Abstract
Background
A biopsy is the final step in the diagnosis of sarcomas. Complete resection of the biopsy tract traditionally has been recommended in musculoskeletal oncology guidelines, as that tract is considered potentially seeded with tumor cells. However, to our knowledge, the frequency and implications of contamination of the biopsy tract—specifically with respect to the likelihood of local recurrence—and the factors that affect cell seeding are not well described.
Questions/purposes
We asked: (1) How often are biopsy tracts contaminated with pathologically detectable tumor cells at the time of tumor resection? (2) What factors, in particular biopsy type (open versus percutaneous), are associated with tumoral seeding? (3) Is biopsy tract contamination associated with local recurrence?
Methods
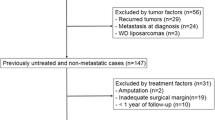
This is a retrospective study of a database with patient data collected from a single center between 2000 and 2013. We treated 221 patients with sarcomas. A total of 27 patients (12%) were excluded and 14 (6%) were lost to followup. One hundred eighty patients finally were included in the analysis who either had biopsies at our center (112) or biopsies at outside institutions (68). Of those performed at our center, 15 (13%) were open and 97 (87%) were percutaneous; of those at outside centers, those numbers were 47 (69%) and 21 (31%) respectively. Median followup was 40 months (range, 24–152 months). During the study period, we generally performed percutaneous biopsies as a standard practice for the diagnosis of bone and soft tissue sarcomas and open biopsies were done when the percutaneous procedure failed to provide a histologic characterization. The mean age of the population was 48 years (range, 7–87 years); 60% were male; 42% had bone sarcomas. Nineteen patients had preoperative radiotherapy and 56 had postoperative radiotherapy. Fifty-seven patients received neoadjuvant chemotherapy and 73 had adjuvant chemotherapy. We determined what proportion of biopsy tracts were contaminated by pathologic analysis of the biopsy tract specimen; during the period in question, our routine practice was to excise the biopsy tract whenever possible at the time of the definitive resection. Using the logistic regression test and Mantel-Haenszel test, we compared open with percutaneous biopsies in terms of the proportion of those that were contaminated at our site and for outside referral biopsies separately, because we do not assume the level of expertise was the same (our site is a referral tumor center). We compared the local recurrence-free survival between patients with and without contamination and between open and percutaneous biopsies using the Kaplan Meier test, again separating those performed at our site from those referred for purposes of this analysis.
Results
Twenty-one of 180 biopsy tracts were contaminated (12%). Twenty of 62 (32%) of the open biopsies and one of 118 (0.8%) of the percutaneous core needle biopsies had cell seeding (odds ratio [OR], 56; 95% CI, 7–428; p < 0.001. One of 97 (1%) percutaneous biopsies performed in our center, and none of the 21 (0%) percutaneous biopsies performed in other centers had contaminated biopsy tracts (p = 0.047). Two of 15 (13%) open biopsies performed at our center and 18 of 41(38%) open biopsies performed at other centers had contaminated biopsy tracts (OR, 4; 95% CI, 1–7; p = 0.001). Four of 74 (5%) bone sarcomas and 18 of 106 (17%) soft tissue sarcomas had biopsy tract contamination (OR, 3; 95% CI, 1–10; p = 0.023). The local recurrence-free survival was longer for patients without contaminated tracts (mean, 107 months; 95% CI, 74–141 months) than for those with biopsy tract seeding (mean, 11 months; 95% CI, 1–20 months; p < 0.001).
Conclusions
Open biopsies were associated with an increased risk of tumoral seeding of the biopsy site, and tumoral seeding was associated with an increased risk of local recurrence. However, it is possible that other factors, such as increased complexity of the tumor or a difficult location, influenced the decision to obtain an open biopsy. Even so, based on these results, we believe that higher risk of local recurrence may be caused by an incomplete biopsy tract resection. In our opinion, the percutaneous biopsy with neoadjuvant or adjuvant therapy is the preferred method of biopsy at our center.
