Abstract
Urban air pollutants cause a wide range of acute and chronic effects on the respiratory system of children that can be devastating. In this study, the respiratory health of children was assessed in the capital city of India where the level of air pollution is much above the National Ambient Air Quality Standards. The study was carried out in Delhi, and the findings were compared with those of rural West Bengal and Uttaranchal. The prevalence of respiratory symptoms was determined through a structured respiratory symptomlogy questionnaire and personal interviews. Air quality data were collected from Central and State Pollution Control Boards and also obtained by direct measurements using a portable aerosol monitor. Based on the data collected on the cohort of children participating in this study, 32.1% of children in Delhi suffered from respiratory problems in contrast to 18.2% of rural children (control). The respiratory symptoms were more prevalent in girls than in boys. A strong, statistically significant positive association was observed between PM10 level in Delhi’s air and the prevalence of lower respiratory tract symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epidemiological studies throughout the world have established a close association between urban air pollution and human diseases (Dockery et al. 1993; Samet et al. 2000). Air pollution is a complex mixture of various gases, particulates, hydrocarbons, and transition metals. Of all these pollutants, the association between air pollution and adverse health conditions is strongest and most consistent for respirable suspended particulate matter (RSPM) with an aerodynamic diameter <10 μm (PM10). The health risk from particulate pollution is high for some susceptible groups such as the children and the elderly persons, and those with diseases of the heart and lungs (Ulrich et al. 2002).
Diseases of the lungs and the airways are often manifested by one or more symptoms that can be easily recognized. Thus, the presence of a particular symptom or a group of symptoms can confirm the presence of an underlying disease in the upper or lower airways. Respiratory symptoms are classified into two broad groups: (1) upper respiratory symptoms (URS), which include running and stuffy nose, sinusitis, sore throat, cold head, fever, and burning or red eyes, and (2) lower respiratory symptoms (LRS), which include wheezing, wet cough, dry cough, phlegm, shortness of breath, and chest discomfort or pain. Most of the respiratory diseases underlying these symptoms are caused by bacterial, fungal, or viral infections or by structural or functional damage to the respiratory system. Very often the symptoms of a respiratory disease are aggravated following exposure to air pollutant.
Children represent the largest subgroup of the population susceptible to the adverse health effects of urban air pollution (Dockery et al. 2005). Urban air pollutants cause a wide range of acute and chronic effects in the respiratory system of children. Approximately 4 million deaths globally were attributed to respiratory infections between 1997 and 1999 (World Health Organization 2000). Damage to the respiratory system in children can be devastating and permanent, and the adverse effects of air pollution may be obvious in adult life owing to long latent periods for several chronic diseases, including cancer.
Given this background, it seemed important to assess the respiratory health of children in Delhi where the level of air pollution is still much above the National Ambient Air Quality Standards (NAAQS) despite the introduction of compressed natural gas as fuel for public transport vehicles. Air pollution is viewed as a serious problem in Delhi. The Indian capital has the dubious distinction of being one of the most polluted cities in the world. In 2005, Delhi had an annual average concentration of RSPM, i.e., PM10, of 163.4 μg/m3, which was 2.7-fold higher the Indian standards for residential areas (60 μg/m3). The major sources of the city’s air pollution are road traffic (72%), industrial emissions (20%), and emissions from household activities (8%) (Ministry of Environment and Forest, Government of India 2007). Soil resuspension is also an important source of air pollution in the city (Balachandran et al. 2000). Accordingly, the study reported here was undertaken to examine the respiratory health of children in Delhi with the sponsorship of the Central Pollution Control Board (CPCB), Delhi.
Methods
Subjects
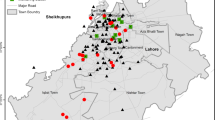
The study was conducted in different areas of Delhi, West Bengal, and Uttaranchal. The sample areas were divided into different homogeneous strata based on air pollution level. Sampling was then carried out following a stratified random sampling procedure under the general guidelines of the simple random sampling without replacement method (Rao 1989). A total of 16,164 children aged between 6 and 17 years participated in this study.
Urban children
Among the participants, 11,628 school-going children were enrolled from 36 schools located in different parts of Delhi. The schools were selected on the basis of the following considerations:
-
located within a 3-km radius of the air quality monitoring stations of the CPCB and National Environmental Engineering Research Institute (NEERI), so that health data of the children could be analyzed based on air quality.
-
represented a cross-section of the residents with comparable representations of children from low, medium, and high socio-economic status (SES).
