Abstract
Purpose of Review
Faster aspart is a new formulation of insulin aspart (IAsp) produced by adding the excipients niacinamide and L-arginine. As this new, “ultra-rapid insulin” is available in the EU-market and Canada, the pharmacokinetic and pharmacodynamics data is summarized.
Recent Findings
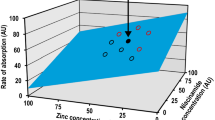
Faster aspart shows an earlier onset of appearance of insulin in the bloodstream after subcutaneous administration and an earlier onset of glucose-lowering action and a higher glycemic effect within the first 30 min. Faster aspart administered by pump is indeed faster than conventional aspart with a faster on (− 11 min), faster off (− 24 min), and more than 100% greater insulin action within the first 30 min. Tolerability of faster aspart is similar to that of Iasp; the same holds true for compatibility in pump use.
Summary
Faster aspart shows a faster occurrence of insulin in the blood compared with IAsp in subcutaneous injection. Improvements over current analogs may be more pronounced in pumps than with injections. Data from phase IIIa studies confirm the reduction of postprandial glucose excursions that can be achieved with faster aspart.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Pandyarajan V, Weiss MA. Design of non-standard insulin analogs for the treatment of diabetes mellitus. Curr Diab Rep. 2012;12(6):697–704.
Heinemann L, Muchmore DB. Ultrafast-acting insulins: state of the art. J Diabetes Sci Technol. 2012;6:728–42.
Heise T. Getting closer to physiologic insulin secretion. Clin Ther. 2007;29(Suppl. D):S161–5.
Overmann H, Heinemann L. Injection-meal interval: recommendations of diabetologists and how patients handle it. Diabetes Res Clin Pract. 1999;43:137–42.
Gallwitz B, Westrup D, Schmeisl G-W. Stellenwert der Insulinanaloga bei der Therapie von Menschen mit Typ-2-Diabetes. DMW. 2014;139:2199–203.
Fullerton B, Siebenhofer A, Jeitler K, Horvath K, Semlitsch T, Berghold A, et al. Short-acting insulin analogues versus regular human insulin for adults with type 1 diabetes mellitus. Cochrane Database Syst Rev. 2016;6:CD012161.
Siebenhofer A, Plank J, Berghold A, Jeitler K, Horvath K, Narath M, et al. Short acting insulin analogues versus regular human insulin in patients with diabetes mellitus. Cochrane Database Syst Rev. 2006;2:CD003287.
Bode BW, Weinstein R, Bell D, et al. Comparison of insulin aspart with buffered regular insulin and insulin lispro in continuous subcutaneous insulin infusion. Diabetes Care. 2002;25:439–44.
Radermecker RP, Scheen AJ. Continuous subcutaneous insulin infusion with short-acting insulin analogues or human regular insulin: efficacy, safety, quality of life, and cost-effectiveness. Diabetes Metab Res Rev. 2004;20(3):178–88.
Brod M, Nikolajsen A, Weatherall J, Pfeiffer KM. Understanding post-prandial hyperglycemia in patients with type 1 and type 2 diabetes: a web-based survey in Germany, the UK, and USA. Diabetes Ther. 2016a;7(2):335–48.
Brod M, Nikolajsen A, Weatherall J, Pfeiffer KM. The economic burden of post-prandial hyperglycemia (PPH) among people with type 1 and type 2 diabetes in three countries. Diabetes Ther. 2016;7(1):75–90.
Cengiz E, Bode B, Van Name M, Tamborlane WV. Moving toward the ideal insulin for insulin pumps. Expert Rev Med Devices. 2016;13(1):57–69.
Andersen G, Alluis B, Meiffren G, Ranson A, Soula O, Seroussi C, Fischer A, et al. The ultra-rapid BioChaperone® lispro shows a faster onset of action and stronger early metabolic effect than Humalog®. EASD 2014, 16th September 2014, Vienna, Austria: Poster #934.
Krasner A, Pohl R, Simms P, Pichotta P, Hauser R, De Souza E. A review of a family of ultra-rapid-acting insulins: formulation development. J Diabetes Sci Technol. 2012;6:786–96.
Frost GI. Recombinant human hyaluronidase (rHuPH20): an enabling platform for subcutaneous drug and fluid administration. Exp Opin Drug Deliv. 2007;4:427–40.
Buckley ST, Jeppesen CB, Olsen HB, Hostrup S, Sturis J. Faster-acting insulin aspart: towards an understanding of the mechanism(s) of action of nicotinamide. Diabetes. 2015;64(Suppl. 1):A262. 1024-P
Buckley ST, Kildegaard J, Høiberg-Nielsen R, Bekker Jeppesen C, Birk Olsen H, Refsgaard HHF, et al. Mechanistic analysis into the mode(s) of action of niacinamide in faster-acting insulin aspart. Diabetes Technol Ther. 2016;18(Suppl.1):A116–7.
Heise T, Haahr H, Jensen L, et al. Faster-acting insulin aspart improves postprandial glycemia vs insulin aspart in patients with type 1 diabetes mellitus (T1DM). Diabetes. 2014;63(Suppl. 1):A34. 129-OR
Heise T, Zijlstra E, Nosek L, LicEng TR, Haahr H. Pharmacological properties of faster-acting insulin aspart vs insulin aspart in patients with type 1 diabetes receiving continuous subcutaneous insulin infusion: a randomized, double-blind, crossover trial. Diabetes Obes Metab. 2016; https://doi.org/10.1111/dom.12803.
