Abstract
Background
Prolonged systemic antibiotic prophylaxis for central nervous system (CNS) devices may be associated with increased risk of antimicrobial resistance. The primary objective of this study was to determine the impact of prolonged CNS device antibiotic prophylaxis on the growth of resistant microorganisms and Clostridium difficile.
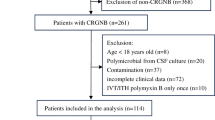
Methods
This retrospective, observational, cohort study included patients admitted to intensive care units with traumatic brain injury or other neurocritical illness. Patients who received a CNS device and antibiotic prophylaxis for at least 72 h were compared to patients with similar neurologic injuries who did not receive a CNS device.
Results
Study (n = 116) and control (n = 557) patients had mean APACHE II scores of 17.7 ± 9.2 and 15.1 ± 10.6 (p = 0.004) with 53.4 and 24.6 % receiving craniotomies (p < 0.001), respectively. Mean CNS device duration was 9.9 days, and 73 % of patients received cefuroxime for prophylaxis. The study cohort had a higher absolute incidence of resistant organisms compared with the control cohort (15.5 vs 4.1 %; odds ratio 1.93, 95 % CI 0.93–4.03, p = 0.078), though the study was underpowered to show statistical significance in multivariate analysis. C. difficile incidence was similar between groups (2.6 vs 2.0 %; odds ratio 1.45, 95 % CI 0.35–6.12, p = 0.61).
Conclusion
We found a higher incidence of resistant organisms in patients receiving prolonged antibiotic prophylaxis with a CNS device, but similar incidence of C. difficile compared to controls. Lack of data supporting prolonged antibiotic prophylaxis for CNS devices and the risk of nosocomial infections with resistant organisms encourage limiting prophylactic antibiotics to a short periprocedural course.


Similar content being viewed by others
References
Helmy A, Vizcaychipi M, Gupta AK. Traumatic brain injury: intensive care management. Br J Anaesth. 2007;99(1):32–42.
Mayhall CG, Archer NH, Lamb VA, et al. Ventriculostomy-related infections. A prospective epidemiologic study. N Engl J Med. 1984;310(9):553–9.
Holloway KL, Barnes T, Choi S, et al. Ventriculostomy infections: the effect of monitoring duration and catheter exchange in 584 patients. J Neurosurg. 1996;85:419–24.
Kim JH, Desai NS, Ricci J, et al. Factors contributing to ventriculostomy infection. World Neurosurg. 2012;77(1):135–40.
Stenehjem E, Armstrong WS. Central nervous system device infections. Infect Dis Clin North Am. 2012;26(1):89–110.
Ramanan M, Lipman J, Shorr A, Shankar A. A meta-analysis of ventriculostomy-associated cerebrospinal fluid infections. BMC Infect Dis. 2015;8(15):3.
Lozier AP, Sciacca RR, Romagnoli MF, Connolly ES. Ventriculostomy-related infections: a critical review of the literature. Neurosurgery. 2002;51(1):170–81.
Camacho EF, Boszczowski I, Basso M, et al. Infection rate and risk factors associated with infections related to external ventricular drain. Infection. 2011;39(1):47–51.
Citerio G, Signorini L, Bronco A, et al. External ventricular and lumbar drain device infections in ICU patients: a prospective multicenter Italian study. Crit Care Med. 2015;43(8):1630–7.
Bratzler DW, Dellinger EP, Olsen KM, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health-Syst Pharm. 2013;70:195–283.
Brain Trauma Foundation, American Association of Neurological Surgeons, Congress of Neurological Surgeons, et al. Guidelines for the management of severe traumatic brain injury. IV. Infection prophylaxis. J Neurotrauma 2007;24(suppl 1):S26–31.
Rebuck JA, Murry KR, Rhoney DH, Michael DB, Coplin WM. Infection related to intracranial pressure monitors in adults: analysis of risk factors and antibiotic prophylaxis. J Neurol Neurosurg Psychiatry. 2000;69:381–4.
Alleyne CH, Hassan M, Zabramski JM. The efficacy and cost of prophylactic and periprocedural antibiotics in patients with external ventricular drains. Neurosurgery. 2000;47:1124–9.
Poon WS, Ng S, Wai S. CSF antibiotic prophylaxis for neurosurgical patients with ventriculostomy: a randomised study. Acta Neurochir Suppl. 1998;71:146–8.
Dellit TH, Chan JD, Fulton C, et al. Reduction in Clostridium difficile infections among neurosurgical patients associated with discontinuation of antimicrobial prophylaxis for the duration of external ventricular drain placement. Infect Control Hosp Epidemiol. 2014;25(5):589–90.
Jacobs DG, Westerband A. Antibiotic prophylaxis for intracranial pressure monitors. J Natl Med Assoc. 1998;90:417–23.
Flibotte JJ, Lee KE, Koroshetz WJ, et al. Continuous antibiotic prophylaxis and cerebral spinal fluid infection in patients with intracranial pressure monitors. Neurocrit Care. 2004;1:61–8.
May AK, Fleming SB, Carpenter RO, et al. Influence of broad-spectrum antibiotic prophylaxis on intracranial pressure monitor infections and subsequent infectious complications in head injured patients. Surg Infect. 2006;7:409–17.
McCarthy PJ, Patil S, Conrad SA, Scott LK. International and specialty trends in the use of prophylactic antibiotics to prevent infectious complications after insertion of external ventricular drainage devices. Neurocrit Care. 2010;12(2):220–4.
Prabhu VC, Kaufman HH, Voelker JL, Aronoff SC, Niewiadomska-Bugaj M, Mascara S, Hobbs GR. Prophylactic antibiotics with intracranial pressure monitors and external ventricular drains: a review of the evidence. Surg Neurol. 1999;52(3):226–37.
Acknowledgments
The authors would like to thank Ramon Castillo III for his role in data extraction.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chauv, S., Fontaine, G.V., Hoang, Q.P. et al. Risk of Resistant Organisms and Clostridium difficile with Prolonged Systemic Antibiotic Prophylaxis for Central Nervous System Devices. Neurocrit Care 25, 128–132 (2016). https://doi.org/10.1007/s12028-016-0254-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-016-0254-x