Abstract
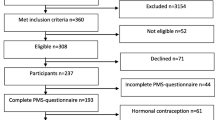
Migraine attacks increase during the perimenstrual period in approximately half of female migraineurs. There are differences in the pathogenesis and clinical features of menstrually related and non-menstrual migraine attacks. The objective of this study was to compare the characteristics of migraine in patients with menstrually related and non-menstrual migraine, and to investigate the differences between premenstrual, menstrual, and late-menstrual migraine attacks. Three-hundred and thirty-two women with migraine without aura were evaluated using questionnaires and diaries to determine the characteristics of headache, preceding and accompanying symptoms, and the relation of migraine attacks and menstruation. One-hundred and sixty-three women had menstrually related migraine without aura (49.1%). Duration of disease and duration of headache were longer (p = 0.002 and p < 0.001, respectively), and nausea, vomiting, phonophobia, and aggravation of headache with physical activity were more frequent in patients with menstrually related migraine (p = 0.005, p = 0.006, p < 0.001 and p = 0.006, respectively). Premonitory symptoms and allodynia were observed more frequently in the menstrually related migraine group (p = 0.012 and p = 0.004, respectively). Perimenstrual migraine attacks occurred premenstrually (days −2 and −1) in 46 patients (25.3%), menstrually (days 1 to 3) in 90 patients (49.4%), and late menstrually (days 4 to 7) in 19 patients (10.4%). Our results showed that the duration of headache was longer and accompanying symptoms were more frequent and diverse in patients with menstrually related migraine without aura, suggesting that these findings may reflect the increase in excitability or susceptibility of the brain in these patients.
Similar content being viewed by others
References
Bille B (1962) Migraine in school children. A study of the incidence and short-term prognosis, and a clinical, psychological and electroencephalographic comparison between children with migraine and matched controls. Acta Paedatr Suppl 136:1–151
Victor TW, Hu X, Campbell JC, Buse DC, Lipton RB (2010) Migraine prevalence by age and sex in the United States: a life-span study. Cephalalgia 30(9):1065–1072
Lipton RB, Stewart WF, Diamond S, Diamond ML, Reed M (2001) Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Headache 41(7):646–657
Stewart WF, Wood C, Reed ML, Roy J, Lipton RB, AMPP Advisory Group (2008) Cumulative lifetime migraine incidence in women and men. Cephalalgia 28(11):1170–1178
Couturier EG, Bomhof MA, Neven AK, van Duijn NP (2003) Menstrual migraine in a representative Dutch population sample: prevalence, disability and treatment. Cephalalgia 23(4):302–308
Granella F, Sances G, Pucci E, Nappi RE, Ghiotto N, Napp G (2000) Migraine with aura and reproductive life events: a case control study. Cephalalgia 20(8):701–707
Wöber C, Holzhammer J, Zeitlhofer J, Wessely P, Wöber-Bingöl C (2006) Trigger factors of migraine and tension-type headache: experience and knowledge of the patients. J Headache Pain 7(4):188–195
MacGregor EA (2012) Classification of perimenstrual headache: clinical relevance. Curr Pain Headache Rep 16(5):452–460
Headache Classification Committee of the International Headache Society (IHS) (2013) The international classification of headache disorders, 3rd edition (beta version). Cephalalgia 33(9):629–808
MacGregor EA, Chia H, Vohrah RC, Wilkinson M (1990) Migraine and menstruation: a pilot study. Cephalalgia 10(6):305–310
Somerville BW (1972) The role of estradiol withdrawal in the etiology of menstrual migraine. Neurology 22(4):355–365
Martin VT, Behbehani M (2006) Ovarian hormones and migraine headache: understanding mechanisms and pathogenesis—part 2. Headache 46(3):365–386
MacGregor EA, Hackshaw A (2004) Prevalence of migraine on each day of the natural menstrual cycle. Neurology 63(2):351–353
MacGregor EA, Victor TW, Hu X, Xiang Q, Puenpatom RA, Chen W, Campbell JC (2010) Characteristics of menstrual vs nonmenstrual migraine: a post hoc, within-woman analysis of the usual-care phase of a nonrandomized menstrual migraine clinical trial. Headache 50(4):528–538
Granella F, Sances G, Allais G, Nappi RE, Tirelli A, Benedetto C, Brundu B, Facchinetti F, Nappi G (2004) Characteristics of menstrual and nonmenstrual attacks in women with menstrually related migraine referred to headache centres. Cephalalgia 24(9):707–716
