Abstract
Objective
It has been reported recently that correlation between brain tissue oxygen (PbtO2) and cerebral perfusion pressure (CPP) may serve as an indicator of cerebral autoregulation after subarachnoid hemorrhage. We aimed to compare similar indices describing interaction between changes in intracranial pressure (ICP), arterial blood pressure (ABP), and brain tissue oxygen to verify their clinical utility in patients after traumatic brain injury.
Materials and Methods
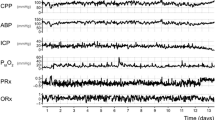
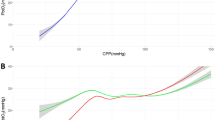
Retrospective analysis of multimodal monitoring of 32 patients suffering from head injury, admitted in the Neurosciences Critical Care Unit, Addenbrooke’s Hospital, Cambridge, UK. Initial 24 h intervals of continuous ABP, ICP, and PbtO2 recordings were analyzed. Index of tissue oxygen reactivity ORx was evaluated as the correlation coefficient between PbtO2 and CPP over a period of 60 min and compared to the index of pressure reactivity PRx. “Optimal CPP” and a hypothetical “optimal PbtO2” were defined as the ranges of CPP and PbtO2 at which PRx or ORx were indicating best cerebrovascular milieu.
Results
PRx and ORx mean values did not show any correlation with each other (R = 0.012; P = 0.95) between patients. There was also no correlation between ORx and PbtO2 (R = 0.098; P = 0.61) and between PRx and PbtO2 (R = 0.019; P = 0.923). No clear and consistent value of “optimal CPP” minimizing ORx or of hypothetical “optimal PbtO2” were found analyzing PbtO2 or ORx trend over the 24 h of monitoring. However, in most of patients ‘optimal CPP’ has been found for PRx index. The same has been confirmed when the data from whole monitoring period were analyzed. There was no correlation between values of ‘optimal CPP’ assessed using ORx and ‘optimal CPP’ assessed with PRx.
Conclusion
The relationships between PbtO2, ORx, and CPP in head injury appear less useful than reported before for patients after subarachnoid hemorrhage.



Similar content being viewed by others
References
Czosnyka M, Balestrieri M, Steiner L, Smielewski P, Hutchinson PJ, Matta B, et al. Age, intracranial pressure, autoregulation, and outcome after brain injury. J Neurosurg. 2005;102:450–1.
Menon DK. Cerebral protection in severe head injury: physiological determinants of outcome and their optimisation. Br Med Bull. 1999;55(1):226–58. doi:10.1258/0007142991902231.
Steiner LA, Czosnyka M, Piechnik SK, et al. Continuous monitoring of cerebrovascular pressure reactivity allows determination of optimal cerebral perfusion pressure in patients with traumatic brain injury. Crit Care Med. 2002;30:733–8. doi:10.1097/00003246-200204000-00002.
Czosnyka M, Smielewski P, Kirkpatrick P, Laing RJ, Menon D, Pickard JD. Continuous assessment of the cerebral vasomotor reactivity in head injury. Neurosurgery. 1997;41:11–9. doi:10.1097/00006123-199707000-00005.
Jaeger M, Schuhmann MU, Soehl M, Nagel C, Meixensberger J. Continuous monitoring of cerebrovascular autoregulation after subarachnoid hemorrhage by brain tissue oxygen pressure reactivity and its relation to delayed cerebral infarction. Stroke. 2007;38:981–6. doi:10.1161/01.STR.0000257964.65743.99.
Jaeger M, Soehle M, Schuhmann MU, Winkler D, Meixensberger J. Correlation of continuously monitored regional cerebral blood flow and brain tissue oxygen. Acta Neurochir (Wien). 2005;147:51–6. doi:10.1007/s00701-004-0408-z.
Kiening KL, Unterberg AW, Bardty TF, Schneider GH, Lanksch WR. Monitoring of cerebral oxygen in patients with severe head injuries: brain tissue PtO2 versus jugular vein oxygen saturation. J Neurosurg. 1996;85:751–7.
Dings J, Meixensberger J, Jager A, Roosen K. Clinical experience with 118 brain tissue oxygen partial pressure catheter probes. Neurosurgery. 1998;43:1082–95. doi:10.1097/00006123-199811000-00045.
Lang EW, Mulvey JM, Mudaliar Y, Dorsch NWC. Direct cerebral oxygen monitoring: a systematic review of recent publications. Neurosurg Rev. 2007;30:99–107. doi:10.1007/s10143-006-0062-4.
Hoelper BM, Alessandri B, Heimann A, Behr R, Kempski O. Brain oxygen monitoring: in vitro accuracy, long term drift and response-time of licox and Neurotrend sensor. Acta Neurochir (Wien). 2005;147:767–74. doi:10.1007/s00701-005-0512-8.
Jaeger M, Schuhmann MU, Soehle M, Meixensberger J. Continuous assessment of cerebrovascular autoregulation after traumatic brain injury using brain tissue oxygen pressure reactivity. Crit Care Med. 2006;34(6):1783–8. doi:10.1097/01.CCM.0000218413.51546.9E.
Sarrafzadeh AS, Kiening KL, Bardt TF, Schneider GH, Unterberg AW, Lanksch WR. Cerebral oxygen in contusioned vs. nonlesioned brain tissue: monitoring of PtiO2 with Licox and Paratrend. Acta Neurochir Suppl (Wien). 1998;71:186–9.
Valadka AB, Hlatky R, Furuya Y, Robertson CS. Brain tissue PO2: correlation with cerebral blood flow. Acta Neurochir Suppl (Wien). 2002;81:299–301.
Hemphill JIII, Knudson M, Derugin N, Morabito D, GeoffreyTM. Carbon dioxide reactivity and pressure autoregulation of brain tissue oxygen. Neurosurgery. 2001;48(2):377–83. doi:10.1097/00006123-200102000-00028.
Hemphill JCIII, Smith WS, Sonne CD, Morabito D, Geoffry TM. Relationship between brain tissue oxygen tension and CT perfusion: feasibility and initial results. AJNR Am J Neuroradiol. 2005;26:1095–100.
Sahuquillo J, Amoros S, Santos A, Poca MA, Panzardo H, Domínguez L, et al. Does an increase in cerebral perfusion pressure always mean a better oxygenated brain? A study in head-injured patients. Acta Neurochir Suppl (Wien). 2000;76:457–62.
Acknowledgment
Many thanks are due to all Addenbrooke’s Hospital Neurocritical Care Staff for their incredible help and understanding we experienced during this study. ICMplus is a software licensed by Cambridge University Enterprise Ltd (www.neurosurg.cam.ac.uk/icmplus); PS and MC have financial interest in a fraction of licensing fee.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Radolovich, D.K., Czosnyka, M., Timofeev, I. et al. Reactivity of Brain Tissue Oxygen to Change in Cerebral Perfusion Pressure in Head Injured Patients. Neurocrit Care 10, 274–279 (2009). https://doi.org/10.1007/s12028-009-9190-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-009-9190-3