Abstract
Purpose of Review
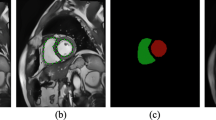
Myocardial fibrosis (MF) arises due to myocardial infarction and numerous cardiac diseases. MF may lead to several heart disorders, such as heart failure, arrhythmias, and ischemia. Cardiac magnetic resonance (CMR) imaging techniques, such as late gadolinium enhancement (LGE) CMR, enable non-invasive assessment of MF in the left ventricle (LV). Manual assessment of MF on CMR is a tedious and time-consuming task that is subject to high observer variability. Automated segmentation and quantification of MF is important for risk stratification and treatment planning in patients with heart disorders. This article aims to review the machine learning (ML)-based methodologies developed for MF quantification in the LV using CMR images.
Recent Findings
With the availability of relatively large labeled datasets supervised learning methods based on both conventional ML and state-of-the-art deep learning (DL) methods have been successfully applied for automated segmentation of MF. The incorporation of ML algorithms into imaging techniques such as 3D LGE CMR permits fast characterization of MF on CMR imaging and may enhance the diagnosis and prognosis of patients with heart disorders. Concurrently, the studies using cine CMR images have revealed that accurate segmentation of MF on non-contrast CMR imaging might be possible.
Summary
The application of ML/DL tools in CMR image interpretation is likely to result in accurate and efficient quantification of MF.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Murtha LA, Schuliga MJ, Mabotuwana NS, Hardy SA, Waters DW, Burgess JK, et al. The processes and mechanisms of cardiac and pulmonary fibrosis. Front Physiol. 2017;8:1664–042X. https://doi.org/10.3389/fphys.2017.00777.
Weber KT, Sun Y, Bhattacharya SK, Ahokas RA, Gerling IC. Myofibroblast-mediated mechanisms of pathological remodelling of the heart. Nat Rev Cardiol. 2013;10:15–26. https://doi.org/10.1038/nrcardio.2012.158.
Zeisberg M, Kalluri R. Cellular mechanisms of tissue fibrosis. Common and organ-specific mechanisms associated with tissue fibrosis. Am J Physiol Cell Physiol. 2013;304:C216–25. https://doi.org/10.1152/ajpcell.00328.2012.
Jellis C, Martin J, Narula J, Marwick TH. Assessment of nonischemic myocardial fibrosis. J Am Coll Cardiol. 2010;56:89–97. https://doi.org/10.1016/j.jacc.2010.02.047.
Disertori M, Masè M, Ravelli F. Myocardial fibrosis predicts ventricular tachyarrhythmias. Trends Cardiovasc Med. 2017;27:363–72.
Espeland T, Lunde IG, Amundsen BH, Gullestad L, Aakhus S. Myocardial fibrosis. Tidsskr Nor Laegeforen. 2018;138. https://doi.org/10.4045/tidsskr.17.1027.
Piek A, de Boer RA, Silljé HH. The fibrosis-cell death axis in heart failure. Heart Fail Rev. 2016;21:199–211. https://doi.org/10.1007/s10741-016-9536-9.
Barison A, Grigoratos C, Todiere G, Aquaro GD. Myocardial interstitial remodelling in non-ischaemic dilated cardiomyopathy: insights from cardiovascular magnetic resonance. Heart Fail Rev. 2015;20:731–49. https://doi.org/10.1007/s10741-015-9509-4.
Herum KM, Lunde IG, McCulloch AD, Christensen G. The soft- and hard-heartedness of cardiac fibroblasts: mechanotransduction signaling pathways in fibrosis of the heart. J Clin Med. 2017;6:E53. https://doi.org/10.3390/jcm6050053.
Travers JG, Kamal FA, Robbins J, Yutzey KE, Blaxall BC. Cardiac fibrosis: the fibroblast awakens. Circ Res. 2016;118:1021–40. https://doi.org/10.1161/CIRCRESAHA.115.306565.
Kong P, Christia P, Frangogiannis NG. The pathogenesis of cardiac fibrosis. Cell Mol Life Sci. 2014;71:549–74. https://doi.org/10.1007/s00018-013-1349-6.
Tao Q, Sebastiaan RP, Hildo JL, Katja Z, Rob JG. Myocardial scar surface area identified by LGE MRI is an independent predictor of mortality in post-infarction patients. J Cardiovasc Magn Reson. 2015;17(Suppl 1):P46. https://doi.org/10.1186/1532-429X-17-S1-P46The findings of this study demonstrate that MF surface area identified from LGE CMRI is a predictor of all-course mortality in post-infarction patients, independent of left ventricle ejection fraction.
