Abstract
Purpose of Review
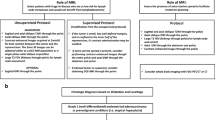
Colorectal cancer (CRC) is the most common gastrointestinal neoplasm. Imaging plays a key role in the primary diagnosis, risk stratification and prognosis, therapy planning, treatment response assessment, follow-up, and, to some extent, also in prevention of CRC. The most used imaging modalities for the evaluation of these tumours are computed tomography (CT) and magnetic resonance imaging (MRI). We review the literature and, drawed on our own experience, evaluate recent innovations in hardware, software (including artificial intelligence), and analytic tools that are opening new possibilities to CT and MRI imaging in CRC. Finally, we examine the advantages and disadvantages of these techniques.
Recent Findings
Advances in CT technology have improved image quality and reduced radiation exposure to patients and have allowed a paradigm shift from an imaging modality that provided solely anatomical data to one that can also provide functional information. In addition, technological improvements in MRI have made possible a faster and more robust imaging technique and the generation of new data of tumour phenotype. All these advances have expanded the clinical capabilities of these techniques in colorectal tumours.
Summary
Recent developments and emerging technologies in CT and MRI are changing the management of CRC patients in many clinical scenarios. Current evidence supports the clinical application of many of them. In other cases, such as quantitative imaging, multiparametric assessment, and radiomics/radiogenomics, important problems of standardization and reproducibility of these techniques persist that limit their introduction in daily clinical practice.












Similar content being viewed by others
Availability of Data and Material
Data transparency is guaranteed.
We declare that all authors whose names appear on the submission (1) made substantial contributions to the conception or design of the work, or the acquisition, analysis, or interpretation of data in the work; (2) drafted the work or revised it critically for important intellectual content; (3) approved the submitted version; and (4) agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49. https://doi.org/10.3322/caac.21660.
López-Campos F, Martín-Martín M, Fornell-Pérez R, García-Pérez JC, Die-Trill J, Fuentes-Mateos R, et al. Watch and wait approach in rectal cancer: current controversies and future directions. World J Gastroenterol. 2020;26:4218–39. https://doi.org/10.3748/wjg.v26.i29.4218.
Santiago I, Rodrigues B, Barata M, Figueiredo N, Fernandez L, Galzerano A, et al. Re-staging and follow-up of rectal cancer patients with MR imaging when “Watch-and-Wait” is an option: a practical guide. Insights Imaging. 2021;12:114. https://doi.org/10.1186/s13244-021-01055-w.
Kasi A, Abbasi S, Handa S, Al-Rajabi R, Saeed A, Baranda J, et al. Total neoadjuvant therapy vs standard therapy in locally advanced rectal cancer: a systematic review and meta-analysis. JAMA Netw Open. 2020;3(12): e2030097. https://doi.org/10.1001/jamanetworkopen.2020.30097.
Bhoday J, Balyasnikova S, Wale A, Brown G. How should imaging direct/orient management of rectal cancer? Clin Colon Rectal Surg. 2017;30:297–312. https://doi.org/10.1055/s-0037-1606107.
Santiago I, Figueiredo N, Parés O, Matos C. MRI of rectal cancer-relevant anatomy and staging key points. Insights Imaging. 2020;11:100. https://doi.org/10.1186/s13244-020-00890-7.
• Krdzalic J, Maas M, Gollub MJ, Beets-Tan RGH. Guidelines for MR imaging in rectal cancer: Europe versus United States. Abdom Radiol (NY). 2019;44:3498–507. doi: https://doi.org/10.1007/s00261-019-02251-5. An important paper comparing American and European guidelines and protocols for rectal MRI, which improve imaging quality and reporting standardization.
Nerad E, Lambregts DM, Kersten EL, Maas M, Bakers FC, van den Bosch HC, et al. MRI for local staging of colon cancer: can MRI become the optimal staging modality for patients with colon cancer? Dis Colon Rectum. 2017;60:385–92. https://doi.org/10.1097/DCR.0000000000000794.
Laghi A. CT colonography: an update on current and future indications. Expert Rev Gastroenterol Hepatol. 2016;10:785–94. https://doi.org/10.1586/17474124.2016.1143358.
