613480187.
Hinton, D. E., Hofmann, S. G., Pollack, M. H., & Otto, M. W. (2009). Mechanisms of efficacy of CBT for Cambodian refugees with PTSD: Improvement in emotion regulation and orthostatic blood pressure response. CNS Neuroscience & Therapeutics, 15, 255–263. https://doi.org/10.1111/j.1755-5949.2009.00100.x.
Hyman, S. E. (2000). The millennium of mind, brain, and behaviour. Archives of General Psychiatry, 57(1), 88–89.
Imai, K., Keele, L., & Tingley, D. (2015). A general approach to causal mediation analysis. Psychological Methods, 15(4), 309–334. https://doi.org/10.1037/a0020761.
Jadad, A. R., Moore, R. A., Carroll, D., Jenkinson, C., Reynolds, D. J., Gavaghan, D. J., & McQuay, H. J. (1996). Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Controlled Clinical Trials, 17(1), 1–12. https://doi.org/10.1016/0197-2456(95)00134-4.
Jensen, T. K., Holt, T., Ormhaug, S. M., Fjermestad, K. W., & Wezel-Larsen, T. (2018). Change in post-traumatic cognitions mediates treatment effects for traumatized youth – A randomized controlled trial. Journal of Counseling Psychology, 65(2), 166–177. https://doi.org/10.1037/cou0000258.
Johansson, P., & Høglend, P. (2007). Identifying mechanisms of change in psychotherapy: Mediators of treatment outcome. Clinical Psychology & Psychotherapy, 14(1), 1–9. https://doi.org/10.1002/cpp.514.
Jones, C., Harvey, A. G., & Brewin, C. R. (2007). The organisation and content of trauma memories in survivors of road traffic accidents. Behavior Research and Therapy, 45(1), 151–162. https://doi.org/10.1016/j.brat.2006.02.004.
Kangaslampi, S., Punamäki, R.-L., Qouta, S., Diab, M., & Peltonen, K. (2016). Psychosocial group intervention among war-affected children: An analysis of changes in posttraumatic cognitions. Journal of Traumatic Stress, 29, 546–555. https://doi.org/10.1002/jts.22149.
Karl, A., Rabe, S., Zöllner, T., Maercker, A., & Stopa, L. (2009). Negative self-appraisals in treatment-seeking survivors of motor vehicle accidents. Journal of Anxiety Disorders, 23, 775–781. https://doi.org/10.1016/j.janxdis.2009.03.001.
Kazdin, A. E. (1999). Current (lack of) status of theory in child and adolescent psychotherapy research. Journal of Clinical Child Psychology, 28, 533–543. https://doi.org/10.1207/S15374424JCCP2804_13.
Kazdin, A. E. (2001). Progression of therapy research and clinical application of treatment require better understanding of the change process. Clinical Psychology: Science and Practice, 8(2), 143–151. https://doi.org/10.1093/clipsy.8.2.143.
Kazdin, A. E. (2007). Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology, 3, 1–27. https://doi.org/10.1146/annurev.clinpsy.3.022806.091432.
Kazdin, A. E. (2009). Understanding how and why psychotherapy leads to change. Psychotherapy Research, 19, 418–428. https://doi.org/10.1080/10503300802448899.
Kazdin, A. E., & Nock, M. K. (2003). Delineating mechanisms of change in child and adolescent therapy: Methodological issues and research recommendations. Journal of Child Psychology and Psychiatry, 44, 1116–1129. https://doi.org/10.1111/1469-7610.00195.
Kenardy, J., Smih, A., Spence, S. H., Lilley, P., Newcombe, P., Dob, R., & Robinson, S. (2007). Dissociation in children's trauma narratives: An exploratory investigation. Journal of Anxiety Disorders, 21, 456–466. https://doi.org/10.1016/j.janxdis.2006.05.007.
Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M., & Nelson, C. (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52(12), 1048–1060.
Khanna, M. M., Badura-Brack, A. S., McDermott, T M.., Shepherd, A., Heinrichs-Graham, E., Pine, D. S., … Wilson, T. W. (2015). Attention training normalises combat-related post-traumatic stress disorder effects on emotional Stroop performance using lexically matched word lists. Cognition and Emotion, 30, 1521–1528. https://doi.org/10.1080/02699931.2015.1076769.