Level of Evidence
Level III, therapeutic study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It commonly is assumed in musculoskeletal oncology [3, 5, 14] that the biopsy tract must be resected together with the tumor in limb-sparing surgery for sarcomas. Some authors have recommended contamination of a biopsy tract as an indication for amputation when the biopsy tract is impossible to include in the surgical approach, affects the neurovascular bundle, or wide margins are not possible [14, 15]. Oncologic surgeons now use different types of biopsies, which create different kinds of biopsy tracts. The scar from a percutaneous core needle biopsy is a puncture of the surface, but in deep tissues it has a tridimensional shape that is difficult to predict reliably. The accuracy of core needle biopsies ranges from 77% to 97% in published series [16, 17, 22, 28–34]. It is excellent for bone sarcomas (77%–96%) and possibly less so for soft tissue sarcomas (76%–78%). However, the sensitivity in soft tissue sarcomas improves with image-guided core needle biopsy (special contrast-enhanced ultrasound) and with a pathologist with extensive experience working with limited samples [7, 17, 19]. The accuracy of open biopsies is close to 100% in some reported series [1, 17, 21], but the cost and the possibility of complications are higher [1, 2, 17, 21]. They are used more commonly in centers without experienced sarcoma experts [1, 2, 17]. An open biopsy produces a longitudinal scar that may be variable in morphologic features and direction.
Some authors have suggested that complete resection of the percutaneous biopsy tract rarely is achieved [10]. Although resection of the biopsy tract is recommended by numerous authors [5, 13, 14], neither we nor Oliveira et al. [20] could find a study that definitively confirmed the frequency of biopsy tract seeding or that there is increased risk of local recurrence when the biopsy tract is not resected.
We performed a pathologic analysis of the musculoskeletal sarcoma biopsy tracts of patients treated at our institution during 2000 to 2013. The main objective was to identify factors associated with contamination. We define “contaminated biopsy tracts” or “biopsy tract seeding” as those in which the pathologists actually find tumor (viable or necrotic) cell nests anywhere in the resected biopsy tract of the main tumor at the time of definitive resection. The secondary objective was to detect the relevance of tumor seeding in local recurrence-free survival of the series. We asked the following questions: (1) How often are biopsy tracts contaminated with pathologically detectable tumor cells at the time of tumor resection? (2) What factors, in particular biopsy type (open versus percutaneous), are associated with tumoral seeding? (3) Is biopsy tract contamination associated with local recurrence?
Patients and Methods
After institutional ethical board approval, we performed a study in which we included 221 patients with bone and soft tissue sarcomas treated at our tertiary referral musculoskeletal oncology center from March 2000 until March 2013. This is a retrospective observational study of prospectively collected data of the medical records, surgical protocols, radiologic studies, and pathologist reports. Forty-one of the 221 patients were excluded; 14 were lost to followup and therefore not included for analysis. The samples of four patients were ulcerated or infected and therefore these four patients were not eligible for inclusion in the study. Twenty-three biopsy tracts were not resected because either the biopsy was performed at another hospital and we were not able to find the scar, or the scar resection would have led to an ablative surgery and the patient rejected amputation. Apart from these cases just mentioned, during this period, our practice was to excise and histologically examine the biopsy tract at the time of definitive resection of the sarcoma. We included all the patients with a diagnosed musculoskeletal sarcoma who had their final surgery at our hospital even if the biopsy had been performed elsewhere before the referral (Table 1). Median followup was 40 months (range, 24–152 months).
During this study period, of the biopsies performed at our center and included in this series, 15 of 112 (13%) were open and 97 of 112 (87 %) were percutaneous; of those at outside centers, those numbers were 47 of 68 (69%) and 21 of 68 (31%), respectively. During the study period, we generally performed percutaneous biopsies as a standard practice for the diagnosis of bone and soft tissue sarcomas and open biopsies when the percutaneous procedure failed to provide a histologic characterization. We compared open with percutaneous biopsies, in terms of the proportion of those that were contaminated, for our institution and for outside referral biopsies separately, as we do not assume the level of expertise was the same (our institution is a referral tumor center). We compared local recurrence-free survival between patients with and without contamination and between open and percutaneous biopsies, again separating those performed at our institution from those referred, for purposes of this analysis.
If the patient was referred from another center, our pathology team reviewed the samples to determine if a new biopsy was needed. We routinely performed core needle biopsies as standard procedure for histologic diagnosis of bone and soft tissue tumors. Two senior musculoskeletal radiologists performed all the biopsies (DB-T, MTV). Bone biopsies were performed in most cases using CT guidance, but also targeted to the periphery of the tumor. In some cases with cortical breakout, ultrasound guidance was used. Bone biopsy was performed using a T-Lok™ ultrasound-guided (Argon Medical Devices, Plano, TX, USA) or a Bonopty™ (AprioMed, Uppsala, Sweden) coaxial needle.