Lin A, Kwan C, Guppy-Coles K, Sippel J, Atherton J, Prasad S. Impact of infarct size on left ventricular diastolic function following acute myocardial infarction. Heart Lung Circ. 2015;132:A18996. https://doi.org/10.1016/j.hlc.2015.06.089.
Nguyen T, Phan J, Richards D, Moses D, Serratore M, Hogan J, et al. The impact of myocardial scar size and systolic function on diastolic dysfunction following acute st elevated myocardial infarction (STEMI) revascularisation. Heart Lung Circ. 2013;22:S200. https://doi.org/10.1016/j.hlc.2013.05.476.
Trayanova NT. Computational cardiology: the heart of the matter. ISRN Cardiol. 2012;2012:269680–15. https://doi.org/10.5402/2012/269680.
Ashikaga H, Arevalo H, Vadakkumpadan F, Blake RC, Bayer JD, Nazarian S, et al. Feasibility of image-based simulation to estimate ablation target in human ventricular arrhythmia. Heart Rhythm. 2013;10:1109–16. https://doi.org/10.1016/j.hrthm.2013.04.015.
Winslow RL, Trayanova N, Geman D, Miller MI. Computational medicine: Translating models to clinical care. Sci Transl Med. 2012;4:158rv11. https://doi.org/10.1126/scitranslmed.3003528.
Vigmond E, Vadakkumpadan F, Gurev V, Arevalo H, Deo M, Plank G, et al. Towards predictive modelling of the electrophysiology of the heart. Exp Physiol. 2009;94:563–77. https://doi.org/10.1113/expphysiol.2008.044073.
Vadakkumpadan F, Gurev V, Constantino J, Arevalo H, Trayanova N. Modeling of whole-heart electrophysiology and mechanics: toward patient-specific simulations. Modeling of whole-heart electrophysiology and mechanics: toward patient-specific simulations. In: Kerckhoffs R, editor. Patient-specific modeling of the cardiovascular system. New York: Springer; 2010.
Vadakkumpadan F, Arevalo H, Jebb A, Wu KC, Trayanova N. Image-based patient-specific simulations of ventricular electrophysiology for sudden arrhythmic death risk stratification. Circulation. 2013;128:A18014. https://doi.org/10.1161/CIRCEP.117.004743.
Ukwatta E, Nikolov P, Zabihollahy F, Trayanova NA, Wright GA. Virtual electrophysiological study as a tool for evaluating efficacy of MRI techniques in predicting adverse arrhythmic events in ischemic patients. Phys Med Biol. 2018;63:225008. https://doi.org/10.1088/1361-6560/aae8b2.
Trayanova N, Boyle PM, Arevalo HJ, Zahid S. Exploring susceptibility to atrial and ventricular arrhythmias resulting from remodeling of the passive electrical properties in the heart: a simulation approach. Front Physiol. 2014;5:435. https://doi.org/10.3389/fphys.2014.00435.
Ukwatta E, Arevalo H, Rajchl M, White JA, Pashakhanloo F, Prakosa A, et al. Image-based reconstruction of three-dimensional myocardial infarct geometry for patient-specific modeling of cardiac electrophysiology. Med Phys. 2015;42:4579–90. https://doi.org/10.1118/1.4926428.
Schmidt A, Azevedo CF, Cheng A, Gupta SN, Bluemke DA, Foo TK, et al. Infarct tissue heterogeneity by magnetic resonance imaging identifies enhanced cardiac arrhythmia susceptibility in patients with left ventricular dysfunction. Circulation. 2007;115:2006–14. https://doi.org/10.1161/CIRCULATIONAHA.106.653568.
Bello D, Fieno DS, Kim RJ, Pereles FS, Passman R, Song G, et al. Infarct morphology identifies patients with substrate for sustained ventricular tachycardia. J Am Coll Cardiol. 2005;45:1104–8. https://doi.org/10.1016/j.jacc.2004.12.057.
Kubicek J, Bryjova I, Penhaker M, Augustynek M. Extraction of myocardial fibrosis from MR using fuzzy soft thresholding algorithm. In: Proceedings - 2016 5th IIAI International Congress on Advanced Applied Informatics, IIAI-AAI 2016. 2016. https://doi.org/10.1109/IIAI-AAI.2016.143.