Kimble, M. O., Fleming, K., Bandy, C., Kim, J., & Zambetti, A. (2010). Eye tracking and visual attention to threating stimuli in veterans of the Iraq war. Journal of Anxiety Disorders, 24, 293–299. https://doi.org/10.1016/j.janxdis.2009.12.006.
Kleim, B., Grey, N., Wild, J., Nussbek, F. W., Stott, R., Hackmann, A., … Ahlers, A. (2013). Cognitive change predicts symptom reduction with cognitive therapy for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 81, 383–393. https://doi.org/10.1037/a0031290.
Kraemer, H. C., Wilson, T., Fairburn, C. G., & Agras, W. S. (2002). Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry, 59, 877–883. https://doi.org/10.1001/archpsyc.59.10.877.
Krüger, A., Ehring, T., Priebe, K., Dyer, A. S., Steil, R., & Bohus, M. (2014). Sudden losses and sudden gains during a DBT-PTSD treatment for posttraumatic stress disorder following childhood sexual abuse. European Journal of Psychotraumatology, 5, 24470. https://doi.org/10.3402/ejpt.v5.24470.
Kuckertz, J. E., Amir, N., Boffa, J. W., Warren, C. K., Rindt, S. E., Norman, S., … McLay, R. (2014). The effectiveness of an attention bias modification program as an adjunctive treatment for post-traumatic stress disorder. Behaviour Research and Therapy, 63, 24–35. https://doi.org/10.1016/j.brat.2014.09.002.
Kumpula, M. J., Pentel, K. Z., Foa, E. B., LeBlanc, N. J., Bul, E., McSweeney, L. B., … Rauch, S. (2017). Temporal sequencing of change in posttraumatic cognitions and PTSD symptom reduction during prolonged exposure therapy. Behavior Therapy, 48(2), 156–165. https://doi.org/10.1016/j.beth.2016.02.008.
Lee, D. J., Schnitzlein, C. W., Wolf, J. P., Vythilingam, M., Rasmusson, A. M., & Hoge, C. W. (2016). Psychotherapy versus pharmacotherapy for posttraumatic stress disorder: Systemic review and meta-analyses to determine first-line treatments. Depression and Anxiety, 33, 792–806. https://doi.org/10.1002/da.22511.
Lemmens, L. H., Müller, V. N., Arntz, A., & Huibers, M. J. (2016). Mechanisms of change in psychotherapy for depression: An empirical update and evaluation of research aimed at identifying psychological mediators. Clinical Psychology Review, 50, 95–107. https://doi.org/10.1016/j.cpr.2016.09.004.
LoSavio, S. T., Dillon, K. H., & Resick, P. A. (2017). Cognitive factors in the development, maintenance, and treatment of post-traumatic stress disorder. Current Opinion in Psychology, 14, 18–22. https://doi.org/10.1016/j.copsyc.2016.09.006.
MacKinnon, D. P., & Pirlott, A. G. (2015). Statistical approaches for enhancing causal interpretation of the M-to-Y relation in mediation analysis. Personality and Social Psychology Review, 19(1), 30–43. https://doi.org/10.1177/1088868314542878.
MacKinnon, D. P., Lockwood, C. M., Hoffman, J. M., West, S. G., & Sheets, V. (2002). A comparison of methods to test mediation and other intervening variable effects. Psychological Methods, 7(1), 83–104. https://doi.org/10.1037/1082989X.7.1.83.
Markowitz, J. C., Petkova, A., Neria, Y., Van Meter, P. E., Zhao, Y., Hembree, E., … Marshall. R. D. (2015). Is exposure necessary? A randomized clinical trial of interpersonal psychotherapy for PTSD. American Journal of Psychiatry, 172(5), 1–11. https://doi.org/10.1176/appi.ajp.2014.14070908.