Heise T, Stender-Petersen K, Hövelmann U, Bonde Jacobsen J, Nosek L, Zijlstra E, et al. Pharmacokinetic and pharmacodynamic properties of faster-acting insulin aspart versus insulin aspart across a clinically relevant dose range in subjects with type 1 diabetes mellitus. Clin Pharmacokinet. 2016; https://doi.org/10.1007/s40262-016-0473-5.
Heise T, Hövelmann U, Zijlstra E, Stender-Petersen K, Bonde Jacobsen J, Haahr H. A comparison of pharmacokinetic and pharmacodynamic properties between faster-acting insulin aspart and insulin aspart in elderly subjects with type 1 diabetes mellitus. Drugs Aging. 2016; https://doi.org/10.1007/s40266-016-0418-6.
• Bode BW, Johnson JA, Hyveled L, Tamer SC, Demissie M. Improved postprandial glycemic control with faster-acting insulin aspart in patients with type 1 diabetes using continuous subcutaneous insulin infusion. Diabetes Technol Ther. 2017; https://doi.org/10.1089/dia.2016.0350. In this study, the use of faster-acting insulin aspart in insulin pump use is shown
•• Russell-Jones D, Bode BW, De Block C, Franek E, Heller SR, Mathieu C, et al. Fast-acting insulin aspart improves glycemic control in basal-bolus treatment for type 1 diabetes: results of a 26-week multicenter, active-controlled, treat-to-target, randomized, parallel-group trial (onset 1). Diabetes Care. 2017; https://doi.org/10.2337/dc16-1771. This article shows the results of a multicenter real-life study of faster-acting insulin aspart in adults which was the pivotal trial
Bowering K, Case C, Harvey J, Reeves M, Sampson M, Strzinek R, et al. Faster aspart versus insulin aspart as part of a basal-bolus regimen in inadequately controlled type 2 diabetes: the onset 2 trial. Diabetes Care. 2017; https://doi.org/10.2337/dc16-1770.
•• Heise T, Pieber TR, Danne T, Erichsen L, Haahr H. A pooled analysis of clinical pharmacology trials investigating the pharmacokinetic and pharmacodynamic characteristics of fast-acting insulin aspart in adults with type 1 diabetes. Clin Pharmacokinet. 2017;56(5):551–9. https://doi.org/10.1007/s40262-017-0514-8. Heise et al. show data from several studies which show in pooled analysis the time benefit of faster-acting insulin aspart
Fath M, Danne T, Biester T, Erichsen L, Kordonouri O, Haahr H. Faster-acting insulin aspart provides faster onset and greater early exposure vs insulin aspart in children and adolescents with type 1 diabetes mellitus. Pediatr Diabetes. 2017; https://doi.org/10.1111/pedi.12506.
Zijlstra E, Demissie M, Graungaard T, et al. Compatibility and safety of faster-acting insulin aspart used in continuous subcutaneous insulin therapy in patients with type 1 diabetes. The Endocrine Society’s 98th Annual Meeting and Expo, Boston, MA, USA. 1–4 April 2016a: Poster number FRI-697.
Weinzimer SA, Steil GM, Swan KL, Dziura J, Kurtz N, Tamborlane WV. Fully automated closed-loop insulin delivery versus semiautomated hybrid control in pediatric patients with type 1 diabetes using an artificial pancreas. Diabetes Care. 2008b;31:934–9.
Chase HP, Doyle FJ 3rd, Zisser H, Renard E, Nimri R, Control to Range Study Group, et al. Multicenter closed-loop/hybrid meal bolus insulin delivery with type 1 diabetes. Diabetes Technol Ther. 2014;16(10):623–32.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Torben Biester received research support from Medtronic, speaker’s honoraria from Medtronic and Ypsomed, and travel support from Novo Nordisk.
Olga Kordonouri received honoraria for participating on an advisory board of Novo Nordisk as well as speaker’s honoraria from Eli Lilly and Sanofi. She also owns DreaMed stocks.
Thomas Danne reports the following conflicts of interest: AstraZeneca (Speaker, Advisory Panel, Research Support), Boehringer (Speaker, Advisory Panel, Research Support), Bristol-Myers Squibb (Advisory Panel), DexCom (Speaker, Advisory Panel, Research Support), Eli Lilly (Speaker, Advisory Panel, Research Support), Johnson & Johnson (Advisory Panel, Research Support), Medtronic (Speaker, Advisory Panel, Research Support), Novo Nordisk (Speaker, Advisory Panel, Research Support), Roche (Speaker, Advisory Panel, Research Support), Sanofi (Speaker, Advisory Panel, Research Support), Unomedical (Advisory Panel, Research Support), Ypsomed (Speaker, Research Support). Stock Options/Holdings/Board of Directors DreaMed Ltd.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Therapies and New Technologies in the Treatment of Type 1 Diabetes
Rights and permissions
About this article
Cite this article
Biester, T., Kordonouri, O. & Danne, T. Pharmacological Properties of Faster-Acting Insulin Aspart. Curr Diab Rep 17, 101 (2017). https://doi.org/10.1007/s11892-017-0931-y
Published:
DOI: https://doi.org/10.1007/s11892-017-0931-y