Rajiah P, Desai MY, Kwon D, Flamm SD. MR imaging of myocardial infarction. Radiographics. 2013;33:1383–413. https://doi.org/10.1148/rg.335125722.
Mewton N, Chia Ying L, Croisille P, Bluemke D, João ACL. Assessment of myocardial fibrosis with cardiovascular magnetic resonance. J Am Coll Cardiol. 2011;57(8):891–903. https://doi.org/10.1016/j.jacc.2010.11.013.
Flett AS, Hayward MP, Ashworth MT, Hansen MS, Taylor AM, Elliott PM, et al. Equilibrium contrast cardiovascular magnetic resonance for the measurement of diffuse myocardial fibrosis: preliminary validation in humans. Circulation. 2010;122(2):138–44. https://doi.org/10.1161/CIRCULATIONAHA.109.930636 ISSN 0009-7322.
Pfeiffer MP, Biederman RW. Cardiac MRI: a general overview with emphasis on current use and indication. Med Clin North Am. 2015;99:849–61. https://doi.org/10.1016/j.mcna.2015.02.011.
Kim RJ, Fieno DS, Parrish TB, Harris K, Chen EL, Simonetti O, et al. Relationship of MRI delayed contrast enhancement to irreversible injury, infarct age, and contractile function. Circulation. 1999;100(19):1992–2002. https://doi.org/10.1161/01.CIR.100.19.1992Circulation.
Ibrahim T, Makowski MR, Jankauskas A, Maintz D, Karch M, Schachoff S, et al. Serial contrast-enhanced cardiac magnetic resonance imaging demonstrates regression of hyperenhancement within the coronary artery wall in patients after acute myocardial infarction. JACC Cardiovasc Imaging. 2009;2:580–8. https://doi.org/10.1016/j.jcmg.2008.12.029.
Farrag NA, Ramanan V, Wright GA, Ukwatta E. Effect of T1-mapping technique and diminished image resolution on quantification of infarct mass and its ability in predicting appropriate ICD therapy. Med Phys. 2018;45:1577–85. https://doi.org/10.1002/mp.12840.
Amano Y, Yanagisawa F, Tachi M, Asai K, Suzuki Y, Hashimoto H, et al. Three-dimensional cardiac MR imaging: related techniques and clinical applications. Magn Reson Med Sci. 2017;16:183–9. https://doi.org/10.2463/mrms.rev.2016-0116.
Davis CP, Hany TF, Wildermuth S, Schmidt M, Debatin JF. Postprocessing techniques for gadolinium-enhanced three-dimensional MR angiography. Radiographics. 1997;17:1061–77. https://doi.org/10.1148/radiographics.17.5.9308101.
Heiss SG, Shifrin RY, Sommer FG. Contras-enhanced three-dimensional fast spoiled gradient-echo renal MR imaging: evaluation of vascular and nonvascular disease. Radiographics. 2000;20:1341–52. https://doi.org/10.1148/radiographics.20.5.g00se251341.
Bizino M, Tao Q, Amersfoort J, Van Der Geest RJ, Lamb HJ. 3D free-breathing late gadolinium enhancement 3T MRI: comparison with standard 2D Imaging. J Cardiovasc Magn Reson. 2014;16(Suppl 1):P198. https://doi.org/10.1186/1532-429X-16-S1-P198.
Viallon M, Jacquier A, Rotaru C, Delattre BMA, Mewton N, Vincent F, et al. Head-to-head comparison of eight late gadolinium-enhanced cardiac MR (LGE CMR) sequences at 1.5 tesla: from bench to bedside. J Magn Reson Imaging. 2011;34(6):1374–87. https://doi.org/10.1002/jmri.22783.
Morita K, Utsunomiya D, Oda S, Komi M, Namimoto T, Hirai T, et al. Comparison of 3D phase-sensitive inversion-recovery and 2D inversion-recovery MRI at 3.0 T for the assessment of late gadolinium enhancement in patients with hypertrophic cardiomyopathy. Acad Radiol. 2013;20(6):752–7. https://doi.org/10.1016/j.acra.2013.01.014.
Goetti R, Kozerke S, Donati OF, Sürder D, Stolzmann P, Kaufmann PA, et al. Acute, subacute, and chronic myocardial infarction: quantitative comparison of 2D and 3D late gadolinium enhancement MR imaging. Radiology. 2011;259(3):704–11. https://doi.org/10.1148/radiol.11102216.
