Abstract
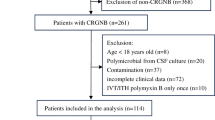
The objective of this study was to determine risk factors of pejorative evolution course in patients suffering from postoperative cranial infection. The data of patients who developed an intracranial infection after craniocerebral surgery in the neurosurgical intensive care unit of the First Affiliated Hospital of Nanjing Medical University in Nanjing, Jiangsu, China, from February 2018 to August 2019 were retrospectively analyzed. Logistic regression was used to analyze the factors influencing the prognosis of intracranial infection treatment. Sixty-four patients developed an infection after craniocerebral surgery, and 48 of them with negative CSF cultures received experimental anti-infectives. In 16 patients, cerebrospinal fluid culture showed pandrug-resistant pathogens, including 11 Acinetobacter baumannii (11), Klebsiella pneumoniae (3), Escherichia coli (1), and Candida glabrata (1). Nine patients received intraventricular or intrathecal injections of polymyxin B. The mean duration of infection treatment was 22.2 ± 9.9 days, and the clinical cure rate was 85.9% (55/64). Logistic multivariate regression analysis showed that inadequate CSF drainage (OR, 6.839; 95% CI, 1.130–41.383; P = 0.036) and infection with drug-resistant bacteria (OR, 24.241; 95% CI, 2.032–289.150; P = 0.012) were independent risk factors for postoperative intracranial infection. Intracranial infection with positive CSF culture and inadequate CSF drainage are factors contributing to the poor prognosis of intracranial infection. Moreover, early anti-infection treatment and adequate CSF drainage may improve patient outcomes. In particular, intraventricular or intrathecal injection of polymyxin B may be a safe and effective treatment strategy for MDR/XDR gram-negative bacilli infection.

Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author, Dr. Jing Ji, upon request.
References
Ortiz OH, García HI, Ramírez FM, Flórez JS, Valencia BA, Mantilla SE, Ochoa MJ, Ochoa JE, Jaimes F (2018) Development of a prediction rule for diagnosing postoperative meningitis: a cross-sectional study. J Neurosurg 128(1):262–271. https://doi.org/10.3171/2016.10.JNS16379
De Bonis P, Lofrese G, Scoppettuolo G, Spanu T, Cultrera R, Labonia M, Cavallo MA, Mangiola A, Anile C, Pompucci A (2016) Intraventricular versus intravenous colistin for the treatment of extensively drug resistant Acinetobacter baumannii meningitis. Eur J Neurol 23(1):68–75. https://doi.org/10.1111/ene.12789
Shahan B, Choi EY, Nieves G (2021) Cerebrospinal fluid analysis. Am Fam Physician 103(7):422–428 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/33788511
Society, C. N., & (2017), CNCMCG Consensus of experts in the diagnosis and treatment of infection in Chinese neurosurgical critical patients (2017). Natl Med J China(21).
Chen L, Li X, Li D, Dong X, Chen H (2022) Efficacy and safety of intraventricular polymyxin B plus continuous ventricular drainage for the treatment of intracranial infection caused by drug-resistant Acinetobacter baumannii. Ann Palliat Med 11(2):490–497. https://doi.org/10.21037/apm-21-3149
Tunkel, A. R., Hasbun, R., Bhimraj, A., Byers, K., Kaplan, S. L., Scheld, W. M., . . . Zunt, J. R. (2017). 2017 Infectious Diseases Society of America's Clinical Practice Guidelines for Healthcare-Associated Ventriculitis and Meningitis. Clin Infect Dis, 64(6), e34-e65. https://doi.org/10.1093/cid/ciw861
Nau R, Seele J, Djukic M, Eiffert H (2018) Pharmacokinetics and pharmacodynamics of antibiotics in central nervous system infections. Curr Opin Infect Dis 31(1):57–68. https://doi.org/10.1097/QCO.0000000000000418
Kural C, Kirmizigoz S, Ezgu MC, Bedir O, Kutlay M, Izci Y (2019) Intracranial infections: lessons learned from 52 surgically treated cases. Neurosurg Focus 47(2):E10. https://doi.org/10.3171/2019.5.FOCUS19238