Pinkerman B, Holroyd K (2010) Menstrual and nonmenstrual migraines differ in women with menstrually-related migraine. Cephalalgia 30(10):1187–1194
Vetvik KG, Benth JŠ, MacGregor EA, Lundqvist C, Russell MB (2015) Menstrual versus non-menstrual attacks of migraine without aura in women with and without menstrual migraine. Cephalalgia 35(14):1261–1268
Martin VT, Wernke S, Mandell K, Ramadan N, Kao L, Bean J, Liu J, Zoma W, Rebar R (2005) Defining the relationship between ovarian hormones and migraine headache. Headache 45(9):1190–1201
MacGregor EA, Frith A, Ellis J, Aspinall L, Hackshaw A (2006) Incidence of migraine relative to menstrual cycle phases of rising and falling estrogen. Neurology 67(12):2154–2158
Pavlović JM, Stewart WF, Bruce CA, Gorman JA, Sun H, Buse DC, Lipton RB (2015) Burden of migraine related to menses: results from the AMPP study. J Headache Pain 16:24
Granella F, Sances G, Zanferrari C, Costa A, Martignoni E, Manzoni GC (1993) Migraine without aura and reproductive life events: a clinical epidemiological study in 1300 women. Headache 33(7):385–389
Dzoljic E, Sipetic S, Vlajinac H, Marinkovic J, Brzakovic B, Pokrajac M, Kostic V (2002) Prevalence of menstrually related migraine and nonmigraine primary headache in female students of Belgrade University. Headache 42(3):185–193
Stewart WF, Lipton RB, Chee E, Sawyer J, Silberstein SD (2000) Menstrual cycle and headache in a population sample of migraineurs. Neurology 55(10):1517–1523
Silberstein SD, Massiou H, McCarroll KA, Lines CR (2002) Further evaluation of rizatriptan in menstrual migraine: retrospective analysis of long-term data. Headache 42(9):917–923
Diamond ML, Cady RK, Mao L, Biondi DM, Finlayson G, Greenberg SJ, Wright P (2008) Characteristics of migraine attacks and responses to almotriptan treatment: a comparison of menstrually related and nonmenstrually related migraines. Headache 48(2):248–258
Vetvik KG, Russell MB (2011) Are menstrual and nonmenstrual migraine attacks different? Curr Pain Headache Rep 15(5):339–342
Güven H, Çilliler AE, Çomoğlu SS (2013) Cutaneous allodynia in patients with episodic migraine. Neurol Sci 34(8):1397–1402
Baykan B, Ekizoglu E, Karli N, Kocasoy-Orhan E, Zarifoglu M, Saip S, Siva A, Ertas M (2016) Characterization of migraineurs having allodynia: results of a large population-based study. Clin J Pain 32(7):631–635
Gazerani P, Andersen OK, Arendt-Nielsen L (2005) A human experimental capsaicin model for trigeminal sensitization. Gender-specific differences. Pain 118(1–2):155–163
Kaube H, Keay KA, Hoskin KL, Bandler R, Goadsby PJ (1993) Expression of c-Fos-like immunoreactivity in the caudal medulla and upper cervical spinal cord following stimulation of the superior sagittal sinus in the cat. Brain Res 629(1):95–102
Ruggiero DA, Underwood MD, Mann JJ, Anwar M, Arango V (2000) The human nucleus of the solitary tract: visceral pathways revealed with an “in vitro” postmortem tracing method. J Auton Nerv Syst 79(2–3):181–190
Kelman L, Tanis D (2006) The relationship between migraine pain and other associated symptoms. Cephalalgia 26(5):548–553
Maniyar FH, Sprenger T, Monteith T, Schankin C, Goadsby PJ (2014) Brain activations in the premonitory phase of nitroglycerin-triggered migraine attacks. Brain 137(Pt 1):232–241
Kannan H, Yamashita H (1985) Connections of neurons in the region of the nucleus tractus solitarius with the hypothalamic paraventricular nucleus: their possible involvement in neural control of the cardiovascular system in rats. Brain Res 329(1–2):205–212
Johannes CB, Linet MS, Stewart WF, Celentano DD, Lipton RB, Szklo M (1995) Relationship of headache to phase of the menstrual cycle among young women: a daily diary study. Neurology 45(6):1076–1082
Wöber C, Brannath W, Schmidt K, Kapitan M, Rudel E, Wessely P, Wöber-Bingöl C, PAMINA Study Group (2007) Prospective analysis of factors related to migraine attacks: the PAMINA study. Cephalalgia 27(4):304–314
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no conflict of interest.
Ethics approval
The study was carried out according to 1964 Helsinki Declaration and was approved by the Institutional Ethics Committee.
Informed consent
All patients participating in the study provided informed consent.
Rights and permissions
About this article
Cite this article
Güven, B., Güven, H. & Çomoğlu, S. Clinical characteristics of menstrually related and non-menstrual migraine. Acta Neurol Belg 117, 671–676 (2017). https://doi.org/10.1007/s13760-017-0802-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-017-0802-y