Rajchl M, Yuan J, White JA, Ukwatta E, Stirrat J, Nambakhsh CMS, et al. Interactive hierarchical-flow segmentation of scar tissue from late-enhancement cardiac MR images. IEEE Trans Med Imaging. 2014;33(1):159–72. https://doi.org/10.1109/TMI.2013.2282932.
Xu C, Xu L, Gao Z, Zhao S, Zhang H, Zhang Y, et al. Direct delineation of myocardial infarction without contrast agents using a joint motion feature learning architecture. Med Image Anal. 2018;50:82–94. https://doi.org/10.1016/j.media.2018.09.001.
•• Xu C, Howey J, Ohorodnyk P, Roth M, Zhang H, Li S. Segmentation and quantification of infarction without contrast agents via spatiotemporal generative adversarial learning. Med Image Anal. 2020;59:101568. https://doi.org/10.1016/j.media.2019.101568The findings of this research show that LV MF characterization from non-contrast CMRI with high accuracy is possible.
Fox CS, Muntner P, Chen AY, Alexander KP, Roe MT, Cannon CP, et al. Use of evidence-based therapies in short-term outcomes of ST-segment elevation myocardial infarction and non–ST-segment elevation myocardial infarction in patients with chronic kidney disease: a report from the National Cardiovascular Data Acute Coronary Treatment and Intervention Outcomes Network Registry. Circulation. 2010;121(3):357–65. https://doi.org/10.1161/CIRCULATIONAHA.109.865352.
Rosendahl L, Blomstrand P, Heiberg E, Ohlsson J, Björklund PG, Ahlander BM, et al. Computer-assisted calculation of myocardial infarct size shortens the evaluation time of contrast-enhanced cardiac MRI. Clin Physiol Funct Imaging. 2008;28(1):1–7. https://doi.org/10.1111/j.1475-097X.2007.00765.x.
Neizel M, Katoh M, Schade E, Rassaf T, Krombach GA, Kelm M, et al. Rapid and accurate determination of relative infarct size in humans using contrast-enhanced magnetic resonance imaging. Clin Res Cardiol. 2009;98:319–24. https://doi.org/10.1007/s00392-009-0007-3.
Kolipaka A, Chatzimavroudis GP, White RD, O’Donnell TP, Setser RM. Segmentation of non-viable myocardium in delayed enhancement magnetic resonance images. Int J Cardiovasc Imaging. 2005;21:303–11. https://doi.org/10.1007/s10554-004-5806-z.
Ukwatta E, Arevalo H, Li K, Yuan J, Qiu W, Malamas P, et al. Myocardial infarct segmentation from magnetic resonance images for personalized modeling of cardiac electrophysiology. IEEE Trans Med Imaging. 2016;35:1408–19. https://doi.org/10.1109/TMI.2015.2512711.
Ukwatta E, Yuan J, Qiu W, Wu KC, Trayanova N, Vadakkumpadan F. Myocardial infarct segmentation and reconstruction from 2D late-gadolinium enhanced magnetic resonance image. Med Image Comput Comput Assist Interv. 2014;35:1408–19. https://doi.org/10.1109/TMI.2015.2512711.
Usta F, Gueaieb W, White JA, Ukwatta E. 3D scar segmentation from LGE-MRI using a continuous max-flow method. Houston: SPIE Medical Imaging; 2018. https://doi.org/10.1117/12.2294406.
Lu Y, Connelly KA, Yang Y, Joshi SB, Wright G, Radau PE. Semi-automated analysis of infarct heterogeneity on DE-MRI using graph cuts. J Cardiovasc Magn Reson. 2012;14:T6. https://doi.org/10.1186/1532-429X-14-S1-T6.
Zhu X, Vondrick C, Fowlkes CC, Ramanan D. Do we need more training data? Int J Comput Vis. 2016;119(17):76–92. https://doi.org/10.1007/s11263-015-0812-2.
LeCun Y, Bengio Y, Hinton G. Deep learning. Nature. 2015;521(7553):436–44.
Karim R, Bhagirath P, Claus P, James Housden R, Chen Z, Karimaghaloo Z, et al. Evaluation of state-of-the-art segmentation algorithms for left ventricle infarct from late Gadolinium enhancement MR images. Med Image Anal. 2016;30:95–107. https://doi.org/10.1016/j.media.2016.01.004.