Rural children (control)
A total of 4,536 children from 17 schools located in the rural areas of Uttaranchal and West Bengal, where the level of ambient air pollution is much lower due to the absence of air-polluting industries and fewer motor vehicles, were enrolled in this study as control subjects. To facilitate a comparison of the urban (Delhi) and control children with respect to fuel use at home, children from homes using liquefied petroleum gas were preferred for enrollment.
Questionnaire survey on respiratory symptoms
The prevalence of respiratory symptoms was determined using a structured respiratory symptomlogy questionnaire based on the questionnaire developed by the British Medical Research Council (BMRC) (Cotes 1987), the American Thoracic Society (ATS) and the National Heart and Lung Institute (NHLI) Division of Lung Diseases (DLD) questionnaire (ATS-DLD-78-C; Ferris 1978), and the International Union Against Tuberculosis and Lung Disease (IUATLD) bronchial symptoms questionnaire (1984) (Burney et al. 1989). The questions mainly addressed respiratory symptoms, such as attacks of shortness of breath, wheezing, dry or wet cough, and chest tightness. The questions were generally formulated to elicit information covering the 12-month period preceding completion of the questionnaire. It also included extended items on asthma, asthma-like symptoms, and allergies. After consent had been obtained from the school principal, the respiratory health questionnaires were distributed among the school children. Completed questionnaire forms signed by the parent or guardian and countersigned by the class teacher were collected from the respective schools.
Air quality data
Air quality data on PM10 and oxides of sulphur and nitrogen (SOx and NOx) in the ambient air of the study areas were collected from fixed-site monitoring stations of the Central and State Pollution Control Boards . The level of PM10 in the indoor air of the households of the participating children was also measured, using portable, battery-operated laser photometers (DustTrakTM Aerosol monitor, model 8520; TSI, Minneapolis, MN).
Statistical analysis
The collected data were processed and analyzed in the EPI info ver. 6.0 (Centers for Disease Control and Prevention, Atlanta, GA) and SPSS software packages (SPSS, Chicago, IL). The chi-square test was performed on dichotomous or multinomial qualitative variables, and the Student’s t test was used for quantitative variables with a normal distribution and homogeneous variances. A descendant stepwise logistic regression adjusted over potential confounding variables was carried out for the multivariate analysis.
Ethical clearance
The Institutional Ethics Committee of Chittaranjan National Cancer Institute (CNCI), Kolkata approved the study protocol.
Results
Study population
Among the 11,628 school-going children in Delhi who participated in this study, 7,757 were boys and 3,871 were girls. Among the 4,536 children who comprised the control group, 2,950 were boys and 1,586 were girls. The age of the children varied between 6 and 17 years, with the majority of these children (approx. 55%) in both the urban and rural groups being 12–14 years of age.
Demographic characteristics
The characteristics of both groups of children are presented in Table 1. Based on these data, the children of Delhi (case) and those of the rural areas of Uttaranchal and West Bengal (control) were comparable (p > 0.05, non-significant) with respect to age, gender, body mass index (BMI), exposure to parental smoking, religion, and eating habits. However, the level of education attained by the parents and the family income were lower for children in the control group than for those in Delhi (p < 0.05).
Air pollution level
Comparison of the air quality of Delhi with that of the control areas revealed significantly higher levels of all pollutants tested in the former. Although the SPM and RSPM levels exceeded the national standards in both the control areas and in Delhi, the latter had twofold higher levels of these pollutants. The annual average concentration (± standard deviation) of PM10 in Delhi was 161.3 ± 4.9 μg/m3 , which is significantly higher than the 74.6 ± 3.3 μg/m3 measured in the control areas. The mean concentrations of sulfur dioxide (SO2) and nitrogen dioxide (NO2) in the urban air during this same period were 9.6 ± 1.0 and 50.1 ± 7.1 μg/m3, respectively, which were within the permissible limit. In the control areas, the concentrations of these two pollutants were 5.6 ± 2.2 and 30.3 ± 5.2 μg/m3, respectively. The annual average concentrations of PM2.5 and PM1 in Delhi were 53.6 ± 4.2 and 44.7 ± 3.6 μg/m3; in the control areas, these were 34.6 ± 6.8 and 25.7 ±5.5 μg/m3 respectively (Table 2).
