Abstract
Background
Real-world data are scarce about the effectiveness and safety of sofosbuvir/velpatasvir/voxilaprevir (SOF/VEL/VOX) for retreating East Asian patients with hepatitis C virus (HCV) infection who previously received NS5A direct-acting antivirals (DAAs). We conducted a multicenter study to assess the performance of SOF/VEL/VOX in patients who were not responsive to prior NS5A inhibitors in Taiwan.
Methods
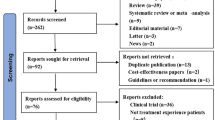
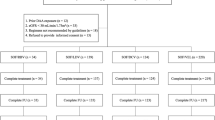
Between September 2021 and May 2022, 107 patients who failed NS5A inhibitor-containing DAAs with SOF/VEL/VOX salvage therapy for 12 weeks were included at 16 academic centers. The sustained virologic response at off-treatment week 12 (SVR12) was assessed in the evaluable (EP) and per-protocol (PP) populations. The safety profiles were also reported.
Results
All patients completed 12 weeks of treatment and achieved an end-of-treatment virologic response. The SVR12 rates were 97.2% (95% confidence interval (CI) 92.1–99.0%) and 100% (95% CI 96.4–100%) in EP and PP populations. Three (2.8%) patients were lost to off-treatment follow-up and did not meet SVR12 in the EP population. No baseline factors predicted SVR12. Two (1.9%) not-fatal serious adverse events (AE) occurred but were unrelated to SOF/VEL/VOX. Sixteen (15.0%) had grade 2 total bilirubin elevation, and three (2.8%) had grade 2 alanine transaminase (ALT) elevation. Thirteen (81.3%) of the 16 patients with grade 2 total bilirubin elevation had unconjugated hyperbilirubinemia. The estimated glomerular filtration rates (eGFR) were comparable between baseline and SVR12, regardless of baseline renal reserve.
Conclusions
SOF/VEL/VOX is highly efficacious and well-tolerated for East Asian HCV patients previously treated with NS5A inhibitor-containing DAAs.
Clinical trials registration
The study was not a drug trial. There was no need for clinical trial registration.




Similar content being viewed by others
Data availability
All data collection was approved by the Research Ethics Committee of each participating center.
Abbreviations
- HCV:
-
Hepatitis C virus
- DAA:
-
Direct-acting antiviral
- HCC:
-
Hepatocellular carcinoma
- SVR:
-
Sustained virologic response
- IFN:
-
Interferon
- RAS:
-
Resistance-associated substitution
- WHO:
-
World Health Organization
- SOF:
-
Sofosbuvir
- VEL:
-
Velpatasvir
- VOX:
-
Voxilaprevir
- FDC:
-
Fixed-dose combination
- GT:
-
Genotype
- RBV:
-
Ribavirin
- LLOQ:
-
Lower limit of quantification
- HBV:
-
Hepatitis B virus
- HIV:
-
Human immunodeficiency virus
- RNA:
-
Ribonucleic acid
- DNA:
-
Deoxyribonucleic acid
- DDI:
-
Drug-drug interaction
- DM:
-
Diabetes mellitus
- HTN:
-
Hypertension
- ULN:
-
Upper limit of normal
- AST:
-
Aspartate aminotransferase
- ALT:
-
Alanine aminotransferase
- eGFR:
-
Estimated glomerular filtration rate
- FIB-4:
-
Fibrosis index based on four parameters
- AE:
-
Adverse event
- IQR:
-
Interquartile range
- CI:
-
Confidence interval
- MAFLD:
-
Metabolic dysfunctional-associated fatty liver disease
- DILI:
-
Drug-induced liver injury
- NUC:
-
Nucleot(s)ide analogue
- OATP:
-
Organic anion transport protein
- DCV:
-
Daclatasvir
- ASV:
-
Asunaprevir
- PrOD:
-
Paritaprevir/ritonavir/ombitasvir plus dasabuvir
