Abstract
Objective
Multiple studies have shown worse outcomes in patients admitted for medical and surgical conditions on the weekend. However, past literature analyzing this “weekend effect” on subarachnoid hemorrhage (SAH) found no significant increase in mortality. This study utilizes more recent data to re-evaluate the association between weekend admission and mortality of patients hospitalized for SAH.
Methods
This retrospective cohort study queried the SAH patients in the Nationwide Inpatient Sample (NIS) database who were discharged from 2006 through 2014 during the weekend.
Results
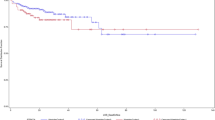
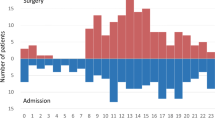
Of the 54,703 admissions for SAH identified during the study period, 14,821 (27.1%) occurred over the weekend. Patients admitted over the weekend had a mean age of 59.2 years and were most likely to be female (59.6%), to be white (62.9%), located in the south region of the USA (40.1%), and be admitted to a teaching hospital (74.4%). When compared directly to weekday admissions, patients admitted over the weekend had higher odds of in-hospital mortality (odds ratio 1.07; confidence interval 95%, 1.02–1.12). There was no significant difference shown in the rate patients get surgical clipping versus endovascular coiling (p = 0.28) or the amount of time between admission to procedure for clipping (p = 0.473) or coiling (p = 0.255) on the weekend versus a weekday.
Conclusion
Based on our findings, the likelihood of the in-hospital mortality was higher for patients admitted over the weekend. However, the characteristics of the study, primarily observational, prevent us arriving at an accurate conclusion about why this occurs; hence, we believe it is an important starting point to consider for future research.
Similar content being viewed by others
Abbreviations
- CT:
-
Computed tomography
- HCUP:
-
Healthcare Cost and Utilization Project
- ICD-9 CM:
-
International Classification of Diseases, Ninth Edition, Clinical Modification
- NIS:
-
Nationwide Inpatient Sample
- SAH:
-
Subarachnoid hemorrhage
References
Kreiter KT, Copeland D, Bernardini GL, Bates JE, Peery S, Claassen J, et al. Predictors of cognitive dysfunction after subarachnoid hemorrhage. Stroke J Cereb Circ. 2002;33:200.
Pas T, Marinus F, Lebret B, Oksbjerg N. Invited review. Arch Fuer Tierz. 2017;60:271–83.
Samra SK, Giordani B, Caveney AF, Clarke WR, Scott PA, Anderson S, et al. Recovery of cognitive function after surgery for aneurysmal subarachnoid hemorrhage. Stroke J Cereb Circ. 2007;38:1864–72.
van Gijn J, Kerr RS, Rinkel GJ. Subarachnoid haemorrhage. Lancet. 2007;369:306–18.
Juul R, Fredriksen TA, Ringkjøb R. Prognosis in subarachnoid hemorrhage of unknown etiology. J Neurosurg. 1986;64:359–62.
Kassell NF, Torner JC, Haley EC, Jane JA, Adams HP, Kongable GL. The international cooperative study on the timing of aneurysm surgery part I. J Neurosurg. 1990;73:18–36.
van Gijn J, Rinkel GJ. Subarachnoid haemorrhage: diagnosis, causes and management. Brain J Neurol. 2001;124:249–78.
Larsen CC, Astrup J. Rebleeding after aneurysmal subarachnoid hemorrhage: a literature review. World Neurosurg. 2013;79:307–12.
Brilstra EH, Rinkel GJ, Algra A, van Gijn J. Rebleeding, secondary ischemia, and timing of operation in patients with subarachnoid hemorrhage. Neurology. 2000;55:1656–60.
Roos YB, de Haan RJ, Beenen LF, Groen RJ, Albrecht KW, Vermeulen M. Complications and outcome in patients with aneurysmal subarachnoid haemorrhage: a prospective hospital based cohort study in the Netherlands. J Neurol Neurosurg Psychiatry. 2000;68:337–41.
Kassell NF, Torner JC, Jane JA, Haley EC, Adams HP. The international cooperative study on the timing of aneurysm surgery part II. J Neurosurg. 1990;73:37–47.
de Gans K, Nieuwkamp DJ, Rinkel GJE, Algra A. Timing of aneurysm surgery in subarachnoid hemorrhage: a systematic review of the literature. Neurosurgery. 2002;50:336–42.
Wong GKC, Boet R, Ng SCP, Chan M, Gin T, Zee B, et al. Ultra-early (within 24 hours) aneurysm treatment after subarachnoid hemorrhage. World Neurosurg. 2012;77:311–5.
Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345:663–8.
Deshmukh H, Hinkley M, Dulhanty L, Patel HC, Galea JP. Effect of weekend admission on in-hospital mortality and functional outcomes for patients with acute subarachnoid haemorrhage (SAH). Acta Neurochir (Wien). 2016;158:829–35.
Crowley RW, Yeoh HK, Stukenborg GJ, Ionescu AA, Kassell NF, Dumont AS. Influence of weekend versus weekday hospital admission on mortality following subarachnoid hemorrhage. J Neurosurg. 2009;111:60–6.
Zhang G, Zhang JH, Qin X. Effect of weekend admission on in-hospital mortality after subarachnoid hemorrhage in Chongqing China. Acta Neurochir. 2011;110:229–32.
HCUP N. Nationwide Inpatient Sample (NIS), Healthcare Cost and Utilization Project (HCUP). Rockv MD Agency Healthcare Research Quality; 2005.
Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27.
Higashida RT, Lahue BJ, Torbey MT, Hopkins LN, Leip E, Hanley DF. Treatment of unruptured intracranial aneurysms: a nationwide assessment of effectiveness. Am J Neuroradiol. 2007;28:146–51.
Bekelis K, Missios S, MacKenzie TA, Labropoulos N, Roberts DW. A predictive model of hospitalization cost after cerebral aneurysm clipping. J Neurointerv Surg. 2016;8:316–22.
Carr K, Rincon F, Maltenfort M, Birnbaum L, Dengler B, Rodriguez M, et al. Incidence and morbidity of craniocervical arterial dissections in atraumatic subarachnoid hemorrhage patients who underwent aneurysmal repair. J NeuroInterv Surg. 2015;7:728–33.
Long B, Koyfman A, Runyon MS. Subarachnoid hemorrhage: updates in diagnosis and management. Emerg Med Clin N Am. 2017;35:803–24.
Ruiz M, Bottle A, Aylin PP. The Global Comparators project: international comparison of 30-day in-hospital mortality by day of the week. BMJ Qual Saf. 2015;24:492–504.
Bottle A, Middleton S, Kalkman CJ, Livingston EH, Aylin P. Global Comparators Project: international comparison of hospital outcomes using administrative data. Health Serv Res. 2013;48:2081–100.
Galloway M, Hegarty A, McGill S, Arulkumaran N, Brett SJ, Harrison D. The effect of ICU out-of-hours admission on mortality: a systematic review and meta-analysis. Crit Care Med. 2018;46:290–9.
Gough MJ, Goodwin A, Shotton H, Butt A. Managing the flow? A review of the care received by patients who were diagnosed with an aneurysmal subarachnoid hemorrhage. Dave Terrey; 2013. Report No.: 1328–4045. http://www.ncepod.org.uk/2013report2/downloads/ManagingTheFlow_FullReport.pdf. Accessed Jan 2018.
Sander Connolly J E, Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, Higashida RT, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/american Stroke Association. Stroke J Cereb Circ. 2012;43:1711.
Gooderham PA, Steinberg GK. Reflections on the benefits and pitfalls of ultra-early aneurysm treatment after subarachnoid hemorrhage. World Neurosurg. 2012;77:261–2.
Park J, Woo H, Kang DH, Kim YS, Kim MY, Shin IH, et al. Formal protocol for emergency treatment of ruptured intracranial aneurysms to reduce in-hospital rebleeding and improve clinical outcomes. J Neurosurg. 2015;122:383–91.
Tarnow-Mordi WO, Hau C, Warden A, Shearer AJ. Hospital mortality in relation to staff workload: a 4-year study in an adult intensive-care unit. Lancet. 2000;356:185–9.
Petersen LA, Brennan TA, O’Neil AC, Cook E, Lee TH. Does housestaff discontinuity of care increase the risk for preventable adverse events? Ann Intern Med. 1994;121:866–72.
Thorpe KE. House staff supervision and working hours-reply. JAMA. 1990;264:2739.
Cram P, Hillis SL, Barnett M, Rosenthal GE. Effects of weekend admission and hospital teaching status on in-hospital mortality. Am J Med. 2004;117:151–7.
Saposnik G, Baibergenova A, Bayer N, Hachinski V. Weekends: a dangerous time for having a stroke? Stroke. 2007;38:1211–5.
Albright KC, Raman R, Ernstrom K, Hallevi H, Martin-Schild S, Meyer BC, et al. Can comprehensive stroke centers erase the ‘weekend effect’? Cerebrovasc Dis. 2009;27:107–13.
McKinney JS, Deng Y, Kasner SE, Kostis JB. Comprehensive stroke centers overcome the weekend versus weekday gap in stroke treatment and mortality. Stroke J Cereb Circ. 2011;42:2403–9.
Meretoja A, Roine RO, Kaste M, Linna M, Roine S, Juntunen M, et al. Effectiveness of primary and comprehensive stroke centers: PERFECT stroke: a nationwide observational study from Finland. Stroke. 2010;41:1102–7.
Mark TL, Dilonardo JD, Chalk M, Coffey RM. Trends in inpatient detoxification services, 1992–1997. J Subst Abuse Treat. 2002;23:253–60.
Livingston EH, Miller JAG, Coan B, Rege RV. Costs and utilization of intraoperative cholangiography. J Gastrointest Surg. 2007;11:1162–7.
Livingston EH, Elliott AC, Hynan LS, Engel E. When policy meets statistics: the very real effect that questionable statistical analysis has on limiting health care access for bariatric surgery. Arch Surg. 2007;142:979–87.
Berthelsen CL. Evaluation of coding data quality of the HCUP National Inpatient Sample. Top Health Inf Manag. 2000;21:10–23.
Funding
None.
Author information
Authors and Affiliations
Contributions
WCJ, NM-G, and DG contributed to the literature review and writing of the paper. Statistical analysis and writing the paper were carried out by JL. AM, who is an epidemiologist, edited the final draft and helped in the method rewriting. AS was the principal investigator, who designed the project and edited the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Rights and permissions
About this article
Cite this article
Johnson, W.C., Morton-Gonzaba, N.A., Lacci, J.V. et al. Re-evaluating the Weekend Effect on SAH: A Nationwide Analysis of the Association Between Mortality and Weekend Admission. Neurocrit Care 30, 293–300 (2019). https://doi.org/10.1007/s12028-018-0609-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-018-0609-6