Mainenti PP, Stanzione A, Guarino S, Romeo V, Ugga L, Romano F, et al. Colorectal cancer: parametric evaluation of morphological, functional and molecular tomographic imaging. World J Gastroenterol. 2019;25:5233–56. https://doi.org/10.3748/wjg.v25.i35.5233.
•• García-Figueiras R, Baleato-González S, Padhani AR, Luna-Alcalá A, Marhuenda A, Vilanova JC, et al. Advanced imaging techniques in evaluation of colorectal cancer. Radiographics. 2018;38:740–65. doi: https://doi.org/10.1148/rg.2018170044. This paper represents the most detailed and up-to-date review of the role of advanced imaging techniques in colorectal tumours.
Hsieh J, Flohr T. Computed tomography recent history and future perspectives. J Med Imaging (Bellingham). 2021;8: 052109. https://doi.org/10.1117/1.JMI.8.5.052109.
Willemink MJ, Noël PB. The evolution of image reconstruction for CT-from filtered back projection to artificial intelligence. Eur Radiol. 2019;29:2185–95. https://doi.org/10.1007/s00330-018-5810-7.
Zhang Q, Eagleson R, Peters TM. Volume visualization: a technical overview with a focus on medical applications. J Digit Imaging. 2011;24:640–4. https://doi.org/10.1007/s10278-010-9321-6.
Planz VB, Lubner MG, Pickhardt PJ. Volumetric analysis at abdominal CT: oncologic and non-oncologic applications. Br J Radiol. 2019;92:20180631. https://doi.org/10.1259/bjr.20180631.
Dappa E, Higashigaito K, Fornaro J, Leschka S, Wildermuth S, Alkadhi H. Cinematic rendering - an alternative to volume rendering for 3D computed tomography imaging. Insights Imaging. 2016;7:849–56. https://doi.org/10.1007/s13244-016-0518-1.
• Spada C, Hassan C, Bellini D, Burling D, Cappello G, Carretero C, et al. Imaging alternatives to colonoscopy: CT colonography and colon capsule. European Society of Gastrointestinal Endoscopy (ESGE) and European Society of Gastrointestinal and Abdominal Radiology (ESGAR) Guideline - Update 2020. Eur Radiol. 2021;31:2967–82. doi: https://doi.org/10.1007/s00330-020-07413-4. A consensus that establish clinical scenarios for the use of alternative techniques to optical colonoscopy.
Yee J, Chang KJ, Dachman AH, Kim DH, McFarland EG, Pickhardt PJ, et al. The added value of the CT colonography reporting and data system. J Am Coll Radiol. 2016;13:931–5. https://doi.org/10.1016/j.jacr.2016.04.031.
Bates DDB, Paroder V, Lall C, Lalwani N, Widmar M, Garcia-Aguilar J. Complete mesocolic excision and central vascular ligation for right colon cancer: an introduction for abdominal radiologists. Abdom Radiol (NY). 2019;44:3518–26. https://doi.org/10.1007/s00261-019-02037-9.
Nepal P, Mori S, Kita Y, Tanabe K, Baba K, Sasaki K, et al. Anatomical study of the inferior mesenteric vein using three-dimensional computed tomography angiography in laparoscopy-assisted surgery for left-sided colorectal cancer. Surg Today. 2021. https://doi.org/10.1007/s00595-021-02292-8. Online ahead of print.
Park JY, Kim SH, Lee SM, Lee JS, Han JK. CT volumetric measurement of colorectal cancer helps predict tumor staging and prognosis. PLoS One. 2017;12:e0178522. https://doi.org/10.1371/journal.pone.0178522. eCollection 2017.
Lim MC, Tan CH, Cai J, Zheng J, Kow AW. CT volumetry of the liver: where does it stand in clinical practice? Clin Radiol. 2014;69:887–95. https://doi.org/10.1016/j.crad.2013.12.021.
Zimmermann M, Kuhl CK, Engelke H, Bettermann G, Keil S. CT-based whole-body tumor volumetry versus RECIST 1.1: feasibility and implications for inter-reader variability. Eur J Radiol. 2021;135:109514. https://doi.org/10.1016/j.ejrad.2020.109514.
Rothe JH, Grieser C, Lehmkuhl L, Schnapauff D, Fernandez CP, Maurer MH, et al. Size determination and response assessment of liver metastases with computed tomography–comparison of RECIST and volumetric algorithms. Eur J Radiol. 2013;82:1831–9. https://doi.org/10.1016/j.ejrad.2012.05.018.