Prevalence of respiratory symptoms
The prevalence of respiratory symptoms was recorded by means of the questionnaire survey and personal interview. We found that one or more respiratory symptoms were present in the preceding 3-month period in nearly one-third (32.1%) of children in Delhi. In contrast, 18.2% of the rural children had experienced respiratory symptoms during the same period (Table 3). The respiratory symptoms were more prevalent in girls than in boys in both the rural and urban settings. The girl:boy ratio with respect to symptom prevalence was 1.21 in Delhi and 1.3 in the rural areas. The children in Delhi exhibited a greater prevalence of both URS (23.1 vs. 14.6%) and LRS (17.0 vs. 8.0%) than the controls. The prevalence of the respiratory symptoms complex (RSC) varied in different parts of the city, being maximum in the residents of Central Delhi, where the level of particulate pollution was also high. The concentration of PM10 was least in South Delhi, and this was reflected in the prevalence of RSC in the residents of this part of the city, namely, the prevalence of RSC was the lowest here. Respiratory symptoms, both URS and LRS, were more prevalent during the winter, followed by the summer and monsoon, corresponding to the concentration of PM, the concentration of which was the highest during the winter and lowest during the monsoon (Fig. 1).
Prevalence of individual URS
The prevalence of five URS, namely, sinusitis, rhinitis (running or stuffy nose), sneezing, sore throat, and common cold with fever, were the most prevalent URS reported in this study. In general, 23.1 and 14.6% of the children in Delhi and the rural areas, respectively, had experienced one or more of these URS in the preceding 3 months. URS were more prevalent in girls than in boys in Delhi (26.5 vs. 21.4%) and in the control group (18.0 vs. 12.8%; p < 0.05). The girl:boy ratio of URS prevalence was 1.24 in Delhi and 1.40 in the control group, implying that the prevalence of URS showed a female predominance, especially in rural areas. Running or stuffy nose is associated with rhinitis. Nearly 90% of rhinitis cases in children is caused by hypersensitivity, i.e., allergic reactions to a host of environmental allergens. This symptom was present in 9.6% of the children of Delhi and in 5.8% of the control children, which is a highly significant difference (p < 0.05). The children of Delhi had a 1.7-fold increased prevalence of sneezing than control children, and the difference was highly significant. Sore throat was reported by 7.4% children of Delhi compared with 4.9% of the control children. More than 10% of the children of Delhi suffered from common cold and fever in the preceding 3 months compared with 5.2% in the control children.
Prevalence of individual LRS
The overall prevalence of LRS was significantly higher (p < 0.001) among children residing in Delhi than among their rural counterparts (control). Among the former, boys had a slightly greater prevalence of LRS than girls (17.4 vs. 16.4%), whereas the opposite was the case among the control group [8.5 (girls) vs. 7.7% (boys)]. Dry cough was present in 6.6% of the children of Delhi and 3.3% of the control children. Children from north and central Delhi suffered most from a dry cough, while the prevalence was lowest in south Delhi. Cough with phlegm (sputum production) or wet cough was present in 7.0% of the children of Delhi; in contrast, only 3.8% of the children in the control group had this symptom (p < 0.001). Children from north, west, and central Delhi suffered more from a cough with phlegm than did children from east and south Delhi. This symptom was significantly more prevalent during the winter than during the summer and monsoon [ winter vs. summer: odds ratio (OR) 1.98, 95% confidence interval (CI) 1.34–2.71; winter vs. monsoon: OR 2.23, 95% CI 1.55–2.95). Wheeze, i.e., a whistling sound during breathing, was present in 4.8% of the children of Delhi and in 2.7% of the control children. Thus, Delhi’s children had a 1.8-fold higher prevalence of wheeze than the controls (difference was highly significant at p < 0.05). Pain or tightness of the chest was present in 3.3% of the boys and 3% of the girls of Delhi in the preceding 3 months, with an overall prevalence of 3.2%. In contrast, 1.2 % of the control children (1% of boys and 1.6% of girls) had this symptom. Out of breath or breathless on exertion was reported by 5.9% of the children of Delhi compared with 2.9% of the control children (p < 0.001). Disturbed sleep due to breathing problems was reported by 2.2% of the children of Delhi and 0.7% of the rural children (p < 0.001).
Weak positive association between PM10 level in breathing air and prevalence of URS
When the potential confounders, such as SES, parental smoking, age, and gender, were controlled for in a multivariate logistic regression analysis, only sore throat (OR 1.25, 95% CI 1.03–1.52, p < 0.05) and common cold with fever (OR 1.35, 95% CI 1.12–1.65, p < 0.05) were found to be positively associated with particulate pollution (Table 4).