McKinnon, A., Brewer, N., Meiser-Stedman, R., & Nixon, R. D. V. (2017). Trauma memory characteristics and the development of acute stress disorder and post-traumatic stress disorder in youth. Journal of Behavior Therapy and Experimental Psychiatry, 54, 112–119. https://doi.org/10.1016/j.jbtep.2016.07.009.
McLean, C. P., Su, Y.-J., & Foa, E. B. (2015a). Mechanisms of symptom reduction in a combined treatment for comorbid posttraumatic stress disorder and alcohol dependence. Journal of Consulting and Clinical Psychology, 83, 655–661. https://doi.org/10.1037/ccp0000024.
McLean, C. P., Yeh, R., Rosenfield, D., & Foa, E. B. (2015b). Changes in negative cognitions mediate PTSD symptom reductions during client-centered therapy and prolonged exposure for adolescents. Behaviour Research and Therapy, 68, 64–69. https://doi.org/10.1016/j.brat.2015.03.008.
McLean, C. P., Su, Y.-J., Carpenter, J. K., & Foa, E. B. (2017). Changes in PTSD and depression during prolonged exposure and client-centered therapy for PTSD in adolescents. Journal of Clinical Child & Adolescent Psychology, 46, 500–510. https://doi.org/10.1080/15374416.2015.1012722.
Meiser-Stedman, R. (2002). Towards a cognitive-behavioral model of PTSD in children and adolescents. Clinical Child and Family Psychology Rview, 5(4), 217–232.
Meiser-Stedman, R., Shepperd, A., Glucksman, E., Dalgleish, T., Yule, W., & Smith, P. (2014). Thought control strategies and rumination in youth with acute stress disorder and posttraumatic stress disorder following single-event trauma. Journal of Child and Adolescent Psychopharmacology, 24(1), 47–51. https://doi.org/10.1089/cap.2013.0052.
Meiser-Stedman, R., Smith, P., McKinnon, A., Dixon, C., Trickey, D., Ehlers, A., … Dalgleish, T. (2017). Cognitive therapy as an early treatment for post-traumatic stress disorder in children and adolescents: A randomized controlled trial addressing preliminary efficacy and mechanisms of action. Journal of Child Psychology and Psychiatry 58, 623–633. https://doi.org/10.1111/jcpp.12673.
Mitchell, R., Brennan, K., Curran, D., Hanna, D., & Dyer, K. F. W. (2017). A meta-analysis of the association between appraisals of trauma and posttraumatic stress in children and adolescents. Journal of Traumatic Stress, 30(1), 88–93. https://doi.org/10.1002/jts.22157.
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & The PRISMA Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6, e1000097. https://doi.org/10.1371/journal.pmed1000097.
Mueser, K. T., Rosenberg, S. D., Xie, H., Jankowski, M. K., Bolton, E. E., Lu, W., … & Wolfe, R. (2008). A randomized controlled trial of cognitive-behavioral treatment of posttraumatic stress disorder in severe mental illness. Journal of Consulting and Clinical Psychology, 76(2), 259–271. https://doi.org/10.1037/0022-006X.76.2.259.
Muthén, B. (2011). Applications of causally defined direct and indirect effects in mediation analysis using SEM in Mplus. Available from: https://www.statmodel.com/download/causalmediation.pdf
Nixon, R. D., & Bryant, R. A. (2005). Are negative cognitions associated with severe acute trauma responses? Behavior Change, 22(1), 22–28. https://doi.org/10.1375/bech.22.1.22.66783.
Norr, A. M., Smolenski, D. J., & Reger, G. M. (2018). Effects of prolonged exposure and virtual reality exposure on suicidal ideation in active duty soldiers: An examination of potential mechanisms. Journal of Psychiatric Research, 103, 69–74. https://doi.org/10.1016/j.jpsychires.2018.05.009.
Oman, D., & Bormann, J. E. (2015). Mantram repetition fosters self-efficacy in veterans for managing PTSD: A randomized trial. Psychology of Religion and Spirituality, 7(1), 34–45. https://doi.org/10.1037/a0037994.