• Winter KS, Hofmann FO, Thierfelder KM, Holch JW, Hesse N, Baumann AB, et al. Towards volumetric thresholds in RECIST 1.1: therapeutic response assessment in hepatic metastases. Eur Radiol. 2018;28:4839–48. doi: https://doi.org/10.1007/s00330-018-5424-0. A study that demonstrates the possibility of using volumetric measurements instead of the classic value of the largest diameter of the lesions (RECIST) in the assessment of response of colorectal cancer. Volumetric measurements represent more accurately tumour burden.
Rowe SP, Chu LC, Fishman EK. Computed tomography cinematic rendering in the evaluation of colonic pathology: technique and clinical applications. J Comput Assist Tomogr. 2019;43:475–84. https://doi.org/10.1097/RCT.0000000000000864.
Srinivasan S. Dual-energy CT in colorectal cancers: beyond the density measurements. Diagn Interv Radiol. 2017;23:479–80. https://doi.org/10.5152/dir.2017.17287.
Sun K, Han R, Han Y, Shi X, Hu J, Lu B. Accuracy of combined computed tomography colonography and dual energy iiodine map imaging for detecting colorectal masses using high-pitch dual-source CT. Sci Rep. 2018;8:3790. https://doi.org/10.1038/s41598-018-22188-x.
Al-Najami I, Mahmoud Sheta H, Baatrup G. Differentiation between malignant and benign rectal tumors by dual-energy computed tomography - a feasibility study. Acta Oncol. 2019;58(sup1):S55–9. https://doi.org/10.1080/0284186X.2019.1574404.
Chuang-Bo Y, Tai-Ping H, Hai-Feng D, et al. Quantitative assessment of the degree of differentiation in colon cancer with dual-energy spectral CT. Abdom Radiol (NY). 2017;42:2591–6. https://doi.org/10.1007/s00261-017-1176-6.41.
Gong HX, Zhang KB, Wu LM, et al. Dual energy spectral CT imaging for colorectal cancer grading: a preliminary study. PLoS ONE. 2016;11: e0147756. https://doi.org/10.1371/journal.pone.0147756.
Wu J, Lv Y, Wang N, et al. The value of single-source dual-energy CT imaging for discriminating microsatellite instability from microsatellite stability human colorectal cancer. Eur Radiol. 2019;29:3782–90. https://doi.org/10.1007/s00330-019-06144-5.
Cao Y, Zhang G, Bao H, Zhang S, Zhang J, Zhao Z, et al. Development of a dual-energy spectral CT based nomogram for the preoperative discrimination of mutated and wild-type KRAS in patients with colorectal cancer. Clin Imaging. 2021;69:205–12. https://doi.org/10.1016/j.clinimag.2020.08.023.
Fan S, Li X, Zheng L, Hu D, Ren X, Ye Z. Correlations between the iodine concentrations from dual energy computed tomography and molecular markers Ki-67 and HIF-1α in rectal cancer: a preliminary study. Eur J Radiol. 2017;96:109–14. https://doi.org/10.1016/j.ejrad.2017.08.026.
Kang HJ, Kim SH, Bae JS, Jeon SK, Han JK. Can quantitative iodine parameters on DECT replace perfusion CT parameters in colorectal cancers? Eur Radiol. 2018;28:4775–82. https://doi.org/10.1007/s00330-018-5502-3.
Kato T, Uehara K, Ishigaki S, Nihashi T, Arimoto A, Nakamura H, et al. Clinical significance of dual-energy CT-derived iodine quantification in the diagnosis of metastatic LN in colorectal cancer. Eur J Surg Oncol. 2015;41:1464–70.
Yang Z, Zhang X, Fang M, Li G, Duan X, Mao J, et al. Preoperative diagnosis of regional lymph node metastasis of colorectal cancer with quantitative parameters from dual-energy CT. AJR Am J Roentgenol. 2019;213:W17-25. https://doi.org/10.2214/AJR.18.20843.
Liu H, Yan F, Pan Z, et al. Evaluation of dual energy spectral CT in differentiating metastatic from non-metastatic lymph nodes in rectal cancer: initial experience. Eur J Radiol. 2015;84:228–34.
Al-Najami I, Drue HC, Steele R, Baatrup G. DECT - a possible new method to assess regression of rectal cancers after neoadjuvant treatment. J Surg Oncol. 2017;116:984–8.