Strong positive association between PM10 level in breathing air and prevalence of LRS in children
Unlike URS, a strong, statistically significant positive association was observed between PM10 level in Delhi’s air and the prevalence of six symptoms of LRS in children in the preceding 3 months (Table 5). Using multivariate logistic regression analysis after controlling for potential confounders, such as parental smoking and SES, we found that particulate pollution was positively associated with all six symptoms of LRS. The strongest association was for sleep disturbance due to breathing trouble and dry cough, followed by chest pain or discomfort, breathlessness on exertion, cough with sputum production, and wheeze. In essence, the prevalence of LRS increases with increasing concentrations of particulate pollution in the breathing air.
The sample areas were divided into different homogeneous strata based on air pollution level (in μg/m3: 50–75; 76–100; 101–125; 126–150; >150). Taking the prevalence of individual symptoms at the low pollution level (PM10 = 50–70 μg/m3) as the constant (OR 1) in the conditional regression analysis, the prevalence of LRS symptoms was found to be doubled or tripled when the particulate pollution level was elevated (PM10 >125 μg/m3 ; Table 6).
Discussion
Compared with age-and sex-matched rural controls, there was a remarkably higher prevalence of URS and LRS among the school-ages children of Delhi participating in this study. The children from the control areas (rural areas of West Bengal and Uttaranchal) were comparable with the children from the exposed area (Delhi) in all respects with the exception of the level of RSPM (PM10). These findings could be linked to city’s high level of ambient air pollution because a large number of studies have shown positive associations between air pollution and respiratory symptoms (Romieu et al. 2002).
The prevalence of RSC varied in different parts of the city, reaching a maximum among the residents of Central Delhi where the level of particulate pollution was also high. The concentration of PM10 was least in South Delhi, and this was reflected by the lowest prevalence of RSC among the residents of this part of the city. Respiratory symptoms, both URS and LRS, were more prevalent during the winter followed by the summer and monsoon, which again corresponds with the concentration of PM, which was highest during the winter and lowest during the monsoon. The prevalence of RSC varied with seasons, again showing links to PM10 level as the level of PM10 was lowest during the monsoon and highest during the winter. Another important confounder was SES, with the lower the SES, the higher the prevalence of RSC. Poverty and lower social status are associated with a large family size, crowded living conditions, poorer access to medical care, higher smoking rates, nutritional deficits, and exposure to environmental pollutants, including urban air pollution and stressful living environments. These factors may contribute individually or perhaps interact among themselves to increase the susceptibility to respiratory diseases. During the statistical evaluation, the confounder, i.e, SES, was taken into account and controlled for.
Upper and lower respiratory symptoms, which were found in excess in children of Delhi, could be a fall-out of a greater interaction of the airways with allergens and pathogens and/or impairment in lung defense. A review of the literature on possible associations between air pollution and respiratory symptoms in children revealed that outdoor and indoor air pollution are positively associated with upper and lower respiratory tract infections in children (Chauhan et al. 2005). Available evidence conclusively supports the association between outdoor air pollution, including PM10, PM2.5, NO2, SO2, and ozone, and increased upper and lower respiratory symptoms in children. Many of these symptoms are related to infections. Viral and bacterial infections can cause severe pathological abnormalities in both the upper and lower respiratory tract, with the extent of epithelial damage varying with the pathogen type. In particular, the lower airway epithelium between the bronchial and alveolar regions is more susceptible than the nasal, laryngeal and tracheal regions. It is possible that the penetration of pathogens into the epithelium could be facilitated by both epithelial shedding and reduced ciliary clearance, resulting in easier access of the pathogen to antigen-presenting cells and, consequently, leading to increased inflammation. Acute respiratory infections (ARIs) are divided into two main groups; upper respiratory tract infections (URTIs) and lower respiratory tract infections (LRTIs). The risk of severe ARIs is greatest in very young children and in the elderly. The World Health Organization (WHO) has defined URTIs as a combination of symptoms that include one or more of the following; cough with or without fever, blocked or running nose, sore throat and ear discharge (World Health Organization 1997). URTIs are usually viral in origin and include the common cold viruses, such as rhinoviruses and corona viruses. In contrast, LRTIs involve infections of the lung and are associated with symptoms like cough and dyspnea, bronchitis, and pneumonia, which usually present in serious forms. URTIs and LRTIs are not mutually exclusive; they frequently coexist during the same episode of respiratory infections. Bacteria and viruses cause infection in both the upper and lower respiratory tracts, and upper respiratory infections are often followed or accompanied by lower respiratory infections (Chauhan et al. 2005).