- EBR:
-
Elbasvir
- GZR:
-
Grazoprevir
- GLE:
-
Glecaprevir
- PIB:
-
Pibrentasvir
- LDV:
-
Ledipasvir
- CKD-EPI:
-
Chronic kidney disease epidemiology collaboration
- CTCAE:
-
Common terminology criteria for adverse events
References
Polaris Observatory HCV Collaborators. Global change in hepatitis C virus prevalence and cascade of care between 2015 and 2020: a modelling study. Lancet Gastroenterol Hepatol. 2022;7:396–415
Lauer GM, Walker BD. Hepatitis C virus infection. N Engl J Med. 2001;345:41–52
Liu CH, Kao JH. Nanomedicines in the treatment of hepatitis C virus infection in Asian patients: optimizing use of peginterferon alfa. Int J Nanomedicine. 2014;9:2051–2067
Feld JJ, Kowdley KV, Coakley E, Sigal S, Nelson DR, Crawford D, et al. Treatment of HCV with ABT-450/r-ombitasvir and dasabuvir with ribavirin. N Engl J Med. 2014;370:1594–1603
Zeuzem S, Ghalib R, Reddy KR, Pockros PJ, Ben Ari Z, Zhao Y, et al. Grazoprevir-elbasvir combination therapy for treatment-naive cirrhotic and noncirrhotic patients with chronic hepatitis C virus genotype 1, 4, or 6 infection: a randomized trial. Ann Intern Med. 2015;163:1–13
Afdhal N, Zeuzem S, Kwo P, Chojkier M, Gitlin N, Puoti M, et al; ION-1 Investigators. Ledipasvir and sofosbuvir for untreated HCV genotype 1 infection. N Engl J Med. 2014;370:1889–98.
Feld JJ, Jacobson IM, Hézode C, Asselah T, Ruane PJ, Gruener N, et al; ASTRAL-1 Investigators. Sofosbuvir and velpatasvir for HCV genotype 1, 2, 4, 5, and 6 infection. N Engl J Med. 2015;373:2599–607.
Zeuzem S, Foster GR, Wang S, Asatryan A, Gane E, Feld JJ, et al. Glecaprevir-pibrentasvir for 8 or 12 weeks in HCV genotype 1 or 3 infection. N Engl J Med. 2018;378:354–369
Ioannou GN, Beste LA, Chang MF, Green PK, Lowy E, Tsui JI, et al. Effectiveness of sofosbuvir, ledipasvir/sofosbuvir, or paritaprevir/ritonavir/ombitasvir and dasabuvir regimens for treatment of patients with hepatitis C in the Veterans Affairs National Health Care System. Gastroenterology. 2016;151:457–71.e5
Liu CH, Liu CJ, Su TH, Yang HC, Hong CM, Tseng TC, et al. Real-world effectiveness and safety of paritaprevir/ritonavir, ombitasvir, and dasabuvir with or without ribavirin for patients with chronic hepatitis C virus genotype 1b infection in Taiwan. J Gastroenterol Hepatol. 2018;33:710–717
Liu CH, Liu CJ, Su TH, Yang HC, Hong CM, Tseng TC, et al. Real-world effectiveness and safety of sofosbuvir and ledipasvir with or without ribavirin for patients with hepatitis C virus genotype 1 infection in Taiwan. PLoS ONE. 2018;13: e0209299
Lampertico P, Carrión JA, Curry M, Turnes J, Cornberg M, Negro F, et al. Real-world effectiveness and safety of glecaprevir/pibrentasvir for the treatment of patients with chronic HCV infection: a meta-analysis. J Hepatol. 2020;72:1112–1121
Liu CH, Liu CJ, Hung CC, Hsieh SM, Su TH, Sun HY, et al. Glecaprevir/pibrentasvir for patients with chronic hepatitis C virus infection: real-world effectiveness and safety in Taiwan. Liver Int. 2020;40:758–768
Mangia A, Milligan S, Khalili M, Fagiuoli S, Shafran SD, Carrat F, et al. Global real-world evidence of sofosbuvir/velpatasvir as simple, effective HCV treatment: analysis of 5552 patients from 12 cohorts. Liver Int. 2020;40:1841–1852