For soft tissue malignancies biopsy, we use ultrasound Doppler color guidance targeted to the most vascularized area and in some cases we also use contrast-enhanced ultrasound. In a soft tissue sarcoma, this area usually corresponds to the periphery of the tumor. The majority of soft tissue biopsies were performed using a coaxial technique, that is, by inserting an introducer or sheath to the edge of the lesion or just inside the lesion and then advancing a cutting needle through the introducer or sheath into the lesion to obtain the biopsy samples. From 2000 to 2010 a TruCore-II™ (Argon Medical Devices) was used; since 2010 we use the Speedybell coaxial biopsy system (Biopsybell Srl, Mirandola, Italy) to infiltrate the periosteal layer.
Needle size depends on the difficulty in obtaining a representative tumor sample (myxoid, heterogeneous tumors, or necrotic tumors), but usually a 16-gauge needle is used to get thick cylinders of tumor and only two or three passes are made. Samples usually were placed in a 10% formalin solution and hand-delivered to the pathology unit for analysis. However, each case is reviewed during weekly meetings before the biopsy to determine the number of samples, the approach [12], and the delivery (fresh or formalin). At our center, the same oncologic orthopaedic team performing surgery on the patient also performs all the open biopsies when they are needed. The patients who are referred are discussed during a weekly meeting [9, 27]; if the open biopsy was performed in line with the predicted incision and the surgeon was aware of the possible neoplastic nature of the lesion, the biopsy was considered to have been correctly performed. If the open biopsy is not considered appropriate (ie, not performed correctly) and limb-sparing surgery is still possible, we plan a wider soft tissue resection (often together with plastic surgery).
Nineteen patients had preoperative radiotherapy and 56 had postoperative radiotherapy. We considered preoperative radiotherapy as a possible bias in the adjusted analysis because some authors [4] point to radiotherapy and chemotherapy as being probable influences to biopsy tract contamination. They did not resect the core needle biopsy in 59 patients with neoadjuvant therapies.
The biopsy tract was resected together with the tumor following the standard of treatment for a wide oncologic resection. We could identify the scar of the percutaneous biopsy tract because it was labeled with India ink in the dermis. In the final surgery, we use the images (ultrasound, CT-guided biopsies) if they are available and manual palpation to include the deep tract as completely as possible. The margins of the main tumor resection were evaluated. We consider the margins wide when the distance between the closest border and the pseudocapsule is wider than 1 cm or 2 mm with anatomic barriers (periosteal layer, epineurium, fascia, or vessel adventitia). The sample is sent to the same pathologists (FLB, JJPK) and reviewed independently macro- and microscopically (Fig. 1). The technique used in pathologic analysis consists of cutting 2-mm parallel blocks of all tissue surrounding the macroscopic scar and the 2-mm blocks were cut in 4-μ thick sections, stained with hematoxylin and eosin, and the pathologist specifically searched for a tumoral cell nest in the sample. Immunohistochemical tests were used if necessary for histologic characterization. The tumor stage is recorded according to the American Joint Committee on Cancer 2010 and Enneking classification for bone sarcomas [8]. The patients were evaluated with MRI and CT every 3 months for 2 years, then every 6 months until 5 years, and finally annually. Bone sarcomas with prosthesis reconstruction also are evaluated with a bone scan and ultrasonography every 6 months. Median followup was 40 months (range, 24–152 months).
Descriptive statistics were analyzed. The statistical analysis was performed using SPSS software, Version 16.0 (SPSS, Chicago, IL, USA). We used a univariate chi-square test for each variable. We analyzed separately, with the Mantel-Haenszel test, contamination of the open and percutaneous biopsies performed at our center and those performed in other hospitals. We performed a multivariable analysis using the logistic regression proportional model to detect the factors that can affect biopsy tract contamination. We also compared the local recurrence-free survival in patients with and without biopsy tract seeding using the Kaplan-Meier method using the log-rank test. Statistical significance was accepted as a probability less than 0.05.