There has been a series of studies investigating the link between URTIs and air pollution. An increase in total suspended particle and NO2 levels of 10 and 70 μg/m3, respectively, was found to be associated with a 27 and 28% increase in cases of laryngo-tracheo-bronchitis (Schwartz et al. 1991). Traffic-related air pollution and the risk of respiratory diseases in a cohort of 4,000 children were investigated in the Netherlands, and a positive association was observed between air pollution and URTIs. A study in the UK investigated the association between the number of general practitioner consultations for upper respiratory tract diseases, excluding allergic rhinitis, and outdoor air pollution. In children aged 0–14 years, a 3.5-fold increase in the number of such consultations was observed for an increase in SO2 levels of between 13 and 31 μg/m3 (Hajat et al. 1999, 2002). In another study in Taiwan, Hwang and Chan (2002) observed a 0.3–1.3% increase in the number of consultations with physicians with a 10% increase in the levels of NO2, SO2, and PM10. In a cross-sectional study in ten different areas of Switzerland in children aged 6–15 years, the risk of bronchitis between the most and least polluted areas was found to be significant with an OR of 2.17 for PM10 (Braun-Fahrlander et al. 1997). It is therefore quite possible that air pollution may modify symptoms in children who are already infected.
Diesel exhaust particles have been identified as the major contributing factor to allergy (Sydbom et al. 2001; Riedl and Diaz-Sanchez 2005). In our study, allergic rhinitis (running or stuffy nose), wheeze, cough, and dyspnea were present in a substantial number of the children of Delhi. Allergic rhinitis is one of the most common chronic diseases in children (Meltzer 2006). It can significantly impact a child’s health, as it impairs the quality of life, and it can predispose to the development of co-morbidities, such as asthma (Meltzer 2006). The poor air quality of Delhi may account for these symptoms because a close relationship exists between outdoor air pollution and sinusitis (Wolf 2002).Exposure to fungal spores, such as those of Alternaria, could also elicit these symptoms (Delfino et al. 2002). A European study has shown that ambient particles (PM10) from combustion sources act as carriers of allergens (such as pollen) that could elicit allergic reactions in the airways following inhalation (Namork et al. 2006).
The combustion of automotive fuels produces a variety of outdoor pollutants, such as NO2, SO2, and PM10. There is increasing evidence to suggest that exposure to these pollutants is positively associated with the genesis of several respiratory diseases in children as particulate air pollutants are able to penetrate the lower airways in children (Bunn et al. 2001). In many epidemiological studies of outdoor NO2 and PM10 exposure, an association has been found between adverse health effects and exposure to these pollutants, often at levels well below the current WHO guidelines. Many of these functions can be modulated by exposure to PM10, NO2, and other air pollutants (Chauhan and Johnston 2003; Chauhan et al. 2005).
Unlike the concentration of RSPM (PM10), the levels of SOx and NOx in the air of Delhi were within established standards. Therefore, it seems possible that PM, rather than SOx or NOx, was primarily responsible for the adverse respiratory changes recorded in the children of Delhi in this study. In agreement with this, epidemiological studies have shown that particulate matter, but not SO2, is associated with increased prevalence of URS and LRS in urban children (Aekplakorn et al. 2003) and adolescents (Pierse et al. 2006).
The World Bank has estimated that India spends about 5,500 crore rupees annually for the treatment of ailments caused by air pollution, of which the health cost of air pollution for Delhi alone was about 1,000 crore rupees (Mittal et al. 2004).Thus, these findings are expected to serve as reference data for future monitoring studies of urban air pollution with respect to public health, in particular, that of children. They will also serve as guidelines in monitoring programs and for intervention policies aimed at bettering the situation.
