Abstract
Summary
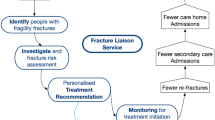
This questionnaire-based study evaluated the reasons for attendance or non-attendance at the fracture liaison service in patients with a recent fracture. Frailty, male sex, living alone, and low education were associated with non-attendance, and the information perceived by the patient was associated with attendance.
Introduction
The purpose of this study was to evaluate hospital registration- and patient-related factors associated with attendance or non-attendance to the Fracture Liaison Service (FLS).
Methods
Out of 1728 consecutive patients registered with a recent fracture at hospital entry, and after exclusion of 440 patients because of death, residence in a nursing home, already on osteoporosis treatment, or recent DXA, 1288 received an FLS invitation. We evaluated the hospital registration of fractures at entry and exit of the hospital. A questionnaire was sent to all invited patients to evaluate factors related to non-attendance (including age, gender, frailty, living alone, income, education, extrinsic motivations (impact of perceived information) and intrinsic motivations (patient’s own perceived views and opinions) and to attendance (personal impact of clinical professionals’ advice).
Results
There were 278 more hospital exit codes than entry codes. Of the 1288 invited patients, 745 returned analyzable questionnaires (537 attenders and 208 non-attenders). Non-attendance was associated with male gender (OR: 2.08, 95% CI: 1.35, 3.21), frailty (OR: 1.62, CI: 1.08, 2.45), living alone (OR:2.05, CI: 1.48, 2.85), low education (OR: 1.82, CI: 1.27, 2.63), not interested in bone strength (OR: 1.85, CI: 1.33, 2.63), and being unaware of increased subsequent fracture risk (OR: 1.75, CI: 1.08, 2.86). Information perceived by the patient was significantly associated with attendance (OR: 3.32, CI: 1.75, 6.27).
Conclusion
Fracture entry registration inaccuracies, male gender, frailty, living alone, having low general education, or low interest in bone health and subsequent fracture risk were independently associated with FLS non-attendance. Adequately perceived advice (to have a bone densitometry and attend the FLS) was strongly associated with FLS attendance.

Similar content being viewed by others
References
Akesson K, Marsh D, Mitchell PJ, McLellan AR, Stenmark J, Pierroz DD, Kyer C, Cooper C (2013) (IOF fracture working group). Capture the fracture®: a best practice framework and global campaign to break the fragility fracture cycle. Osteoporos Int 24(8):2135–2152. https://doi.org/10.1007/s00198-013-2348-z.
Lems WF, Dreinhöfer KE, Bischoff-Ferrari H, Blauth M, Czerwinski E, da Silva J, Herrera A, Hoffmeyer P, Kvien T, Maalouf G, Marsh D, Puget J, Puhl W, Poor G, Rasch L, Roux C, Schüler S, Seriolo B, Tarantino U, van Geel T, Woolf A, Wyers C, Geusens P (2017) EULAR/EFORT recommendations for management of patients older than 50 years with a fragility fracture and prevention of subsequent fractures. Ann Rheum Dis 76(5):802–810. https://doi.org/10.1136/annrheumdis-2016-210289.
Eisman JA, Bogoch ER, Dell R, Harrington JT, McKinney RE Jr, McLellan A, Mitchell PJ, Silverman S, Singleton R, Siris E (2012) Making the first fracture the last fracture: ASBMR task force report on secondary fracture prevention. J Bone Miner Res 27(10):2039–2046. https://doi.org/10.1002/jbmr.1698
McLellan AR, Gallacher SJ, Fraser M, McQuillian C (2003) The fracture liaison service: success of a program for the evaluation and management of patients with osteoporotic fracture. Osteoporos Int 14(12):1028–1034
Ganda K, Puech M, Chen JS, Speerin R, Bleasel J, Center JR, Eisman JA, March L, Seibel MJ (2013) Models of care for the secondary prevention of osteoporotic fractures: a systematic review and meta-analysis. Osteoporos Int 24(2):393–406. https://doi.org/10.1007/s00198-012-2090-y
Luc M, Corriveau H, Boire G, Filiatrault J, Beaulieu MC, Gaboury I (2018) Patient-Related Factors Associated with Adherence to Recommendations Made by a Fracture Liaison Service: A Mixed-Method Prospective Study. Int J Environ Res Public Health 15(5):E944. https://doi.org/10.3390/ijerph15050944
Swart KMA, van Vilsteren M, van Hout W, Draak E, van der Zwaard BC, van der Horst HE, Hugtenburg JG, Elders PJM (2018 Aug 23) Factors related to intentional non-initiation of bisphosphonate treatment in patients with a high fracture risk in primary care: a qualitative study. BMC Fam Pract 19(1):141. https://doi.org/10.1186/s12875-018-0828-0
Eekman DA, van Helden SH, Huisman AM, Verhaar HJ, Bultink IE, Geusens PP, Lips P, Lems WF (2014) Optimizing fracture prevention: the fracture liaison service, an observational study. Osteoporos Int 25(2):701–709. https://doi.org/10.1007/s00198-013-2481-8.
van den Berg P, Schweitzer DH, van Haard PM, van den Bergh JP, Geusens PP (2015) Meeting international standards of secondary fracture prevention: a survey on fracture liaison Services in the Netherlands. Osteoporos Int 26(9):2257–2263. https://doi.org/10.1007/s00198-015-3117-y.