Kurzendorfer T, Breininger K, Steidl S, Brost A, Forman C, Maier A. Myocardial scar segmentation in LGE-MRI using fractal analysis and random forest classification. 2018 24th International Conference on Pattern Recognition (ICPR), August 2018:3168–3173. https://doi.org/10.1109/ICPR.2018.8545636.
Moccia S, Banali R, Martini C, Muscogiuri G, Pontone G, Pepi M, et al. Development and testing of a deep learning-based strategy for scar segmentation on CMR-LGE images. Magn Reson Mater Physics, Biol Med. 2019;32(2):187(9). https://doi.org/10.1007/s10334-018-0718-4.
Zabihollahy F, White JA, Ukwatta E. Myocardial scar segmentation from magnetic resonance images using convolutional neural network. Proceedings Volume 10575, Medical Imaging 2018: Computer-aided diagnosis; 105752Z. https://doi.org/10.1117/12.2293518.
Zabihollahy F, White JA, Ukwatta E. Convolutional neural network-based approach for segmentation of left ventricle myocardial scar from 3D late gadolinium enhancement MR images. Med Phys. 2019;46(4):1740–51. https://doi.org/10.1002/mp.13436.
Lau F, Hendriks T, Lieman-Sifry J, Berk N, Sall S, Golden D, et al. ScarGAN: chained generative adversarial networks to simulate pathological tissue on cardiovascular MR scans. Deep Learn. Med. Image Anal. Multimodal Learn. Clin. Decis. Support, 2018:343–350. https://doi.org/10.1007/978-3-030-00889-5_39,.
Fahmy AS, Rausch J, Ulf N, Chan RH, Maron MS, Appelbaum E, et al. Automated cardiac MR scar quantification in hypertrophic cardiomyopathy using deep convolutional neural networks. JACC Cardiovasc Imaging. 2018;11(12):1917–8. https://doi.org/10.1016/j.jcmg.2018.04.030.
Zabihollahy F, Rajchl M, White JA, Ukwatta E. Fully automated segmentation of left ventricular scar from 3D late gadolinium enhancement magnetic resonance imaging using a cascaded multi-planar U-Net (CMPU-Net). Med Phys. 2020. https://doi.org/10.1002/mp.14022This document demonstrates the fully automated quantification of LV MF from 3D LGE CMRI with high accuracy is feasible.
Chen M, Fang L, Zhuang Q, Liu H. Deep learning assessment of myocardial infarction from MR image sequences. IEEE Access. 2019;7:5438–46. https://doi.org/10.1109/ACCESS.2018.2889744.
Xu C, Xu L, Gao Z, Zhao S, Zhang H, Zhang Y, et al. Direct detection of pixel-level myocardial infarction areas via a deep-learning algorithm. in Lecture Notes in Computer Science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics). 2017. arXiv:1706.03182v1.
Zhang N, Yang G, Gao Z, Xu C, Zhang Y, Shi R, et al. Deep learning for diagnosis of chronic myocardial infarction on nonenhanced cardiac cine MRI. Radiology. 2019;291(3):606–17. https://doi.org/10.1148/radiol.2019182304.
Xu C, Howey J, Ohorodnyk P, Roth M, Zhang H, Li S. Segmentation and quantification of infarction without contrast agents via spatiotemporal generative adversarial learning. Med Image Anal. 2020;291(3):606–17. https://doi.org/10.1148/radiol.2019182304.
Sun, Wong AKC, Kamel MS. Classification of imbalanced data: a review. Int J Pattern Recognit Artif Intell. 2009;23(04):687–719. https://doi.org/10.1142/S0218001409007326.
Acknowledgments
F. Zabihollahy acknowledges the Ontario Graduate Scholarship (OGS).
Funding
This work was supported by the Natural Sciences and Engineering Research Council of Canada (NSERC) Discovery grant (E. Ukwatta).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
F. Zabihollahy, S. Rajan, and E. Ukwatta declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Cardiac PET, CT, and MRI
Rights and permissions
About this article
Cite this article
Zabihollahy, F., Rajan, S. & Ukwatta, E. Machine Learning-Based Segmentation of Left Ventricular Myocardial Fibrosis from Magnetic Resonance Imaging. Curr Cardiol Rep 22, 65 (2020). https://doi.org/10.1007/s11886-020-01321-1
Published:
DOI: https://doi.org/10.1007/s11886-020-01321-1