Liu CH, Chen PY, Chen JJ, Lo CC, Su WW, Tseng KC, et al. Sofosbuvir/velpatasvir for patients with chronic hepatitis C virus infection and compensated liver disease: real-world data in Taiwan. Hepatol Int. 2021;15:338–349
Benítez-Gutiérrez L, Barreiro P, Labarga P, de Mendoza C, Fernandez-Montero JV, Arias A, et al. Prevention and management of treatment failure to new oral hepatitis C drugs. Expert Opin Pharmacother. 2016;17:1215–1223
Heo YA, Deeks ED. Sofosbuvir/velpatasvir/voxilaprevir: a review in chronic hepatitis C. Drugs. 2018;78:577–587
AASLD-IDSA HCV Guidance Panel. Hepatitis C Guidance 2018 Update: AASLD-IDSA recommendations for testing, managing, and treating hepatitis C virus infection. Clin Infect Dis. 2018;67:1477–1492
European Association for the Study of the Liver. EASL recommendations on treatment of hepatitis C: final update of the series. J Hepatol. 2020;73:1170–1218
Omata M, Kanda T, Wei L, Yu ML, Chuang WL, Ibrahim A, et al. APASL consensus statements and recommendation on treatment of hepatitis C. Hepatol Int. 2016;10:702–726
Bourlière M, Gordon SC, Flamm SL, Cooper CL, Ramji A, Tong M, et al; POLARIS-1 and POLARIS-4 Investigators. Sofosbuvir, velpatasvir, and voxilaprevir for previously treated HCV infection. N Engl J Med. 2017;376:2134–46.
Bourlière M, Gordon SC, Schiff ER, Tran TT, Ravendhran N, Landis CS, et al. Deferred treatment with sofosbuvir-velpatasvir-voxilaprevir for patients with chronic hepatitis C virus who were previously treated with an NS5A inhibitor: an open-label substudy of POLARIS-1. Lancet Gastroenterol Hepatol. 2018;3:559–565
Llaneras J, Riveiro-Barciela M, Lens S, Diago M, Cachero A, García-Samaniego J, et al. Effectiveness and safety of sofosbuvir/velpatasvir/voxilaprevir in patients with chronic hepatitis C previously treated with DAAs. J Hepatol. 2019;71:666–672
Degasperi E, Spinetti A, Lombardi A, Landonio S, Rossi MC, Pasulo L, et al; NAVIGATORE-Lombardia and Veneto Study Groups. Real-life effectiveness and safety of sofosbuvir/velpatasvir/voxilaprevir in hepatitis C patients with previous DAA failure. J Hepatol. 2019;71:1106–15.
Belperio PS, Shahoumian TA, Loomis TP, Backus LI. Real-world effectiveness of sofosbuvir/velpatasvir/voxilaprevir in 573 direct-acting antiviral experienced hepatitis C patients. J Viral Hepat. 2019;26:980–990
Onofrio FQ, Cooper C, Borgia SM, Vachon ML, Ramji A, Lilly LB, et al. Salvage therapy with sofosbuvir/velpatasvir/voxilaprevir in DAA-experienced patients: results from a prospective Canadian registry. Clin Infect Dis. 2021;72:e799-805
Papaluca T, Roberts SK, Strasser SI, Stuart KA, Farrell G, MacQuillan G, et al. Efficacy and safety of sofosbuvir/velpatasvir/voxilaprevir for hepatitis C virus (HCV) NS5A-inhibitor experienced patients with difficult to cure characteristics. Clin Infect Dis. 2021;73:e3288–e3295
Da BL, Lourdusamy V, Kushner T, Dieterich D, Saberi B. Efficacy of sofosbuvir/velpatasvir/voxilaprevir in direct-acting antiviral experienced patients with hepatitis C virus. Eur J Gastroenterol Hepatol. 2021;33:859–861
Carson JM, Hajarizadeh B, Hanson J, O'Beirne J, Iser D, Read P, et al; REACH-C Study Group. Retreatment for hepatitis C virus direct acting antiviral therapy virological failure in primary and tertiary settings: the REACH-C cohort. J Viral Hepat. 2022;29:661–7.