Sauter AP, Kössinger A, Beck S, Deniffel D, Dapper H, Combs SE, et al. Dual-energy CT parameters in correlation to MRI-based apparent diffusion coefficient: evaluation in rectal cancer after radiochemotherapy. Acta Radiol Open. 2020;9:2058460120945316. https://doi.org/10.1177/2058460120945316.
García-Figueiras R, Goh VJ, Padhani AR, Baleato-González S, Garrido M, León L, et al. CT perfusion in oncologic imaging: a useful tool? AJR Am J Roentgenol. 2013;200:8–19. https://doi.org/10.2214/AJR.11.8476.
Goh V, Glynne-Jones R. Perfusion CT imaging of colorectal cancer. Br J Radiol. 2014;87:20130811. https://doi.org/10.1259/bjr.20130811.
Muenzel D, Bar-Ness D, Roessl E, Blevis I, Bartels M, Fingerle AA, et al. Spectral photon-counting CT: initial experience with dual-contrast agent K-edge colonography. Radiology. 2017;283:723–8. https://doi.org/10.1148/radiol.2016160890.
• Thivolet A, Si-Mohamed S, Bonnot PE, Blanchet C, Képénékian V, Boussel L, et al. Spectral photon-counting CT imaging of colorectal peritoneal metastases: initial experience in rats. Sci Rep. 2020;10:13394. doi: https://doi.org/10.1038/s41598-020-70282-w. A preliminary study in animal models that shows the ability of photon-counting CT to use and assess multiple contrast media at the same time imaging colorectal tumours. This advanced technique under research may revolutionize CT imaging.
• Gollub MJ, Lall C, Lalwani N, Rosenthal MH. Current controversy, confusion, and imprecision in the use and interpretation of rectal MRI. Abdom Radiol (NY). 2019;44:3549–58. doi: https://doi.org/10.1007/s00261-019-01996-3. A paper that clarifies key points that need to be considered when reporting MR exams of rectal cancer, including confusing nomenclature, prognostic features, and anatomical landmarks.
Yoon JH, Nickel MD, Peeters JM, Lee JM. Rapid imaging: recent advances in abdominal MRI for reducing acquisition time and its clinical applications. Korean J Radiol. 2019;20:1597–615. https://doi.org/10.3348/kjr.2018.0931.
Chan WY, Hartono S, Thng CH, Koh DM. New advances in magnetic resonance techniques in abdomen and pelvis. Magn Reson Imaging Clin N Am. 2020;28:433–45. https://doi.org/10.1016/j.mric.2020.04.001.
Ream JM, Rosenkrantz AB. Advances in T1-weighted and T2-weighted imaging in the abdomen and pelvis. Radiol Clin North Am. 2015;53:583–98. https://doi.org/10.1016/j.rcl.2015.01.003.
Feng L, Benkert T, Block KT, Sodickson DK, Otazo R, Chandarana H. Compressed sensing for body MRI. J Magn Reson Imaging. 2017;45:966–87. https://doi.org/10.1002/jmri.25547.
Park JH, Seo N, Lim JS, Hahm J, Kim MJ. Feasibility of simultaneous multislice acceleration technique in diffusion-weighted magnetic resonance imaging of the rectum. Korean J Radiol. 2020;21:77–87. https://doi.org/10.3348/kjr.2019.0406.
Haak HE, Maas M, Trebeschi S, Beets-Tan RGH. Modern MR imaging technology in rectal cancer; there is more than meets the eye. Front Oncol. 2020;10:537532. https://doi.org/10.3389/fonc.2020.537532. eCollection 2020.
Canellas R, Rosenkrantz AB, Taouli B, Sala E, Saini S, Pedrosa I, et al. Abbreviated MRI protocols for the abdomen. Radiographics. 2019;39:744–58. https://doi.org/10.1148/rg.2019180123.
Lee SL, Shin YR, Kim K. The added value of pelvic surveillance by MRI during postoperative follow-up of rectal cancer, with a focus on abbreviated MRI. Eur Radiol. 2020;30:3113–24. https://doi.org/10.1007/s00330-020-06711-1 (Epub 2020 Feb 18).
Granata V, Fusco R, Avallone A, Cassata A, Palaia R, Delrio P, et al. Abbreviated MRI protocol for colorectal liver metastases: how the radiologist could work in pre surgical setting. PLoS One. 2020;15:e0241431. https://doi.org/10.1371/journal.pone.0241431. eCollection 2020.