Overbeek, M. M., De Schipper, J. C., Willemen, A. M., Lamers-Winkelman, F., & Schuengel, C. (2017). Mediators and treatment factors in intervention for children exposed to interparental violence. Journal of Clinical Child and Adolescent Psychology, 46, 411–427. https://doi.org/10.1080/15374416.2015.1012720.
Owen, J., Adelson, J., Budge, S., Wampold, B., Kopta, M., Minami, T., & Miller, S. (2015). Trajectories of change in psychotherapy. Journal of Clinical Psychology, 71, 817–827. https://doi.org/10.1002/jclp.22191.
Pearl, J. (2001). Direct and indirect effects. In: Proceedings of the Seventeenth Conference on Uncertainty in Artificial Intelligence. San Francisco: Morgan Kaufmann.
Pek, J., & Hoyle, R. H. (2016). On the (in)validity of tests of simple mediation: Threats and solutions. Social and Personality Psychology Compass, 10(3), 150–163. https://doi.org/10.1111/spc3.12237.
Pfeiffer, E., Sachser, C., de Haan, A., Tutus, D., & Goldbeck, L. (2017). Dysfunctional posttraumatic cognitions as a mediator of symptom reduction in trauma-focused cognitive behavioral therapy with children and adolescents: Results of a randomized controlled trial. Behaviour Research and Therapy, 97, 178–182. https://doi.org/10.1016/j.brat.2017.08.001.
Pineles, S. L., Shipherd, J. C., Mostoufi, S. M., Abramovitz, S. M., & Yovel, I. (2009). Attentional biases in PTSD: More evidence for interference. Behavior Research and Therapy, 47, 1050–1057. https://doi.org/10.1016/j.brat.2009.08.001.
Preacher, K. J., & Hayes, A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879–891. https://doi.org/10.3758/BRM.40.3.879.
R Core Team. (2017). R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing.
Resick, P. A., Monson, C. M., & Chard, K. M. (2014). Cognitive processing therapy: Veteran/military version: Therapist's manual. Washington, DC: Department of Veterans Affairs.
Rosen, G. M., & Davison, G. C. (2003). Psychology should list empirically supported principles of change (ESPs) and not credential trademarked therapies or other treatment packages. Behavior Modification, 27(3), 300–312. https://doi.org/10.1177/0145445503253829.
Rubin, D. C., Berntsen, D., Ogle, C. M., Deffler, S. A., & Beckham, J. C. (2016). Scientific evidence versus outdated beliefs: A response to Brewin (2016). Journal of Abnormal Psychology, 125, 1018–1021.
Rytwinski, N. K., Scur, M. D., Feeny, N. C., & Youngstrom, E. A. (2013). The co-occurrence of major depressive disorder among individuals with posttraumatic stress disorder: A meta-analysis. Journal of Traumatic Stress, 26, 299–309. https://doi.org/10.1002/jts.21814.
Sack, M., Zehl, S., Otti, A., Lahmann, C., Henningsen, P., Kruse, J., & Stingl, M. (2016). A comparison of dual attention, eye movements, and exposure only during eye movement desensitization and reprocessing for posttraumatic stress disorder: Results from a randomized clinical trial. Psychotherapy and Psychosomatics, 85(6), 357–365. https://doi.org/10.1159/000447671.
Salmon, K., & Bryant, R. A. (2002). Posttraumatic stress disorder in children: The influence of developmental factors. Clinical Psychology Review, 22, 163–188. https://doi.org/10.1016/S0272-7358(01)00086-1.
Salmond, C., Meiser-Stedman, R., Glucksman, R., Thompson, P., Dalgleish, T., & Smith, P. (2011). The nature of trauma memories in acute stress disorder in children and adolescents. Journal of Child Psychology and Psychiatry, 52, 560–570. https://doi.org/10.1111/j.1469-7610.2010.02340.x.
Sautter, F. J., Glynn, S. M., Becker-Cretu, J. J., Senturk, D., Armelie, A. P., & Wielt, D. B. (2016). Structured approach therapy for combat-related PTSD in returning U.S. veterans: Complementary mediation by changes in emotion functioning. Journal of Traumatic Stress, 29(4), 384–387. https://doi.org/10.1002/jts.22120.
