Abstract
Comorbidity may be defined as the association of two or more diseases in individuals at a frequency greater than that expected statistically by chance. Studying the co-occurrence of two disorders requires a careful statistical analysis before any clear conclusion on causality is reached. Many studies have looked for an association between migraine and many diseases, reporting several sometimes controversial comorbidities in migraine subjects. Although migraine is more common in women than in men, very few studies have analyzed the comorbidity of perimenstrual migraine, a migraine sub-type characterized by attacks of migraine without aura related to menstruation. We review the studies on migraine comorbidities, particularly migraine without aura in women.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Yoon MS, Katsarava Z, Obermann M et al. Prevalence of primary headaches in Germany: results of the German Headache Consortium Study. J Headache Pain 2012;13:215–23.
Martin VT. New theories in the pathogenesis of menstrual migraine. Curr Pain Headache Rep. 2008;12:453–62.
The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004;24 Suppl 1:9–160.
Granella F, Sances G, Allais G, et al. Characteristics of menstrual and non menstrual attacks in women with menstrually related migraine referred to headache centres. Cephalalgia. 2004;24:707–16.
Martin VT, Lipton RB. Epidemiology and biology of menstrual migraine. Headache. 2008;48 Suppl 3:S124–30.
Dowson AJ, Kilminster SG, Salt R, et al. Disability associated with headaches occurring inside and outside the menstrual period in those with migraine: a general practice study. Headache. 2005;45:277–82.
Martin VT, Wernke S, Mandell K, et al. Defining the relationship between ovarian hormones and migraine headache. Headache. 2005;45:1190–201.
Etminan M, Takkouche B, Isoma FC, et al. Risk of ischaemic stroke in people with migraine: systematic review and meta-analysis of observational studies. BMJ. 2005;330:63. doi:10.1136/bmj.38302.504063.8F.
•• Schurks M, Rist PM, Bigal ME, et al. Migraine and cardiovascular disease: systematic review and meta-analysis. BMJ. 2009;339:b3914. This meta-analysis on migraine and cardiovascular disease is the latest and more comprehensive work on this topic.
Spector JT, Kahn SR, Jones MR, et al. Migraine headache and ischemic stroke risk: an updated meta-analysis. Am J Med. 2010;123:612–24.
•• Kurth T, Chabriat H, Bousser MG. Migraine and stroke: a complex association with clinical implications. Lancet Neurol. 2012;11:92–100. This excellent review describes the evidence linking migraine and stroke and discusses the diagnostic and therapeutic implications of the association between these disorders.
Bigal ME, Kurth T, Hu H, et al. Migraine and cardiovascular disease. Possible mechanism of interaction. Neurology. 2009;72(26):1864–71.
Schwedt TJ, Demaerschalk BM, Dodick DW. Patent foramen ovale and migraine: a quantitative systematic review. Cephalalgia. 2008;28:531–40.
Kruit MC, van Buchem MA, Launer LJ, et al. Migraine is associated with an increased risk of deep white matter lesions, subclinical posterior circulation infarcts and brain iron accumulation. The population-based MRI CAMERA study. Cephalalgia. 2010;30:129–36.
Scher AI, Gudmundsson LS, Sigurdsson S, et al. Migraine headache in middle-age and late-life brain infarcts. JAMA. 2009;301(24):2563–70.
Jacome DE. Blepharoclonus, pseudoasterixis, and restless feet. Am J Med Sci. 2001;322:137–40.
Tison F, Crochard A, Leger D, et al. Epidemiology of restless legs syndrome in French adults: a nationwide survey: the INSTANT study. Neurology. 2005;65:239–46.
Högl B, Kiechl S, Willeit J, et al. Restless legs syndrome: a community-based study of prevalence, severity, and risk factors. Neurology. 2005;64:1920–4.
Cannon PR, Larner AJ. Migraine and restless legs syndrome: is there an association? J Headache Pain. 2011;12:405–9.
Rhode AM, Hosing VG, Happe S, et al. Comorbidity of migraine and restless legs syndrome: a case–control study. Cephalalgia. 2007;27:1255–60.
d’Onofrio F, Bussone G, Cologno D, et al. Restless legs syndrome and primary headaches: a clinical study. Neurol Sci. 2008;29 Suppl 1:S169–72.
Suzuki S, Suzuki K, Miyamoto M, et al. Evaluation of contributing factors to restless legs syndrome in migraine patients. J Neurol. 2011;258:2016–35.