Zhang, Y., Cui, P., Zhang, H. C., Wu, H. L., Ye, M. Z., Zhu, Y. M., . . . Zhang, W. H. (2020). Clinical application and evaluation of metagenomic next-generation sequencing in suspected adult central nervous system infection. J Transl Med, 18(1), 199. https://doi.org/10.1186/s12967-020-02360-6
Dabrowski P, Jurkiewicz J, Czernicki Z, Koszewski W, Jasielski P (2017) Polymerase chain reaction based detection of bacterial 16S rRNA gene in the cerebrospinal fluid in the diagnosis of bacterial central nervous system infection in the course of external cerebrospinal fluid drainage. Comparison with standard diagnostics currently used in clinical practice. Neurol Neurochir Pol 51(5):388–394. https://doi.org/10.1016/j.pjnns.2017.06.013
Perdigão Neto LV, Medeiros M, Ferreira SC, Nishiya AS, de Assis DB, Boszczowski Í, Costa SF, Levin AS (2021) Polymerase chain reaction targeting 16S ribosomal RNA for the diagnosis of bacterial meningitis after neurosurgery. Clinics (Sao Paulo) 76:e2284. https://doi.org/10.6061/clinics/2021/e2284
Ruan L, Wu D, Li X, Huang Q, Lin L, Lin J, Chen L, Xu P, Jin J, Yang N, Li X (2017) Analysis of microbial community composition and diversity in postoperative intracranial infection using high-throughput sequencing. Mol Med Rep 16(4):3938–3946. https://doi.org/10.3892/mmr.2017.7082
Tattevin P, Solomon T, Brouwer MC (2019) Understanding central nervous system efficacy of antimicrobials. Intensive Care Med 45(1):93–96. https://doi.org/10.1007/s00134-018-5270-1
Li J, Zhao QH, Huang KC, Li ZQ, Zhang LY, Qin DY, Pan F, Huang WX (2017) Linezolid vs. vancomycin in treatment of methicillin-resistant staphylococcus aureus infections: a meta-analysis. Eur Rev Med Pharmacol Sci 21(17):3974–3979 https://www.ncbi.nlm.nih.gov/pubmed/28975963
Hussein K, Bitterman R, Shofty B, Paul M, Neuberger A (2017) Management of post-neurosurgical meningitis: narrative review. Clin Microbiol Infect 23(9):621–628. https://doi.org/10.1016/j.cmi.2017.05.013
Dang S, J.-X. M., Zhou G, Wang F, Guo (2015). Etiological surveillance of intracranial infections in patients undergoing craniotomy and analysis of risk factors. Chin J Nosocomiology.
Kourbeti IS, Vakis AF, Ziakas P, Karabetsos D, Potolidis E, Christou S, Samonis G (2015) Infections in patients undergoing craniotomy: risk factors associated with post-craniotomy meningitis. J Neurosurg 122(5):1113–1119. https://doi.org/10.3171/2014.8.JNS132557
Chen H, Guo X, Xie D, Dong X, Niu J, Chen G (2020) A clinical study on the use of intraventricular polymyxin B supplemented by continuous external ventricular drainage in the treatment of drug-resistant gram-negative bacilli intracranial infection. Infect Drug Resist 13:2963–2970. https://doi.org/10.2147/IDR.S261510
Abulhasan YB, Al-Jehani H, Valiquette MA, McManus A, Dolan-Cake M, Ayoub O, Angle M, Teitelbaum J (2013) Lumbar drainage for the treatment of severe bacterial meningitis. Neurocrit Care 19(2):199–205. https://doi.org/10.1007/s12028-013-9853-y
Remes F, Tomas R, Jindrak V, Vanis V, Setlik M (2013) Intraventricular and lumbar intrathecal administration of antibiotics in postneurosurgical patients with meningitis and/or ventriculitis in a serious clinical state. J Neurosurg 119(6):1596–1602. https://doi.org/10.3171/2013.6.JNS122126
Wang K, Liu Z, Chen X, Lou M, Yin J (2013) Clinical characteristics and outcomes of patients with cerebral herniation during continuous lumbar drainage. Turk Neurosurg 23(5):653–657. https://doi.org/10.5137/1019-5149.JTN.7954-13.0
Ramanan M, Lipman J, Shorr A, Shankar A (2015) A meta-analysis of ventriculostomy-associated cerebrospinal fluid infections. BMC Infect Dis 15:3. https://doi.org/10.1186/s12879-014-0712-z
Governale LS, Fein N, Logsdon J, Black PM (2008) Techniques and complications of external lumbar drainage for normal pressure hydrocephalus. Neurosurgery 63(4 Suppl 2):379–384. https://doi.org/10.1227/01.NEU.0000327023.18220.88
Bari ME, Haider G, Malik K, Waqas M, Mahmood SF, Siddiqui M (2017) Outcomes of post-neurosurgical ventriculostomy-associated infections. Surg Neurol Int 8:124. https://doi.org/10.4103/sni.sni_440_16