Results
Twenty-one of the 180 samples (12%) were contaminated, with macroscopically detectable cell nests in two and microscopically detectable cell nests in 19. One of the 21 contaminated biopsy tracts was from a percutaneous biopsy (0.8% contamination rate). One of 97 (1%) percutaneous biopsies performed at our center and none of the 21 (0%) percutaneous biopsies performed at other centers had tumoral cell seeding (p = 0.047). This one patient with a contaminated needle biopsy had a Grade 1 chondrosarcoma and underwent extended intralesional resection with high-speed burring and phenol. The biopsy was performed to confirm that this patient had a low-grade, rather than high-grade, chondrosarcoma. The patient has 4 years of followup and no evidence of disease. The other 20 of 21 contaminated biopsy tracts were from open biopsies (32%) (mean, 55 months; 95% CI, (7–428 months; p < 0.001).
Open biopsies were more likely to be contaminated than percutaneous biopsies, among the patients whose biopsies we performed and those whose biopsies were performed at referral centers. Two of 15 (13%) open biopsies performed at our center and 18 of 41(38%) open biopsies performed at other centers had contaminated biopsy tracts (p = 0.001; odds ratio [OR], 4; 95% CI, 1–7). Other factors associated with an increased risk of biopsy tract contamination were soft tissue sarcoma and biopsies performed at other centers before the patient was referred to us (Appendix 1. Supplemental material is available with the online version of CORR ®.) Four of 74 (5%) bone sarcomas and 18 of 106 (17%) soft tissue sarcomas had biopsy tract contamination (OR, 3; 95% CI, 1–10; p = 0.023). We could not find differences in the following variables: age, sex, location, grade, stage, neoadjuvant chemotherapy, number of percutaneous core needle biopsies, tumor resection margins, or time from the biopsy until definitive surgery. None of the patients with preoperative radiotherapy had a contaminated biopsy tract. The center where the biopsy initially was performed was not a factor for biopsy tract contamination in the multivariable analysis. However, the bone or soft tissue sarcoma and the type of biopsy are independent factors (Table 2).
The local recurrence-free survival was longer for patients without contaminated tracts (mean, 107 months; 95% CI, 74–141 months) than in those with biopsy tract seeding (mean, 11 months; 95% CI, 1–20 months; p < 0.001) (Fig. 2). The local recurrence-free survival did not show statistical differences between patients with percutaneous and open biopsies, neither at our center nor in patients whose biopsies were performed at another hospital. With the numbers we had, we could not show a difference in local recurrence-free survival in percutaneous biopsies (mean, 102 months; SD, 12 months; 95% CI, 77–127 months) compared with open biopsies (mean, 98 months; SD, 10 months; 95% CI, 80–117 months; p = 0.252) (Fig. 3). We also did not observe a difference in local recurrence-free survival between patients who had their biopsy at our hospital or at other hospitals.
Discussion
The biopsy is a key step in the diagnosis of sarcomas as incorrectly performed biopsies might result in more ablative final operations or might compromise the oncologic resection [14, 15]. Guidelines recommend biopsy tract resection in the definitive surgery to achieve complete elimination of malignant cells [5, 13, 14]. To our knowledge, and as reported by Oliveira et al. [20], contamination of the tract and the factors that can affect seeding have not been reported. We detected contamination with tumoral cells in 12% of the biopsy tracts. Tumoral cell seeding increased in open biopsies performed at referral centers or at our center. The local recurrence-free survival was longer in patients without contamination of the biopsy tract.
There are limitations in this study. First, the retrospective design may have resulted in some selection bias in terms of which patients received open biopsies and which patients underwent percutaneous biopsies. At our center, open biopsies were performed when we did not achieve a diagnosis after at least two percutaneous procedures. Thirty-eight percent of the biopsies were performed elsewhere, consequently we cannot confirm the biopsy technique in those patients. We obviously do not know exactly why patients whose biopsies were performed at outside centers received an open or a percutaneous biopsy, but it is possible that patients with more-complicated or less-accessible tumors underwent open biopsies, and this could have accounted for some of the increased contamination we observed with open biopsies. Even so, the open biopsies performed at our center also showed a higher contamination rate and the multivariate analysis showed that the type of biopsy procedure (open or percutaneous) was associated with the contamination, whereas the center where the biopsy was performed did not correspond to the contamination rate. Second, there was a relatively small and heterogeneous group of patients with disparate diagnoses that prevents statistical analysis of the effect of the histologic diagnosis, and we also looked at bone and soft tissue tumors together. In this series, we observed higher contamination in soft tissue sarcomas compared with bone sarcomas. Nevertheless, a larger study comprised of all bone tumors or all soft tissue tumors might provide different results. Finally, we did not have enough patients who received preoperative radiotherapy to determine if it might have had an effect on contamination of the biopsy tract. However none of the patients who received preoperative radiation had contamination of the biopsy tract. This variable should be cleared in further study.