Larner J. Migraine with aura and restless legs syndrome. J Headache Pain. 2007;8:141–2.
Tartarotti S, Kallweit U, Bassetti L. Association of restless leg syndrome, chronic motor tic disorder and migraine with aura: a case of a single family. J Neurol. 2010;257:1043–4.
D’Onofrio F, Cologno D, Petretta V, Finocchi C, Autunno M, Marsala G, Usai S, Grazzi L, Omboni S, Fofi L, Barbanti P, Bussone G. Restless legs syndrome is not associated with migraine with aura: a clinical study. Neurol Sci. 2011;32(S1):S153–6.
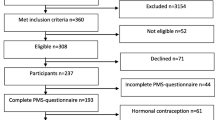
Pierangeli G, Cevoli S, Vignatelli L, et al. Sleep-related movement disorders in menstrual migraine patients: a case–control study. Neurol Sci. 2008;29:S199.
Rasmussen BK. Migraine and tension-type headache in a general population: precipitating factors, female hormones, sleep pattern and relation to lifestyle. Pain. 1993;53:65–72.
Radat F, Swendsen J. Psychiatric comorbidity in migraine: a review. Cephalagia. 2004;25:165–78.
Breslau N, Davis GC. Migraine, physical health and psychiatric disorder: a prospective epidemiologic study in young adults. J Psychiatr Res. 1993;27:211–21.
Merikangas KR, Merikangas JR, Angst J. Headache syndrome and psychiatric disorders: association and familial transmission. J Psychiatr Res. 1993;27:197–210.
Merikangas KR, Angst J. Migraine and psychopathology, results of the Zurich Cohort Study of Young adults. Arch General Psychiatry. 1990;47:849–53.
Breslau N, Davis GC, Schultz LR, et al. Migraine and major depression. Headache. 1994;34:387–93.
Breslau N, Schultz LR, Stewart WF, et al. Headache and major depression. Is the association specific to migraine? Neurology. 2000;54:308–13.
Victor TW, Hu X, Campbell J, et al. Association between migraine, anxiety and depression. Cephalalgia. 2010;30:567–75.
Radat F, Sahk D, Lutz G, et al. Psychiatric comorbidity is related to headache induced by chronic substance use in migraineurs. Headache. 1999;39:477–80.
Juang KD, Wang SJ, Fuh JL, et al. Comorbidity of depressive and anxiety disorders in chronic daily headache and its subtypes. Headache. 2000;40:818–23.
Waraich P, Goldner EM, Somers JM, et al. Prevalence and incidence of mood disorders: A systematic review of the literature. Can J Psychiatry. 2004;49:124–38.
Somers JM, Goldner EM, Waraich P, et al. Prevalence and incidence studies of anxiety disorders: a systematic review of the literature. Can J Psychiatry. 2006;51:100–13.
Jette N, Patten S, William J, et al. Comorbidity of migraine and psychiatric disorders- a national population-based study. Headache. 2008;48:501–16.
Oedegaard KJ, Dilsaver SC, Hundal O, et al. Are migraine and bipolar disorders comorbid phenomena?: findings from a pharmacoepidemiological study using the Norwegian Prescription Database. J Clin Psychopharmacol. 2011;31(6):734–9.
Nicodemo M, Vignatelli L, Grimaldi D, et al. Quality of life, eating and mood disorders in menstrual migraine: a case–control study. Neurol Sci. 2008;29(Suppl):S155–7.
Seidel S, Karwautz A, Gudrun W, et al. Migraine in patients with eating disorders: a study using a sister-pair comparison design. Headache. 2011;51:220–5.
D’Andrea G, Ostuzzi R, Francesconi F, et al. Migraine prevalence in eating disorders and pathophysiological correlations. Neurol Sci. 2009;30 Suppl 1:S55–9.
Brewerton TD, George MS. Is migraine related to the eating disorders? Int J Eat Disord. 1993;14(1):75–9.
De Simone R, Ranieri A, Marano E. Migraine and epilepsy: clinical and pathophysiological relations. Neurol Sci. 2007;28:S150–5.
•• Wang SJ, Chen PK, Fuh JL. Comorbidities of migraine. Front Neurol. 2010;1:16. This review focuses on the findings of common comorbid disorders of migraine and includes all disorders, from stroke and coronary heart disease to psychiatric diseases and other uncommon disorders.
Ottman R, Lipton RB. Comorbidity of migraine and epilepsy. Neurology. 1994;44:2105–10.