Liu CH, Su TH, Liu CJ, Chen PJ, Chen DS, Kao JH. Sofosbuvir/velpatasvir/voxilaprevir plus ribavirin for chronic hepatitis C patients with direct acting antiviral failures: implications for viral elimination in Taiwan. J Formos Med Assoc. 2020;119:1871–1875
Wong YJ, Kumar R, Kumar R, Tan J, Liu CH, Hui VK, et al. Treatment outcomes of sofosbuvir/velpatasvir/voxilaprevir among NS5A inhibitor-experienced patients with hepatitis C: real-world data from a multicenter Asian registry. J Gastroenterol Hepatol. 2022;37:1642–1644
Liu CH, Liang CC, Liu CJ, Lin CL, Su TH, Yang HC, et al. Comparison of Abbott RealTime HCV Genotype II with Versant Line Probe Assay 2.0 for hepatitis C virus genotyping. J Clin Microbiol. 2015;53:1754–1757
Prati D, Taioli E, Zanella A, Della Torre E, Butelli S, Del Vecchio E, et al. Updated definitions of healthy ranges for serum alanine aminotransferase levels. Ann Intern Med. 2002;137:1–10
Liu CH, Lin JW, Liu CJ, Su TH, Wu JH, Tseng TC, et al. Long-term evolution of estimated glomerular filtration rate in patients with antiviral treatment for hepatitis C virus infection. Clin Gastroenterol Hepatol 2022. https://doi.org/10.1016/j.cgh.2022.01.050. Epub ahead of print. PMID: 35131346.
Sterling RK, Lissen E, Clumeck N, Sola R, Correa MC, Montaner J, et al; APRICOT Clinical Investigators. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology 2006;43:1317–25.
Sarrazin C, Cooper CL, Manns MP, Reddy KR, Kowdley KV, Roberts SK, et al. No impact of resistance-associated substitutions on the efficacy of sofosbuvir, velpatasvir, and voxilaprevir for 12 weeks in HCV DAA-experienced patients. J Hepatol. 2018;69:1221–1230
Liu CH, Yu ML, Peng CY, Hsieh TY, Huang YH, Su WW, et al. Comorbidities, concomitant medications and potential drug-drug interactions with interferon-free direct-acting antiviral agents in hepatitis C patients in Taiwan. Aliment Pharmacol Ther. 2018;48:1290–1300
Liu CH, Liu CJ, Su TH, Fang YJ, Yang HC, Chen PJ, et al. Hepatitis B virus reactivation in patients receiving interferon-free direct-acting antiviral agents for chronic hepatitis C virus infection. Open Forum Infect Dis. 2017;4:ofx028.
Xie J, Xu B, Wei L, Huang C, Liu W. Effectiveness and Safety of Sofosbuvir/velpatasvir/voxilaprevir as a hepatitis C virus infection salvage therapy in the real world: a systematic review and meta-analysis. Infect Dis Ther. 2022;11:1661–1682
Wilson E, Covert E, Hoffmann J, Comstock E, Emmanuel B, Tang L, et al. A pilot study of safety and efficacy of HCV retreatment with sofosbuvir/velpatasvir/voxilaprevir in patients with or without HIV (RESOLVE STUDY). J Hepatol. 2019;71:498–504
Pearlman B, Perrys M, Hinds A. Sofosbuvir/velpatasvir/voxilaprevir for previous treatment failures with glecaprevir/pibrentasvir in chronic hepatitis C infection. Am J Gastroenterol. 2019;114:1550–1552
Ruane P, Strasser SI, Gane EJ, Hyland RH, Shao J, Dvory-Sobol H, et al. Sofosbuvir/velpatasvir/voxilaprevir for patients with HCV who previously received a sofosbuvir/velpatasvir-containing regimen: results from a retreatment study. J Viral Hepat. 2019;26:770–773
Kalliokoski A, Niemi M. Impact of OATP transporters on pharmacokinetics. Br J Pharmacol. 2009;158:693–705
Ing Lorenzini K, Girardin F. Direct-acting antiviral interactions with opioids, alcohol or illicit drugs of abuse in HCV-infected patients. Liver Int. 2020;40:32–44
Liu CH, Lee MH, Lin JW, Liu CJ, Su TH, Tseng TC, et al. Evolution of eGFR in chronic HCV patients receiving sofosbuvir-based or sofosbuvir-free direct-acting antivirals. J Hepatol. 2020;72:839–846
Kanda T, Lau GKK, Wei L, Moriyama M, Yu ML, Chuang WL, et al. APASL clinical practice recommendation: how to treat HCV-infected patients with renal impairment? Hepatol Int. 2019;13:103–109
Patel S, Martin MT, Flamm SL. Sofosbuvir/velpatasvir/voxilaprevir for hepatitis C virus retreatment in decompensated cirrhosis. Liver Int. 2021;41:3024–3027
Acknowledgements
The authors thank Hui-Ju Lin and Pin-Chin Huang for clinical data management; the 7th Core Lab of the National Taiwan University Hospital, and the 1st Common Laboratory of the National Taiwan University Hospital, Yun-Lin Branch, for the instrumental and technical support.