The rate of biopsy tract seeding in our series was 12%. There are some published cases of tumor recurrence in the path of no resected or incompletely resected percutaneous and open biopsy tracts [6, 9, 24, 35]. Ribeiro et al. [23] reported contamination of 32% of the biopsy tracts in the largest series with 25 bone and soft tissue sarcomas.
Our study shows that the possibility of contamination is present in open and percutaneous biopsies, but the likelihood is greater with open than with percutaneous procedures. This difference is independent of the hospital where the biopsy is performed, as the possibility remained when we compared percutaneous and open procedures done at our center and at other centers. Other studies also show a high risk of contamination of open biopsies [18, 23]. Saghieh et al. [25] reported 10 cases in pediatric patients in which the percutaneous core needle biopsy tract was not resected and the patients did not have any recurrence. Li et al. [12] suggested decreasing contamination of the percutaneous biopsy tracts in patients with osteosarcoma by using Adriamycin sponges.
When we looked for other factors associated with contamination, we found that soft tissue sarcomas showed higher biopsy tract contamination than bone sarcomas. This factor may be related to the biopsy technique or to the histologic characteristic of each tumor that could not be analyzed separately in this study. Although in our study this factor did not reach statistical significance, other studies have indicated that radiotherapy may decrease tumor tissue contamination near the biopsy pathway [6, 18, 26]. Nevertheless more studies would be necessary to define the influence of adjuvant therapies (chemotherapy/radiotherapy). Binitie et al. [4] did not address the relative effect of each of the adjuvant treatments or the effect of these treatments in open biopsy tracts. Moreover, they did not compare the local recurrence rate in their series with that of patients without resected biopsies who did not receive any adjuvant therapy.
In our study, the local recurrence-free survival was higher in patients with contaminated biopsy tracts, although with the numbers we had, we could not show a difference in local recurrence-free survival in patients who had percutaneous compared with open biopsies. We did not show a difference, when considered separately, biopsies performed at our institution and at other hospitals. It may be attributable to the low number of open biopsies performed at our center, but local recurrence is a complex event that can be affected by other factors, therefore more specific studies are needed to clarify these results.
Percutaneous core needle biopsies can cause contamination in a resected biopsy tract, but the percentage of contaminated samples was much lower in our series than with open biopsy, at our center and among patients referred to us from outside centers for care. We found that patients with a contaminated biopsy tract has shorter local recurrence-free survival than those with a noncontaminated biopsy tract. This might indicate that wider margins are needed around open biopsy tracts than was done in our patients. Resecting the biopsy tract completely may be a difficult task because its tridimensional shape may be difficult to predict reliably during the definitive surgery. Jalgaonkar et al. [11] reported that the biopsy tract was impossible to find after 3 months in 22 of 45 patients (48.8%) when they did not mark it with India ink. With open biopsies, the tridimensional shape of the scar is not always as expected, and the hematoma, which may have tumoral cells, can reach distant tissues. In our opinion, although we can ascertain this proposition, we suspect we are not able to completely resect a substantial number of biopsy pathways.
The treating surgeon should assess the biopsy tract carefully when planning definitive resection. More study is needed to assess the potential benefits of adjuvant treatments in preventing local recurrence, especially in patients who have had an open biopsy. Percutaneous core needle biopsies appear to be a safer approach to establishing the diagnosis of a musculoskeletal neoplasm.
References
Altuntas A, Slavin J, Smith P, Schlict S, Powell G, Ngan S, Toner G, Choong PF. Accuracy of computed tomography guided core needle biopsy of musculoskeletal tumours. ANZ J Surg. 2005;75:187–191.
Barrientos Ruiz I, Serrano Montilla J. Ortiz-Cruz EJ. [Cost analysis of the diagnosis and treatment of soft tissue sarcomas in reference centres][in Spanish]. Rev Esp Cir Ortop Traumatol. 2012;56:374–377.
Bickels J, Jelinek J, Shmookler B, Malawer M. Biopsy of Musculoskeletal Tumors. In Malawer MM, Sugarbaker PH, eds. Musculoskeletal Cancer Surgery Treatment of Sarcomas and Allied Diseases. Dordrecht, The Netherlands: Kluwer Academic Publishers; 2001:37–45.