Lim KK, Noe G, Hornsey E, Lim RP. Clinical applications of 3D T2-weighted MRI in pelvic imaging. Abdom Imaging. 2014;39:1052–62. https://doi.org/10.1007/s00261-014-0124-y.
Kim H, Lim JS, Choi JY, Park J, Chung YE, Kim MJ, et al. Rectal cancer: comparison of accuracy of local-regional staging with two- and three-dimensional preoperative 3-T MR imaging. Radiology. 2010;254:485–92. https://doi.org/10.1148/radiol.09090587.
Cao W, Lian Y, Liu D, Li F, Zhu P, Zhou Z. Rectal cancer restaging using 3D CUBE vs. 2D T2- weighted technique after neoadjuvant therapy: a diagnostic study. Gastroenterol Rep (Oxf). 2017;5:226–31. https://doi.org/10.1093/gastro/gow039.
Gormly K. Rectal MRI: the importance of high resolution T2 technique. Abdom Radiol (NY). 2021;46(9):4090–5. https://doi.org/10.1007/s00261-021-03047-2.
Fütterer JJ, Yakar D, Strijk SP, Barentsz JO. Preoperative 3 T MR imaging of rectal cancer: local staging accuracy using a two-dimensional and three- dimensional T2-weighted turbo spin echo sequence. Eur J Radiol. 2008;65:66–71. https://doi.org/10.1016/j.ejrad.2007.11.029.
Zhao L, Liang M, Shi Z, Xie L, Zhang H, Zhao X. Preoperative volumetric synthetic magnetic resonance imaging of the primary tumor for a more accurate prediction of lymph node metastasis in rectal cancer. Quant Imaging Med Surg. 2021;11:1805–16. https://doi.org/10.21037/qims-20-659.
Zhao L, Liang M, Xie L, Yang Y, Zhang H, Zhao X. Prediction of pathological prognostic factors of rectal cancer by relaxation maps from synthetic magnetic resonance imaging. Eur J Radiol. 2021 May;138: 109658. https://doi.org/10.1016/j.ejrad.2021.109658.
Ge YX, Hu SD, Wang Z, Guan RP, Zhou XY, Gao QZ, et al. Feasibility and reproducibility of T2 mapping and DWI for identifying malignant lymph nodes in rectal cancer. Eur Radiol. 2021;31:3347–54. https://doi.org/10.1007/s00330-020-07359-7.
Chen Y, Jiang Y, Pahwa S, Ma D, Lu L, Twieg MD, et al. MR fingerprinting for rapid quantitative abdominal imaging. Radiology. 2016;279:278–86. https://doi.org/10.1148/radiol.2016152037.
Zhao L, Liang M, Wu PY, Yang Y, Zhang H, Zhao X. A preliminary study of synthetic magnetic resonance imaging in rectal cancer: imaging quality and preoperative assessment. Insights Imaging. 2021;12(1):120. https://doi.org/10.1186/s13244-021-01063-w.
Zhao L, Liang M, Xie L, Yang Y, Zhang H, Zhao X. Prediction of pathological prognostic factors of rectal cancer by relaxation maps from synthetic magnetic resonance imaging. Eur J Radiol. 2021;138: 109658. https://doi.org/10.1016/j.ejrad.2021.109658.
Tang L, Zhou XJ. Diffusion MRI of cancer: from low to high b-values. J Magn Reson Imaging. 2019;49:23–40. https://doi.org/10.1002/jmri.26293.
Prezzi D, Goh V. Rectal cancer magnetic resonance imaging: imaging beyond morphology. Clin Oncol (R Coll Radiol). 2016;28:83–92. https://doi.org/10.1016/j.clon.2015.10.010.
Gürses B, Böge M, Altınmakas E, Balık E. Multiparametric MRI in rectal cancer. Diagn Interv Radiol. 2019;25:175–82. https://doi.org/10.5152/dir.2019.18189.
•• Pham TT, Liney GP, Wong K, Barton MB. Functional MRI for quantitative treatment response prediction in locally advanced rectal cancer. Br J Radiol. 2017;90:20151078. doi: https://doi.org/10.1259/bjr.20151078. This paper highlights the promising role of DWI and DCE-MRI and multiparametric imaging in the assessment of pathological response in rectal cancer, but also remarks that these techniques currently lack sufficient accuracy and standardization to be routinely used to change clinical patient management.