Funding
None.
Author information
Authors and Affiliations
Contributions
Conception and design: CHL, JHK. Analysis and interpretation of data: CHL. Drafting of the article: CHL, JHK. Critical revision of the article for important intellectual content: CHL, CYP, CJL, CYC, CCL, KCT, PYS, WYK, MCT, HDT, HTC, FJL, CSH, KJH, YLS, SSY, JHW, HCL, YJF, PYC, JJH, CWT, WWS, CCC, PLL, JJC, CYC, TYH, CHC, YJH, JHK. Final approval of the article: CHL, CYP, CJL, CYC, CCL, KCT, PYS, WYK, MCT, HDT, HTC, FJL, CSH, KJH, YLS, SSY, JHW, HCL, YJF, PYC, JJH, CWT, WWS, CCC, PLL, JJC, CYC, TYH, CHC, YJH, JHK. Provision of study materials or patients: CHL, CYP, CJL, CYC, CCL, KCT, WWS, WYK, MCT, HDT, HTC, FJL, CSH, KJH, YLS, SSY, JHW, HCL, YJF, PYC, JJH, CWT, PYS, CCC, PLL, JJC, CYC, TYH, CHC, YJH, JHK. Statistical expertise: CHL. Administrative, technical, or logistic support: CHL, JHK. Collection and assembly of data: CHL.
Corresponding author
Ethics declarations
Conflicts of interest
Chen-Hua Liu: advisory board for Abbvie, Gilead Sciences, Merck Sharp & Dohme; speaker’s bureau for Abbott, Abbvie, Gilead Sciences, Merck Sharp & Dohme; research grant from Abbvie, Gilead Science, Merck Sharp & Dohme. Sheng-Shun Yang: advisory board for Abbvie, Roche, Ipsen; speaker’s bureau for Abbvie, Bristol-Myers Squibb, Gilead Sciences, Ipsen, Merck Sharp & Dohme. Jia- Horng Kao: advisory board for Abbott, Abbvie, Bristol-Myers Squibb, Gilead Sciences, GlaxoSmithKline, Merck Sharp & Dohme, Novartis, Roche; speaker’s bureau for Abbott, Abbvie, Bayer, Bristol-Myers Squibb, Gilead Sciences, GlaxoSmithKline, Merck Sharp & Dohme, Novartis, Roche. All other authors declare no competing interests.
Animal research
This study was not an animal research.
Ethical approval
The study was approved by the Research Ethics Committee of each participating center (ID: 202109016RIND) and was conducted in accordance with the principles of the Declaration of Helsinki in 1975.
Consent to participate
Each participant consented to this work and provided informed consent.
Consent to publish
All the authors consented the publish the work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, CH., Peng, CY., Liu, CJ. et al. Sofosbuvir/velpatasvir/voxilaprevir for patients with chronic hepatitis C virus infection previously treated with NS5A direct-acting antivirals: a real-world multicenter cohort in Taiwan. Hepatol Int 17, 291–302 (2023). https://doi.org/10.1007/s12072-022-10475-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-022-10475-9