Khosla S, Hofbauer LC (2017) Osteoporosis treatment: recent developments and ongoing challenges. Lancet Diabetes Endocrinol 5(11):898–907. https://doi.org/10.1016/S2213-8587(17)30188-2
Giangregorio L, Thabane L, Cranney A, Adili A, deBeer J, Dolovich L, Adachi JD, Papaioannou A (2010) Osteoporosis knowledge among individuals with recent fragility fracture. Orthop Nurs 29(2):99–107. https://doi.org/10.1097/NOR.0b013e3181d2436c.
Alami S, Hervouet L, Poiraudeau S, Briot K, Roux C (2016) One barriers to effective postmenopausal osteoporosis treatment: a qualitative study of Patients' and Practitioners' views. PLoS One 11(6):e0158365. https://doi.org/10.1371/journal.pone.0158365
Ong T, Tan W, Marshall L, Sahota O (2015) The relationship between socioeconomic status and fracture in a fracture clinic setting: data from the Nottingham fracture liaison service. Injury. 46(2):366–370. https://doi.org/10.1016/j.injury.2014.10.002
Grover ML, Edwards FD, Chang YH, Cook CB, Behrens MC, Dueck AC (2014) Fracture risk perception study: patient self-perceptions of bone health often disagree with calculated fracture risk. Womens Health Issues 24(1):e69–e75. https://doi.org/10.1016/j.whi.2013.11.007
Besser SJ, Anderson JE, Weinman J (2012) How do osteoporosis patients perceive their illness and treatment? Implications for clinical practice. Besser SJ, Anderson JE, Weinman J. Arch Osteoporos 7:115–124. https://doi.org/10.1007/s11657-012-0089-9
Raybould G, Babatunde O, Evans AL, Jordan JL, Paskins Z (2018) Expressed information needs of patients with osteoporosis and/or fragility fractures: a systematic review. Arch Osteoporos 13(1):55. https://doi.org/10.1007/s11657-018-0470-4.
Vranken L, Wyers CE, van den Bergh JPW, Geusens PPMM (2017) The phenotype of patients with a recent fracture: a literature survey of the fracture liaison service. Calcif Tissue Int 101(3):248–258. https://doi.org/10.1007/s00223-017-0284-1.
Dutch Institute for Healthcare Improvement CBO (2011) Richtlijn Osteoporose en Fractuurpreventie. www.diliguide.nl/document/1015/file/pdf/. (Dutch) Assessed 14-02-2018
Gobbens RJ, van Assen MA, Luijkx KG, Wijnen-Sponselee MT, Schols JMJ (2010) The Tilburg frailty Indicator: psychometric properties. Am Med Dir Assoc 11(5):344–355. https://doi.org/10.1016/j.jamda.2009.11.003
https://www.nza.nl/english Assessed 01-03-2018
https://en.nvz-ziekenhuizen.nl/ Assessed 01-03-2018
https://werkenmetdbcs.nza.nl/downloadcentrum-ziekenhuiszorg/infomateriaal/9156-factsheet-dbc-systematiek/file (Dutch). Assessed 01-03-2018
https://chipsoft.com/?Source=https%3A%2F%2Fwww%2Echipsoft%2Enl%2F. Assessed 14-02-2018
Warriner A (2011) Ea. minor, major, low-trauma, and high-trauma fractures: what are the subsequent fracture risks and how do they vary? Curr Osteoporos Rep 9(3):122–128. https://doi.org/10.1007/s11914-011-0064-1
https://www.vmszorg.nl/wp-content/uploads/2017/11/web_2009.0104_praktijkgids_kwetsbare_ouderen.pdf (Dutch) assessed 30-12-2018
Lötters FJ, van den Bergh JP, de Vries F, Rutten-van Mölken MP (2016) Current and Future incidence and costs of osteoporosis-related fractures in the Netherlands: combining claims data with BMD measurements. Calcif Tissue Int 98(3):235–243. https://doi.org/10.1007/s00223-015-0089-z.
