Abstract
Introduction
Catheter-associated infection of cerebrospinal fluid (CSF) is a potentially life-threatening complication of external ventricular drainage (EVD). The purpose of this pilot study was to address the efficacy of silver-impregnated EVD catheters in neurological and neurosurgical patients requiring external CSF drainage due to acute occlusive hydrocephalus.
Methods
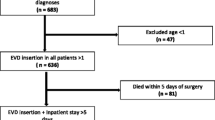
Nineteen consecutive patients were enrolled in the treatment arm of the study and data were prospectively recorded for these patients. The control group consisted of 20 patients for whom data were retrospectively assessed. CSF samples were drawn at least three times a week and routine bacterial cultures and CSF analyses were done according to standard protocols. The primary endpoint of the study was the occurrence of catheter-associated ventriculitis (CAV) proven by positive CSF culture. Secondary endpoints were bacterial colonization of the catheter tip and CSF pleocytosis.
Results
In 20 control patients, 5 CAVs were microbiologically diagnosed. In contrast, no positive CSF cultures were found in the treatment group. This difference was statistically significant (P < 0.05). All CAVs occurred later than day 10 after catheter placement. Colonization of the catheter tip was found in 6 patients in the control group and in 5 patients in the treatment group (not significant).
Conclusions
This pilot study indicates that EVD catheters impregnated with silver nanoparticles might be a new option for preventing CAV in neurocritical care patients, and therefore evaluation in a large prospective randomized study is warranted.


Similar content being viewed by others
References
Munson EL, Heard SO, Doern GV. In vitro exposure of bacteria to antimicrobial impregnated-central venous catheters does not directly lead to the emergence of antimicrobial resistance. Chest 2004;126(5):1628–35.
Furno F, Morley KS, Wong B, et al. Silver nanoparticles and polymeric medical devices: a new approach to prevention of infection? J Antimicrob Chemoth 2004;54(6):1019–24.
Kim TN, Feng QL, Kim JO, et al. Antimicrobial effects of metal ions (Ag+, Cu2+, Zn2+) in hydroxyapatite. J Mater Sci Mater Med 1998;9(3):129–34.
Collart D, Mehrabi S, Robinson L, Kepner B, Mintz EA. Efficacy of oligodynamic metals in the control of bacteria growth in humidifier water tanks and mist droplets. J Water Health 2006;4(2):149–56.
v Naegeli K. Über oligodynamische Erscheinungen in lebenden Zellen. Deutsch Schr Schweiz Naturforsch Ges 1893;33:174.
Slawson RM, Lee H, Trevors JT. Bacterial interactions with silver. Biol Met 1990;3(3–4):151–4.
Stoiser B, Kofler J, Staudinger T, et al. Contamination of central venous catheters in immunocompromised patients: a comparison between two different types of central venous catheters. J Hosp Infect 2002;50(3):202–6.
Galiano K, Pleifer C, Engelhardt K, et al. Silver segregation and bacterial growth of intraventricular catheters impregnated with silver nanoparticles in cerebrospinal fluid drainages. Neurol Res 2007 [Epub ahead of print].
Keong N, Richards H, Farringdon M, Hutchinson P, Pickard J, Kirkpatrick P. Silver trial—Interim results. Acta Neurochir (Wien) 2007; Abstract book of the 13th Congress of the EANS (Glasgow).
External Ventricular Drain (Ventriculostomy). In: Sander Connolly E, McKhann GM, Huang J, Choudhri TF, editors. Fundamentals of operative techniques in neurosurgery. New York: Thieme; 2002. p. 627–34.
Pfausler B, Beer R, Engelhardt K, Kemmler G, Mohsenipour I, Schmutzhard E. Cell index—a new parameter for the early diagnosis of ventriculostomy (external ventricular drainage)-related ventriculitis in patients with intraventricular hemorrhage? Acta Neurochir (Wien) 2004;146(5):477–81.
Sherertz RJ, Raad II, Belani A, et al. Three-year experience with sonicated vascular catheter cultures in a clinical microbiology laboratory. J Clin Microbiol 1990;28(1):76–82.
Bogdahn U, Lau W, Hassel W, Gunreben G, Mertens HG, Brawanski A. Continuous-pressure controlled, external ventricular drainage for treatment of acute hydrocephalus—evaluation of risk factors. Neurosurgery 1992;31(5):898–903.
Wyler AR, Kelly WA. Use of antibiotics with external ventriculostomies. J Neurosurg 1972;37(2):185–7.
Lozier AP, Sciacca RR, Romagnoli MF, Connolly ES Jr. Ventriculostomy-related infections: a critical review of the literature. Neurosurgery 2002;51(1):170–81.
Schultz M, Moore K, Foote AW. Bacterial ventriculitis and duration of ventriculostomy catheter insertion. J Neurosci Nurs 1993;25(3):158–64.
Hader WJ, Steinbok P. The value of routine cultures of the cerebrospinal fluid in patients with external ventricular drains. Neurosurgery 2000;46(5):1149–53.
Broessner G, Helbok R, Lackner P, et al. Survival and long-term functional outcome in 1155 consecutive neurocritical care patients. Crit Care Med 2007;35(9):2025–30.
Zabramski JM, Whiting D, Darouiche RO, et al. Efficacy of antimicrobial-impregnated external ventricular drain catheters: a prospective, randomized, controlled trial. J Neurosurg 2003;98(4):725–30.
Pfisterer W, Muhlbauer M, Czech T, Reinprecht A. Early diagnosis of external ventricular drainage infection: results of a prospective study. J Neurol Neurosurg Psychiatry 2003;74(7):929–32.
Kalfon P, de VC, Samba D, et al. Comparison of silver-impregnated with standard multi-lumen central venous catheters in critically ill patients. Crit Care Med 2007;35(4):1032–9.
Kim KS. Pathogenesis of bacterial meningitis: from bacteraemia to neuronal injury. Nat Rev Neurosci 2003;4(5):376–85.
Bota DP, Lefranc F, Vilallobos HR, Brimioulle S, Vincent JL. Ventriculostomy-related infections in critically ill patients: a 6-year experience. J Neurosurg 2005;103(3):468–72.
McFadden JT. Tissue reactions to standard neurosurgical metallic implants. J Neurosurg 1972;36(5):598–603.
von Holst H, Collins P, Steiner L. Titanium, silver, and tantalum clips in brain tissue. Acta Neurochir (Wien) 1981;56(3–4):239–42.
Acknowledgment
Spiegelberg (GmbH & Co.) KG, 21079 Hamburg, Germany, kindly provided silver-impregnated EVDs (Silverline Antimicrobial Ventricular Catheter) free of charge.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lackner, P., Beer, R., Broessner, G. et al. Efficacy of Silver Nanoparticles-Impregnated External Ventricular Drain Catheters in Patients with Acute Occlusive Hydrocephalus. Neurocrit Care 8, 360–365 (2008). https://doi.org/10.1007/s12028-008-9071-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-008-9071-1