Karaali-Savrun F, Goksan B, Yeni SN, et al. Seizure related headache in patients with epilepsy. Seizure. 2002;11:67–9.
Nuyen J, Schellevis FG, Satariano WA, et al. Comorbidity was associated with neurologic and psychiatric diseases: a general practice-based controlled study. J Clin Epidemiol. 2006;59:1274–84.
Brodtkorb E, Bakken IJ, Sjaastad O. Comorbidity of migraine and epilepsy in a Norwegian community. Eur J Neurol. 2008;15:1421–3.
• Tonini MC, Giordano L, Atzeni L et al. Primary headache and epilepsy: a multicenter crosssectional study. Epilepsy Behav 2012; 23:342–347. This multicenter cross-sectional study is well designed to analyze an hypothetical linkage between migraine and epilepsy.
Dworetzky BA, Townsend MK, Pennell PB, et al. Female reproductive factors and risk of seizure or epilepsy: data from the Nurses’ Health Study II. Epilepsia. 2012;53:e1–e-4.
Evans RW, de Tommaso M. Migraine and fibromyalgia. Headache. 2011;51:295–9.
Ifergane G, Buskila D, Simiseshvely N, et al. Prevalence of fibromyalgia syndrome in migraine patients. Cephalalgia. 2005;26:451–6.
de Tommaso M, Sardaro M, Serpino C, et al. Fibromyalgia comorbidity. Cephalalgia. 2009;29:453–64.
Tervila L, Marttila P. Headache as a symptom of endometriosis externa. Ann Chir Gynaecol Fenn. 1975;64:239–41.
Ferrero S, Pretta S, Bertoldi S, et al. Increased frequency of migraine among women with endometriosis. Hum Reprod. 2004;19:2927–32.
Nylton DR, Gillespie NG, Merikangas KR, et al. Common genetic influences underlie comorbidity of migraine and endometriosis. Genet Epidemiol. 2009;33:105–13.
Dickerson LM, et al. Premenstrual syndrome. Am Fam Physician. 2003;67(8):1743–52.
MacGregor EA. Perimenstrual headaches: unmet needs. Curr Pain Headache Rep. 2008;12:468–74.
Facchinetti F, Allai G, Nappi RE, et al. Migraine is a risk factor for hypertensive disorders in pregnancy: a prospective cohort study. Cephalalgia. 2008;29:286–92.
Marozio L, Facchinetti F, Allais G, et al. Headache and pregnancy outcome: a prospective study. Eur J Obstet Gynecol Reprod Biol. 2012;161(2):140–3.
Evans RW, Williams MA, Rapoport AM, et al. The association of obesity with episodic and chronic migraine. Headache. 2012;52:663–71.
Bigal ME, Liberman JN, Lipton RB. Obesity and migraine: a population study. Neurology. 2006;66:545–50.
Bigal ME, Lipton RB, Holland PR, et al. Obesity, migraine and chronic migraine: possible mechanism of interaction. Neurology. 2007;68:1851–61.
Winter AC, Berger K, Buring JE, et al. Body mass index, migraine, migraine frequency and migraine features in women. Cephalalgia. 2009;29:269–78.
Ford ES, Li C, Pearson WS, et al. Body mass index and headaches: findings from a national sample of US adults. Cephalalgia. 2008;28:1270–6.
Peterlin BL, Rosso AL, Rapoport AM, et al. Obesity and migraine: the effect of age, gender and adipose tissue distribution. Headache. 2010;50:52–62.
• Charbit AR, Akerman S, Goadsby PJ. Dopamine: what’s new in migraine? Curr Opin Neurol. 2010;23(3):275–81. This original review summarizes the current understanding of dopamine in migraine, its role in migraine pathophysiology, and implications in menstrual migraine.
Stiasny-Kolster K, Trenkwalder C, Fogel W, et al. Restless legs syndrome—new insights into clinical charateristics, pathophysiology, and treatment options. J Neurol. 2004;251:39–43.
•• MacGregor EA, Rosenberg JD, Kurth T. Sex-related differences in epidemiological and clinic-based headache studies. Headache. 2011;51:843–59. This critical paper reviews the evidence for differences between men and women on a broad range of parameters with a particular focus on migraine.
Disclosures
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nicodemo, M., Cevoli, S., Giannini, G. et al. Comorbidity in Perimenstrual Migraine. Curr Pain Headache Rep 16, 477–483 (2012). https://doi.org/10.1007/s11916-012-0281-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11916-012-0281-z