Boudreau DM, Yu O, Balasubramanian A, Wirtz H, Grauer A, Crittenden DB, Scholes D (2017) A survey of Women's awareness of and reasons for lack of Postfracture osteoporotic care. J Am Geriatr Soc 65(8):1829–1835. https://doi.org/10.1111/jgs.14921
Bours SP, van Geel TA, Geusens PP, Janssen MJ, Janzing HM, Hoffland GA, Willems PC, van den Bergh JP (2011) Contributors to secondary osteoporosis and metabolic bone diseases in patients presenting with a clinical fracture. J Clin Endocrinol Metab 96(5):1360–1367. https://doi.org/10.1210/jc.2010-2135
Adler RA (2018) Update on osteoporosis in men. Best Pract Res Clin Endocrinol Metab 32(5):759–772. https://doi.org/10.1016/j.beem.2018.05.007
Center JR (2017) Fracture burden: what two and a half decades of Dubbo osteoporosis epidemiology study data reveal about clinical outcomes of osteoporosis. Curr Osteoporos Rep 15(2):88–95. https://doi.org/10.1007/s11914-017-0352-5
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K (2013) Frailty in elderly people. Lancet 381(9868):752–762. https://doi.org/10.1016/S0140-6736(12)62167-9
Li G, Thabane L, Papaioannou A, Ioannidis G, Levine MA, Adachi JD (2017) An overview of osteoporosis and frailty in the elderly. BMC Musculoskelet Disord 18(1):46. https://doi.org/10.1186/s12891-017-1403-x
Blain H, Masud T, Dargent-Molina P, Martin FC, Rosendahl E, van der Velde N, Bousquet J, Benetos A, Cooper C, Kanis JA, Reginster JY, Rizzoli R, Cortet B, Barbagallo M, Dreinhöfer KE, Vellas B, Maggi S, Strandberg T, EUGMS falls and fracture interest group; European Society for Clinical and Economic Aspects of osteoporosis and osteoarthritis (ESCEO), osteoporosis research and information group (GRIO), and international osteoporosis foundation (IOF) (2016) A comprehensive fracture prevention strategy in older adults: the European Union geriatric medicine society (EUGMS) statement. J Nutr Health Aging 20(6):647–652. https://doi.org/10.1007/s12603-016-0741-y
Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G (2004) Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci 59(3):255–263
Theou O, Cann L, Blodgett J, Wallace LM, Brothers TD, Rockwood K (2015) Modifications to the frailty phenotype criteria: systematic review of the current literature and investigation of 262 frailty phenotypes in the survey of health, ageing, and retirement in Europe. Ageing Res Rev 21:78–94. https://doi.org/10.1016/j.arr.2015.04.001
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA (2001) Frailty in older adults: evidence for a phenotype. Cardiovascular health study collaborative research group. J Gerontol A Biol Sci Med Sci 56(3):M146–M156
Li G, Papaioannou A, Thabane L, Cheng J, Adachi JD Frailty change and major osteoporotic fracture in the elderly: data from the global longitudinal study of osteoporosis in women 3-year Hamilton cohort. J Bone Miner Res 31(4):718–724
Li G, Papaioannou A, Thabane L, Levine MAH, Ioannidis G, Wong AKO, Lau A, Adachi JD (2017) Modifying the phenotypic frailty model in predicting risk of major osteoporotic fracture in the elderly. J Am Med Dir Assoc 18(5):414–4199
Weycker D, Edelsberg J, Barron R, Atwood M, Oster G, Crittenden DB, Grauer A (2017) Predictors of near-term fracture in osteoporotic women aged ≥65 years, based on data from the study of osteoporotic fractures. Osteoporos Int 28(9):2565–2571. https://doi.org/10.1007/s00198-017-4103-3
https://www.cbs.nl/en-gb/figures assessed 04-01-2019
Steptoe A, Shankar A, Demakakos P, Wardle J (2013) Social isolation, loneliness, and all-cause mortality in older men and women. Proc Natl Acad Sci U S A 110(15):5797–5801. https://doi.org/10.1073/pnas.1219686110
Ebert JF, Huibers L, Christensen B, Christensen MB (2018) Paper- or web-based questionnaire invitations as a method for data collection: cross-sectional comparative study of differences in response rate, completeness of data, and Financial Cost. J Med Internet Res 20(1):e24. https://doi.org/10.2196/jmir.8353
Acknowledgments
We are grateful to Mrs. Wil Aarssen and Mrs. Maria van Woerden for their excellent secretarial services and to Mrs. Lisette van Hulst for her linguistic advice.
Author information
Authors and Affiliations
Contributions
PVDB, DHS, and PVH are responsible for the study design. PVDB and DHS were the authors, supported by PVH, who also performed all statistical analyses. PG and JVDB supported the process with important scientific contributions.
Corresponding author
Ethics declarations
Ethics
The study was carried out in accordance with the declaration of Helsinki and the guidelines of the International Conference on Harmonization Good Clinical Practice (GCP) after a certificate of no objection approved by the regional Medical Ethical Review Board (METC Zuidwest Holland) no. NL 17.109.
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 430 kb)
Rights and permissions
About this article
Cite this article
van den Berg, P., van Haard, P., Geusens, P. et al. Challenges and opportunities to improve fracture liaison service attendance: fracture registration and patient characteristics and motivations. Osteoporos Int 30, 1597–1606 (2019). https://doi.org/10.1007/s00198-019-05016-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-019-05016-4