Schauer, E., Neuner, F., & Elbert, T. (2011). Narrative exposure therapy. A short-term treatment for traumatic stress disorders (2nd ed.). Göttingen: Hogrefe.
Scher, C. D., Suvak, M. K., & Resick, P. A. (2017). Trauma cognitions are related to symptoms up to 10 years after cognitive behavioral treatment for posttraumatic stress disorder. Psychological Trauma Theory Research Practice and Policy, 9, 750–757. https://doi.org/10.1037/tra0000258.
Seligowski, A. V., Lee, D. J., Bardeen, J. R., & Orcutt, H. K. (2015). Emotion regulation and posttraumatic stress symptoms: A meta-analysis. Cognitive Behaviour Therapy, 44(2), 87–102. https://doi.org/10.1080/16506073.2014.980753.
Shadish, W. (1996). Meta-analysis and the exploration of causal mediating processes: A primer of examples, methods, and issues. Psychological Methods, 1, 47–65. https://doi.org/10.1037/1082-989X.1.1.47.
Shapiro, D. A. (1995). Finding out how psychotherapies help people change. Psychotherapy Research, 5(1), 1–21.
Short, N. A., Boffa, J. W., Norr, A. M., Albanese, B. J., Allan, N. P., & Schmidt, N. B. (2017). Randomized clinical trial investigating the effects of an anxiety sensitivity intervention on posttraumatic stress symptoms: A replication and extension. Journal of Traumatic Stress, 30, 296–303. https://doi.org/10.1002/jts.22194.
Shpitser, I. (2013). Counterfactual graphical models for longitudinal mediation analysis with unobserved confounding. Cognitive Science, 37, 1011–1035. https://doi.org/10.1111/cogs.12058.
Sikkema, K. J., Ranby, K. W., Meade, C. S., Hansen, N. B., Wilson, P., & Kochman, A. (2013). Reductions in traumatic stress following a coping intervention were mediated by decreases in avoidant coping for people living with HIV/AIDS and childhood sexual abuse. Journal of Consulting and Clinical Psychology, 81(2), 274–283. https://doi.org/10.1037/a0030144.
Smith, P., Yule, W., Perrin, S., Tranah, T., Dalgleish, T., & Clark, D. M. (2007). Cognitive-behavioral therapy for PTSD in children and adolescents: A preliminary randomized controlled trial. JAMA Child and Adolescent Psychiatry, 46, 1051–1061. https://doi.org/10.1097/CHI.0b013e318067e288.
Sripada, R. K., & Rauch, S. A. M. (2015). Between-session and within-session habituation in prolonged exposure therapy for posttraumatic stress disorder: A hierarchical linear modeling approach. Journal of Anxiety Disorders, 30, 81–87. https://doi.org/10.1016/j.janxdis.2015.01.002.
Sripada, R. K., Rauch, S. A. M., & Liberzon, I. (2016). Psychological mechanisms of PTSD and its treatment. Current Psychiatry Reports, 18, 99. https://doi.org/10.1007/s11920-016-0735-9.
Szabo, Y. Z., Warnecke, A. J., Newton, T. L., & Valentine, J. C. (2017). Rumination and posttraumatic stress symptoms in trauma-exposed adults: A systematic review and meta-analysis. Anxiety, Stress, and Coping, 30, 396–414. https://doi.org/10.1080/10615806.2017.1313835.
Thoemmes, F., Mackinnon, D. P., & Reiser, M. R. (2010). Power analysis for complex mediational designs using Monte Carlo methods. Structural Equation Modeling, 17, 510–534. https://doi.org/10.1080/10705511.2010.489379.
Tol, W. A., Komproe, I. H., Jordans, M. J., Gross, A. L., Susanty, D., Macy, R. D., & de Jong, J. T. (2010). Mediators and moderators of a psychosocial intervention for children affected by political violence. Journal of Consulting and Clinical Psychology, 78, 818–828. https://doi.org/10.1037/a0021348.