Schurink NW, Lambregts DMJ, Beets-Tan RGH. Diffusion-weighted imaging in rectal cancer: current applications and future perspectives. Br J Radiol. 2019;92:20180655. https://doi.org/10.1259/bjr.20180655. An excellent paper that covers all the clinical applications of diffusion-weighted imaging in rectal cancer with a complete review of the published literature.
Nguyen TL, Soyer P, Fornès P, Rousset P, Kianmanesh R, Hoeffel C. Diffusion-weighted MR imaging of the rectum: clinical applications. Crit Rev Oncol Hematol. 2014;92:279–95. https://doi.org/10.1016/j.critrevonc.2014.07.002.
Jia H, Ma X, Zhao Y, Zhao J, Liu R, Chen Z, et al. Meta-analysis of diffusion-weighted magnetic resonance imaging in identification of colorectal cancer. Int J Clin Exp Med. 2015;8:17333–42. eCollection 2015.
Lambregts DMJ, Boellaard TN, Beets-Tan RGH. Response evaluation after neoadjuvant treatment for rectal cancer using modern MR imaging: a pictorial review. Insights Imaging. 2019;10:15. https://doi.org/10.1186/s13244-019-0706-x.
van der Paardt MP, Zagers MB, Beets-Tan RG, Stoker J, Bipat S. Patients who undergo preoperative chemoradiotherapy for locally advanced rectal cancer restaged by using diagnostic MR imaging: a systematic review and meta-analysis. Radiology. 2013;269:101–12. https://doi.org/10.1148/radiol.13122833.
Taylor SA, Mallett S, Beare S, Bhatnagar G, Blunt D, Boavida P, et al; Streamline investigators. Diagnostic accuracy of whole-body MRI versus standard imaging pathways for metastatic disease in newly diagnosed colorectal cancer: the prospective Streamline C trial. Lancet Gastroenterol Hepatol. 2019;4:529–37. https://doi.org/10.1016/S2468-1253(19)30056-1.
Le Bihan D. What can we see with IVIM MRI? Neuroimage. 2019;187:56–67. https://doi.org/10.1016/j.neuroimage.2017.12.062.
Surov A, Meyer HJ, Höhn AK, Behrmann C, Wienke A, Spielmann RP, et al. Correlations between intravoxel incoherent motion (IVIM) parameters and histological findings in rectal cancer: preliminary results. Oncotarget. 2017;8:21974–83. https://doi.org/10.18632/oncotarget.15753.
Granata V, Fusco R, Reginelli A, Delrio P, Selvaggi F, Grassi R, et al. Diffusion kurtosis imaging in patients with locally advanced rectal cancer: current status and future perspectives. J Int Med Res. 2019;47:2351–60. https://doi.org/10.1177/0300060519827168.
Dijkhoff RAP, Beets-Tan RGH, Lambregts DMJ, Beets GL, Maas M. Value of DCE-MRI for staging and response evaluation in rectal cancer: a systematic review. Eur J Radiol. 2017;95:155–68. https://doi.org/10.1016/j.ejrad.2017.08.009.
Lord A, D’Souza N, Shaw A, Day N, Brown G. The current status of nodal staging in rectal cancer. Curr Colorectal Cancer Rep. 2019;15:143–8. https://doi.org/10.1007/s11888-019-00441-3.
Elsholtz FHJ, Asbach P, Haas M, Becker M, Beets-Tan RGH, Thoeny HC, et al. Introducing the Node Reporting and Data System 1.0 (Node-RADS): a concept for standardized assessment of lymph nodes in cancer. Eur Radiol. 2021. https://doi.org/10.1007/s00330-020-07572-4. Online ahead of print.
Hong EK, Landolfi F, Castagnoli F, Park SJ, Boot J, Van den Berg J, et al. CT for lymph node staging of colon cancer: not only size but also location and number of lymph node count. Abdom Radiol (NY). 2021;46:4096–105. https://doi.org/10.1007/s00261-021-03057-0.