Binitie O, Tejiram S, Conway S, Cheong D, Temple HT, Letson GD. Adult soft tissue sarcoma local recurrence after adjuvant treatment without resection of percutaneous core needle biopsies tract. Clin Orthop Relat Res. 2013;471:891–898.
Campanacci M. Giant Cell Tumor. Bone and Soft Tissue Tumors: Clinical Features, Imaging, Pathology and Treatment. 2nd ed. Wien, Germany: Springer-Verlag; 1999:99–142.
Davies NM, Livesley PJ, Cannon SR. Recurrence of an osteosarcoma in a needle biopsy track. J Bone Joint Surg Br. 1993;75:977–978.
De Marchi A, Brach del Prever EM, Linari A, Pozza S, Verga L, Albertini U, Forni M, Gino GC, Comandone A, Brach del Prever AM, Piana R, Faletti C. Accuracy of core-needle biopsy after contrast-enhanced ultrasound in soft-tissue tumours. Eur Radiol. 2010;20:2740–2748.
Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, eds. AJCC cancer Staging Manual. 7th ed. New York, NY: Springer; 2010.
Huang AJ, Kattapuram SV. Musculoskeletal neoplasms: biopsy and intervention. Radiol Clin North Am. 2011;49:1287–1305.
Iemsawatdikul K, Gooding CA, Twomey EL, Kim GE, Goldsby RE, Cohen I, O’Donnell RJ. Seeding of osteosarcoma in the biopsy tract of a patient with multifocal osteosarcoma. Pediatr Radiol. 2005;35:717–721.
Jalgaonkar A, Dawson-Bowling SJ, Mohan AT, Spiegelberg B, Saifuddin A, Pollock R, Skinner JA, Briggs TW, Aston W. Identification of the biopsy track in musculoskeletal tumour surgery: a novel technique using India ink. Bone Joint J. 2013;95:250–253.
Li ZF, Li JM, Yan J, Yang ZP, Li X, Yang Q. Prevention of contamination by biopsy needle track contamination using a novel adriamycin-loaded gelatin sponge. World J Surg Oncol. 2013;11:169.
Liu PT, Valadez SD, Chivers FS, Roberts CC, Beauchamp CP. Anatomically based guidelines for percutaneous core needle biopsies of bone tumors: implications for limb-sparing surgery. Radiographics. 2007;27:189–205; discussion 206.
Mankin HJ, Lange TA, Spanier SS. The hazards of biopsy in patients with malignant primary bone and soft-tissue tumors. J Bone Joint Surg Am. 1982;64:1121–1127.
Mankin HJ, Mankin CJ, Simon MA. The hazards of the biopsy, revisited: members of the Musculoskeletal Tumor Society. J Bone Joint Surg Am. 1996;78:656–663.
Mitton B, Seeger LL, Eckardt MA, Motamedi K, Eilber FC, Nelson SD, Eckardt JJ, Federman N. Image-guided percutaneous core needle biopsy of musculoskeletal tumors in children. J Pediatr Hematol Oncol. 2014;36:337–341.
Mitsuyoshi G1, Naito N, Kawai A, Kunisada T, Yoshida A, Yanai H, Dendo S, Yoshino T, Kanazawa S, Ozaki T. Accurate diagnosis of musculoskeletal lesions by core needle biopsy. J Surg Oncol. 2006;94:21–27.
Mohana R, Faisham W, Zulmi W, Nawfar AS, Effat O, Salzihan MS. The incidence of malignant infiltration in the biopsy tract of osteosarcoma. Malays Orthop J. 2007;1:7–10.
Narvani AA, Tsiridis E, Saifuddin A, Briggs T, Cannon S. Does image guidance improve accuracy of core needle biopsy in diagnosis of soft tissue tumours? Acta Orthop Belg. 2009;75:239–244.
Oliveira MP, de Andrade Lima PM, DA Silva HJ, Viera de Mello RJ. Neoplasm seeding in biopsy tract of the musculoskeletal system: a systematic review. Acta Ortop Bras. 2014;22:106–110.
Pohlig F, Kirchhoff C, Lenze U, Schauwecker J, Burgkart R, Rechl H, von Eisenhart-Rothe R. Percutaneous core needle biopsy versus open biopsy in diagnostics of bone and soft tissue sarcoma: a retrospective study. Eur J Med Res. 2012;17:29.