Cui Z, Wang B, Zhong Z, Sun Y, Sun Q, Yang G, Bian L (2015) Impact of antibiotic- and silver-impregnated external ventricular drains on the risk of infections: a systematic review and meta-analysis. Am J Infect Control 43(7):e23–e32. https://doi.org/10.1016/j.ajic.2015.03.015
Li, J., Fu, Y., Zhang, J., Wang, Y., Zhao, Y., Fan, X., . . . Li, C. (2019). Efficacy of tigecycline monotherapy versus combination therapy with other antimicrobials against carbapenem-resistant Acinetobacter baumannii sequence type 2 in Heilongjiang Province. Ann Palliat Med, 8(5), 651-659. https://doi.org/10.21037/apm.2019.11.06
Li Z, An Y, Li L, Yi H (2022) Intrathecal injection of tigecycline and polymyxin B in the treatment of extensively drug-resistant intracranial Acinetobacter baumannii infection: a case report and review of the literature. Infect Drug Resist 15:1411–1423. https://doi.org/10.2147/IDR.S354460
Li X, Sun S, Ling X, Chen K, Wang Q, Zhao Z (2017) Plasma and cerebrospinal fluid population pharmacokinetics of vancomycin in postoperative neurosurgical patients after combined intravenous and intraventricular administration. Eur J Clin Pharmacol 73(12):1599–1607. https://doi.org/10.1007/s00228-017-2313-4
Ye J, Tan LH, Shen ZP, Yu YS, Lai DM, Fan J, Shu Q (2020) Polymyxin for the treatment of intracranial infections of extensively drug-resistant bacteria in children after neurosurgical operation. World J Pediatr 16(5):528–532. https://doi.org/10.1007/s12519-020-00350-8
McClellan N, Swanson JM, Magnotti LJ, Griffith TW, Wood GC, Croce MA, Boucher BA, Mueller EW, Fabian TC (2015) Adjunctive intraventricular antibiotic therapy for bacterial central nervous system infections in critically ill patients with traumatic brain injury. Ann Pharmacother 49(5):515–522. https://doi.org/10.1177/1060028015570466
Göçmez C, Çelik F, Tekin R, Kamaşak K, Turan Y, Palancı Y, Bozkurt F, Bozkurt M (2014) Evaluation of risk factors affecting hospital-acquired infections in the neurosurgery intensive care unit. Int J Neurosci 124(7):503–508. https://doi.org/10.3109/00207454.2013.863773
Choucha A, Boissonneau S, Beucler N, Graillon T, Ranque S, Bruder N, Fuentes S, Velly L, Dufour H (2023) Meningoencephalitis with refractory intracranial hypertension: consider decompressive craniectomy. J Neurosurg Sci 67(2):248–256. https://doi.org/10.23736/S0390-5616.21.05397-2
Hover AR, Sistrunk WW, Cavagnol RM, Scarrow A, Finley PJ, Kroencke AD, Walker JL (2014) Effectiveness and cost of failure mode and effects analysis methodology to reduce neurosurgical site infections. Am J Med Qual 29(6):517–521. https://doi.org/10.1177/1062860613505680
Acknowledgements
The authors wish to thank all the patients and their families who participated in the study.
Funding
This study was funded by the National Natural Science Foundation of China (Grant No. 81972153 and 82120108018), Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD, Grant No. JX10231803), Gusu School, Nanjing Medical University (GSKY202201010), Jiangsu Province’s Key Discipline of Medicine (Grant No. XK201117), and Jiangsu Province Innovative Team (Grant No. NR17).
Author information
Authors and Affiliations
Contributions
Jing Ji: conceptualization, methodology, software. Zhen Yue: data curation, writing—original draft preparation. Liqing Bi: visualization, investigation. Xiaohui Zhi: supervision, software. Lin Zhao: validation, writing—reviewing and editing.
Corresponding author
Ethics declarations
Ethics approval
The research protocol was approved by our hospital ethical committee (No. 2022-NT-07).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
The authors affirm that human research participants provided informed consent for publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yue, Z., Zhi, X., Bi, L. et al. Treatment and prognostic risk factors for intracranial infection after craniocerebral surgery. Neurosurg Rev 46, 199 (2023). https://doi.org/10.1007/s10143-023-02106-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10143-023-02106-0