Abstract
Background
Despite dislocation being the most frequent complication after revision THA, risk factors for its occurrence are not completely understood.
Questions/purposes
We therefore (1) determined the overall risk of dislocation after revision THA in a large series of revision THAs using contemporary revision techniques, (2) identified patient-related risk factors predicting dislocation, and (3) identified surgical variables predicting dislocation.
Methods
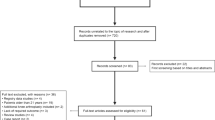
We performed 1211 revision THAs between June 2004 and October 2010 in 576 women and 415 men who had a mean age of 64.7 years (range, 25–95 years) at time of surgery. Forty-six (4%) were lost to followup and 13 died (1%), leaving 1152 hips followed for a minimum of 90 days (mean, 2 years; range, 90 days to 7.1 years). Multivariate logistic regression was performed to identify risk factors for dislocation. The model was also tested on patients followed for a minimum 1 year to assess any difference in longer followup.
Results
One hundred thirteen patients dislocated over the followup period (9.8%). Factors that were different between patients who dislocated and those who remained stable included a history of at least one previous dislocation (odds ratio [OR] = 2.673), abductor deficiency (OR = 2.672), and Paprosky acetabulum class (OR = 1.522). Use of a constrained liner (OR = 0.503) and increased femoral head size (OR = 0.942) were protective against dislocation, while with longer followup a constrained liner was no longer significant.
Conclusions
Dislocation remains a common problem after revision THA. Identifying these risk factors can assist in patient education and surgical planning. Recognition of these risk factors in both patient type and surgical strategy is important for the surgeon performing revision THA and for minimizing these risks.
Level of Evidence
Level IV, therapeutic study. See Instructions for Authors for a complete description of levels of evidence.


Similar content being viewed by others
References
Alberton GM, High WA, Morrey BF. Dislocation after revision total hip arthroplasty: an analysis of risk factors and treatment options. J Bone Joint Surg Am. 2002;84:1788–1792.
Biviji AA, Ezzet KA, Pulido P, Colwell CW Jr. Modular femoral head and liner exchange for the unstable total hip arthroplasty. J Arthroplasty. 2009;24:625–630.
Carter AH, Sheehan EC, Mortazavi SM, Purtill JJ, Sharkey PF, Parvizi J. Revision for recurrent instability: what are the predictors of failure? J Arthroplasty. 2011;26(6 suppl):46–52.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Cogan A, Klouche S, Mamoudy P, Sariali E. Total hip arthroplasty dislocation rate following isolated cup revision using Hueter’s direct anterior approach on a fracture table. Orthop Traumatol Surg Res. 2011;97:501–505.
Della Valle CJ, Paprosky WG. The femur in revision total hip arthroplasty evaluation and classification. Clin Orthop Relat Res. 2004;420:55–62.
Ejsted R, Olsen NJ. Revision of failed total hip arthroplasty. J Bone Joint Surg Br. 1987;69:57–60.
Garbuz DS, Masri BA, Duncan CP, Greidanus NV, Bohm ER, Petrak MJ, Della Valle CJ, Gross AE. The Frank Stinchfield Award. Dislocation in revision THA: do large heads (36 and 40 mm) result in reduced dislocation rates in a randomized clinical trial? Clin Orthop Relat Res. 2012;470:351–356.
Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755.
Kaplan SJ, Thomas WH, Poss R. Trochanteric advancement for recurrent dislocation after total hip arthroplasty. J Arthroplasty. 1987;2:119–124.
Kavanagh BF, Ilstrup DM, Fitzgerald RH. Revision total hip arthroplasty. J Bone Joint Surg Am. 1985;67:517–526.
Khatod M, Barber T, Paxton E, Namba R, Fithian D. An analysis of the risk of hip dislocation with a contemporary total joint registry. Clin Orthop Relat Res. 2006;447:19–23.
Kung PL, Ries MD. Effect of femoral head size and abductors on dislocation after revision THA. Clin Orthop Relat Res. 2007;465:170–174.
Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785.
Mahomed NN, Barrett JA, Katz JN, Phillips CB, Losina E, Lew RA, Guadagnoli E, Harris WH, Poss R, Baron JA. Rates and outcomes of primary and revision total hip replacement in the United States Medicare population. J Bone Joint Surg Am. 2003;85:27–32.
Morrey BF. Instability after total hip arthroplasty. Orthop Clin North Am. 1992;23:237–248.
Murray TG, Wetters NG, Moric M, Sporer SM, Paprosky WG, Della Valle CJ. The Use of Abduction Bracing for Early Postoperative Dislocation Prevention Following Revision Total Hip Arthroplasty. J Arthroplasty. 2012 May 17 [Epub ahead of print].
Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty: a 6-year follow-up evaluation. J Arthroplasty. 1994;9:33–44.
Saadat E, Diekmann G, Takemoto S, Ries MD. Is an algorithmic approach to the treatment of recurrent dislocation after THA effective? Clin Orthop Relat Res. 2012;470:482–489.
Sah AP, Estok DM 2nd. Dislocation rate after conversion from hip hemiarthroplasty to total hip arthroplasty. J Bone Joint Surg Am. 2008;90:506–516.
Springer BD, Fehring TK, Griffin WL, Odum SM, Masonis JL. Why revision total hip arthroplasty fails. Clin Orthop Relat Res. 2009;467:166–173.
Toomey SD, Hopper RH Jr, McAuley JP, Engh CA. Modular component exchange for treatment of recurrent dislocation of a total hip replacement in selected patients. J Bone Joint Surg Am. 2001;83:1529–1533.
Weiss RJ, Beckman MO, Enocson A, Schmalholz A, Stark A. Minimum 5-year follow-up of a cementless, modular, tapered stem in hip revision arthroplasty. J Arthroplasty. 2011;26:16–23.
Acknowledgments
The authors thank Vamsi Kancherla, MD, for his invaluable help with this research.
Author information
Authors and Affiliations
Corresponding author
Additional information
The institution of one or more of the authors (SMS, WGP, CJDV) has received, during the study period, funding from Zimmer Inc (Warsaw, IN, USA), Smith & Nephew Inc (Memphis, TN, USA), and Stryker Orthopaedics (Mahwah, NJ, USA).
One of the authors (TGM) certifies that he, or a member of his immediate family, has received or may receive payments or benefits, during the study period, an amount of less than $10,000, from Zimmer Inc. One of the authors (SMS) certifies that he, or a member of his immediate family, has received or may receive payments or benefits, during the study period, an amount of $10,000 to $100,000, from Smith & Nephew. One of the authors (WGP) certifies that he, or a member of his immediate family, has received or may receive payments or benefits, during the study period, an amount of $100,001 to $1,000,000, from Zimmer Inc; and an amount of $10,000 to $100,000, from Biomet Inc (Warsaw, IN, USA). One of the authors (CJDV) certifies that he, or a member of his immediate family, has received or may receive payments or benefits, during the study period, an amount of $10,000 to $100,000, from Biomet; an amount of $10,000 to $100,000, from Smith & Nephew; and an amount of less than $10,000, from Convatec (Skillman, NJ, USA). Each remaining author (NGW, MM) certifies that he or she, or a member of his or her immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Rush University Medical Center, Chicago, IL, USA.
About this article
Cite this article
Wetters, N.G., Murray, T.G., Moric, M. et al. Risk Factors for Dislocation After Revision Total Hip Arthroplasty. Clin Orthop Relat Res 471, 410–416 (2013). https://doi.org/10.1007/s11999-012-2561-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-012-2561-7