Puri A, Shingade VU, Agarwal MG, Anchan C, Juvekar S, Desai S, Jambhekar NA. CT-guided percutaneous core needle biopsy in deep seated musculoskeletal lesions: a prospective study of 128 cases. Skeletal Radiol. 2006;35:138–143.
Ribeiro MB, de Oliveira CR, Filippi RZ, Baptista AM, Caiero MT, Saito CF, Barbosa do Nascimento SA, de Camargo OP. Histopathological study on biopsy track in malignant musculoskeletal tumors. Acta Ortop Bras. 2009;17:279–281.
Robertson EG, Baxter G. Tumour seeding following percutaneous needle biopsy: the real story! Clin Radiol. 2011;66:1007–1014.
Saghieh S, Masrouha KZ, Musallam KM, Mahfouz R, Abboud M, Khoury NJ, Haidar R. The risk of local recurrence along the percutaneous core-needle biopsy tract in patients with bone sarcomas. Iowa Orthop J. 2010;30:80–83.
Schwartz HS, Spengler DM. Needle tract recurrences after closed biopsy for sarcoma: three cases and review of the literature. Ann Surg Oncol. 1997; 4:228–236.
Siegel GW, Biermann JS, Chugh R, Jacobson JA, Lucas D, Feng M, Chang AC, Smith SR, Wong SL, Hasen J. The multidisciplinary management of bone and soft tissue sarcoma: an essential organizational framework. J Multidiscip Healthc. 2015;8:109–115.
Simon MA, Biermann JS. Biopsy of bone and soft-tissue lesions. J Bone Joint Surg Am. 1993;75:616–621.
Skrzynski MC, Biermann JS, Montag A, Simon MA. Diagnostic accuracy and charge-savings of outpatient core needle biopsy compared with open biopsy of musculoskeletal tumors. J Bone Joint Surg Am. 1996;78:644–649.
Sung KS, Seo SW, Shon MS. The diagnostic value of needle biopsy for musculoskeletal lesions. Int Orthop. 2009;33:1701–1706.
Verheijen P, Witjes H, van Gorp J, Hennipman A, van Dalen T. Current pathology work-up of extremity soft tissue sarcomas: evaluation of the validity of different techniques. Eur J Surg Oncol. 2010;36:95–99.
Welker JA, Henshaw RM, Jelinek J, Shmookler BM, Malawer MM. The percutaneous core needle biopsy is safe and recommended in the diagnosis of musculoskeletal masses. Cancer. 2000;89:2677–2686.
Wu JS, Goldsmith JD, Horwich PJ, Shetty SK, Hochman MG. Bone and soft-tissue lesions: what factors affect diagnosis yield of image-guided core-needle biopsy? Radiology. 2008;248:962–970.
Yang J, Frassica FJ, Fayad L, Clark DP, Weber KL. Analysis of nondiagnostic results after image-guided needle biopsies of musculoskeletal lesions. Clin Orthop Relat Res. 2010;468:3103–3111.
Zocalli C, Prencipe U, Erba F, Vidiri A, Di Filippo F. Biopsy can determinate tumoral track contamination: a case report of chondrosarcoma. Eur J Radiol Extra. 2009;72:e79–e81.
Acknowledgements
We thank the biostatistics department of Hospital La Paz, specially, Rosario Madero PhD, for contribution to the analysis of the data in our study. We also thank Mar Tapia Viñedas MD (Radiology Department, University Hospital La Paz) for her contribution to the biopsy procedures and Fernando Lopez-Barea MD, PhD (Pathology Department, University Hospital La Paz) for his contribution to the biopsy tract review.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution has or waived for the human protocol for this investigation and that all investigations were conducted in conformity with ethical and confidentiality principles of research.
This work was performed at the Musculoskeletal Tumor Unit, Orthopaedics and Traumatology Department, at La Paz University Hospital, Madrid, Spain.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Barrientos-Ruiz, I., Ortiz-Cruz, E.J., Serrano-Montilla, J. et al. Are Biopsy Tracts a Concern for Seeding and Local Recurrence in Sarcomas?. Clin Orthop Relat Res 475, 511–518 (2017). https://doi.org/10.1007/s11999-016-5090-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-016-5090-y