Tol, W. A., Komproe, I. H., Jordans, M. J. D., Vallipuram, A., Sipsma, H., Sivayokan, S., … & de Jong, J. T. (2012). Outcomes and moderators of a preventive school-based mental health intervention for children affected by war in Sri Lanka: A cluster randomized trial. World Psychiatry, 11, 114–122.
Tryon, W. W. (2005). Possible mechanisms for why desensitization and exposure therapy work. Clinical Psychology Review, 25(1), 67–95. https://doi.org/10.1016/j.cpr.2004.08.005.
Tull, M. T., Barrett, H. M., McMillan, E. S., & Roemer, L. (2007). A preliminary investigation of the relationship between emotion regulation difficulties and posttraumatic stress symptoms. Behavior Therapy, 38, 303–313. https://doi.org/10.1016/j.beth.2006.10.001.
Ullman, S. E., Peter-Hagene, L. C., & Relyea, M. (2014). Coping, emotion regulation, and self-blame as mediators of sexual abuse and psychological symptoms in adult sexual assault. Journal of Child Sexual Abuse, 23(1), 74–93. https://doi.org/10.1080/10538712.2014.864747.
Valente, M. J., Pelham III, W. E., Smyth, H., & MacKinnon, D. P. (2017). Confounding in statistical mediation analysis: What it is and how to address it. Journal of Counseling Psychology, 64, 659–671. https://doi.org/10.1037/cou0000242.
Vythilingam, M., Blair, K.S., McCaffrey, D., Scaramozza, M., Jones, M., & Nakic, M. (2007). Biased emotional attention in post-traumatic stress disorder: A help as well as a hindrance? Psychological Medicine, 37, 1445–1455. https://doi.org/10.1017/S003329170700092X.
Watts, B. V., Schnurr, P. P., Mayo, L., Young-Xu, Y., Weeks, W. B., & Friedman, M. J. (2013). Meta-analysis of the efficacy of treatments for posttraumatic stress disorder. Journal of Clinical Psychiatry, 74, e541–e550. https://doi.org/10.4088/JCP.12r08225.
Ye, Z., Yu, N. X., Zhu, W., Chen, L., & Lin, D. (2018). A randomized controlled trial to enhance coping and posttraumatic growth and decrease posttraumatic stress disorder in HIV-infected men who have sex with men in Beijing, China. AIDS Care, 30(6), 793–801. https://doi.org/10.1080/09540121.2017.1417534.
Zalta, A. K. (2015). Psychological mechanisms of effective cognitive–behavioral treatments for PTSD. Current Psychiatry Reports, 17, 23. https://doi.org/10.1007/s11920-015-0560-6.
Zalta, A. K., Gillihan, S. J., Fisher, A. J., Mintz, J., McLean, C. P., Yehuda, R., & Foa, E. B. (2014). Change in negative cognitions associated with PTSD predicts symptom reduction in prolonged exposure. Journal of Consulting and Clinical Psychology, 82(1), 171–175. https://doi.org/10.1037/a0034735.
Zinchenko, A., Al-Amin, M. M., Alam, M. M., Mahmud, W., Kabir, N., Reza, H. M., & Burne, T. H. J. (2017). Content specificity of attentional bias to threat in post-traumatic stress disorder. Journal of Anxiety Disorders, 50, 33–39. https://doi.org/10.1016/j.janxdis.2017.05.006.
Zoellner, L. A., Feeny, N. C., Eftekhari, A., & Foa, E. B. (2011). Changes in negative beliefs following three brief programs for facilitating recovery after assault. Depression and Anxiety, 28, 532–540. https://doi.org/10.1002/da.20847.
Acknowledgements
We would like to thank Professor Raija-Leena Punamäki for helpful comments and suggestions during the preparation of this article.
Funding
Part of this research was funded by a personal grant from the Jenny and Antti Wihuri Foundation to the first author.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Studies
This research did not involve human or animal subjects.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Online Resource 1
(PDF 674 kb)
Online Resource 2
(PDF 541 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kangaslampi, S., Peltonen, K. Mechanisms of change in psychological interventions for posttraumatic stress symptoms: A systematic review with recommendations. Curr Psychol 41, 258–275 (2022). https://doi.org/10.1007/s12144-019-00478-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-019-00478-5