• Stijns RCH, Philips BWJ, Nagtegaal ID, Polat F, de Wilt JHW, Wauters CAP, et al. USPIO-enhanced MRI of lymph nodes in rectal cancer: a node-to-node comparison with histopathology. Eur J Radiol. 2021;138:109636. https://doi.org/10.1016/j.ejrad.2021.109636. An important study that shows the limitations of imaging in the characterization of LNs in rectal cancer. Despite the hopes placed on the USPIO, a lymphotrophic contrast-agent, this study demonstrates that USPIO-enhanced MRI is not accurate for characterizing small benign versus small tumoural lymph nodes in rectal cancer patients.
Khwaja SA, Thipphavong S, Kirsch R, Menezes RJ, Kennedy ED, Brierley JD, et al. Evaluation of a multiparametric MRI scoring system for histopathologic treatment response following preoperative chemoradiotherapy for rectal cancer. Eur J Radiol. 2021;138: 109628. https://doi.org/10.1016/j.ejrad.2021.109628.
Yakar M, Etiz D. Artificial intelligence in rectal cancer. Artif Intell Gastroenterol. 2021;2:10–26. https://doi.org/10.35712/aig.v2.i2.10.
•• Horvat N, Bates DDB, Petkovska I. Novel imaging techniques of rectal cancer: what do radiomics and radiogenomics have to offer? A literature review. Abdom Radiol (NY). 2019;44:3764–74. https://doi.org/10.1007/s00261-019-02042-y. A detailed review of radiomics/radiogenomics in rectal cancer, including basic concepts, benefits, pitfalls, and limitations, is discussed. The complex work-flow of radiomics/radiogenomics generation and the difficult biological correlation of their parameters obtained account for the low implementation in clinical practice.
Staal FCR, van der Reijd DJ, Taghavi M, Lambregts DMJ, Beets-Tan RGH, Maas M. Radiomics for the prediction of treatment outcome and survival in patients with colorectal cancer: a systematic review. Clin Colorectal Cancer. 2021;20:52–71. https://doi.org/10.1016/j.clcc.2020.11.001.
Coppola F, Giannini V, Gabelloni M, Panic J, Defeudis A, Lo Monaco S, et al. Radiomics and magnetic resonance imaging of rectal cancer: from engineering to clinical practice. Diagnostics (Basel). 2021;11:756. https://doi.org/10.3390/diagnostics11050756.
Badic B, Tixier F, Cheze Le Rest C, Hatt M, Visvikis D. Radiogenomics in colorectal cancer. Cancers (Basel). 2021;13:973. https://doi.org/10.3390/cancers13050973.
Otazo R, Lambin P, Pignol JP, Ladd ME, Schlemmer HP, Baumann M, et al. MRI-guided radiation therapy: an emerging paradigm in adaptive radiation oncology. Radiology. 2021;298:248–60. https://doi.org/10.1148/radiol.2020202747.
Keller DS, Berho M, Perez RO, Wexner SD, Chand M. The multidisciplinary management of rectal cancer. Nat Rev Gastroenterol Hepatol. 2020;17:414–29. https://doi.org/10.1038/s41575-020-0275-y
Bird D, Nix MG, McCallum H, Teo M, Gilbert A, Casanova N, et al. Multicentre, deep learning, synthetic-CT generation for ano-rectal MR-only radiotherapy treatment planning. Radiother Oncol. 2021 Mar;156:23–8. https://doi.org/10.1016/j.radonc.2020.11.027.
Kontovounisios C, Tekkis P, Bello F. 3D imaging and printing in pelvic colorectal cancer: ‘The New Kid on the Block.’ Tech Coloproctol. 2019;23:171–3. https://doi.org/10.1007/s10151-018-1922-y.
Emile SH, Wexner SD. Systematic review of the applications of three-dimensional printing in colorectal surgery. Colorectal Dis. 2019;21:261–9. https://doi.org/10.1111/codi.14480.
Papazarkadas X, Spartalis E, Patsouras D, Ioannidis A, Schizas D, Georgiou K, et al. The role of 3D printing in colorectal surgery: current evidence and future perspectives. In Vivo. 2019;33:297–302. https://doi.org/10.21873/invivo.11475.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Diagnostic and Interventional Radiology Innovations in Colorectal Cancer
Rights and permissions
About this article
Cite this article
García-Figueiras, R., Baleato-González, S., Canedo-Antelo, M. et al. Imaging Advances on CT and MRI in Colorectal Cancer. Curr Colorectal Cancer Rep 17, 113–130 (2021). https://doi.org/10.1007/s11888-021-00468-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11888-021-00468-5