Reference
Aekplakorn W, Loomis D, Vichit-Vadakan N, Shy C, Plungchuchon S (2003) Acute effects of SO2 and particles from a power plant on respiratory symptoms of children, Thailand. S East Asian J Trop Med Public Health 34(4):906–914
Balachandran S, Meena BR, Khillare PS (2000) Particle size distribution and its elemental composition in the ambient air of Delhi. Environ Int 26(1–2):49–54
Braun-Fahrlander C, Vuille JC, Sennhauser FJ et al (1997) Respiratory health and long-term exposure to air pollutants in Swiss school children. SCARPOL team: Swiss study on childhood allergy and respiratory symptoms with respect to air pollution, climate and pollen. Am J Respir Crit Care Med 155(3):1042–1049
Bunn HJ, Dinsdale D, Smith T, Grigg J (2001) Ultrafine particles in alveolar macrophages from normal children. Thorax 56(12):932–934
Burney PG, Laities LA, Perdrizet S et al (1989) Validity and repeatability of the IUATLD (1984) Bronchial Symptom Questionnaire: an international comparison. Eur Respir J 2(10):940–945
Chauhan A, Johnston SL (2003) Air pollution and infection in respiratory illness. Br Med Bull 68:95–112
Chauhan A, Chatterjee A, Johnston SL (2005). Acute respiratory infections. In: Effects of air pollution on children’s health and development: a review of the evidence. World Health Organization, Special Programme on Health and Environment. European Center for Environment and Health, Bonn, pp 44–69
Cotes JE (1987) Medical Research Council Questionnaire on Respiratory Symptoms. Lance 31(2):1028
Delfino RJ, Zeiger RS, Seltzer JM, Street DH, McLaren CE (2002) Association of asthma symptoms with peak particulate air pollution and effect modification by anti inflammatory medication use. Environ Health Perspect 110(10):A607–617
Dockery DW, Pope CA, XU X III (1993) An association between air pollution and mortality in six U.S. cities. N Eng J Med 329(24):1753–1759
Dockery DW, Skerrett PJ, Walters D, Gilliland F (2005) Development of lung function. In: Effects of air pollution on children’s health and development: a review of the evidence. World Health Organization Special Programme on Health and Environment. European Centre for Environment and Health, Bonn, pp 108–133
Ferris BG (1978) Epidemiology standardization project. Am Rev Respir Dis 118:1–88
Hajat S, Haines A, Goubet SA, Atkinson RW, Anderson HR (1999) Association of air pollution with daily GP consultations for asthma and other lower respiratory condition in London. Thorax 54:597–605
Hajat S, Anderson HR, Atkinson RW, Haines A (2002) Effects of air pollution on general practitioners consultations for upper respiratory diseases in London. Occu Environ Med 59(5):294–299
Hwang JS, Chan CC (2002) Effects of air pollution on daily clinic visits for lower respiratory tract illness. Am J Epidemiol 155(1):1–10
Meltzer EO (2006) Allergic rhinitis: managing the pediatric spectrum. Allergy Asthma Proc 27(1):2–8
Mittal A, Arora A, Mandal A (2004) Vehicular pollution by introduction of CNG in Delhi—a case study. (abstract) Clean Air Initiative: Better Air Quality (BAQ), 2004
Ministry of Environment and Forest, Government of India (1997). White Paper on Pollution in Delhi with an Action Plan. Ministry of Environment and Forest, New Delhi
Namork E, Johansen BV, Lovik M (2006) Detection of allergens adsorbed to ambient air particles collected in four European cities. Toxicol Lett 165(1):71–78
Pierse N, Rushton L, Harris RS, Kuchni CE, Silverman M, Grigg J (2006) Locally generated particulate pollution and respiratory symptoms in young children. Thorax 61(3):216–220
Rao NSN (1989) Elements of health statistics. Tara Book Agency, Varanasi,
Riedl M, Diaz-Sanchez D (2005) Biology of diesel exhaust effects on respiratory function. J Allergy Clin Immunol 115(2):221–228
Romieu I, Samet JM, Smith KR, Bruce N (2002) Outdoor air pollution and acute respiratory infections among children in developing countries. J Occup Environ Med 44(7):640–649
Samet JM, Domonici F, Frank C, Curriero CI, Zeger SL (2000) Fine particulate air pollution and mortality in 20 U.S. cities, 1987–1994. N Engl J Med 343(24):1742–1749
Schwartz J, Spix C, Wichmann HE, Malin E (1991) Air pollution and acute respiratory illness in five German communities. Environ Res 56(1):1–14
Sydbom A, Blomberg A, Parnia S, Stenfors N, Sandstorm T, Dahlen SE (2001) Health effects of diesel exhaust emissions. Eur Respir J 17(4):733–746
Ulrich MM, Alink GM, Kumarathasan P, Vincent R, Boere AJ, Cassee FR (2002) Health effects and time course of particulate matter on the cardiopulmonary system in rats with lung inflammation. J Toxicol Environ Health A 65(20):1571–1595
Wolf C (2002) Urban air pollution and health: an ecological study of chronic rhinosinusitis in Cologne, Germany. Health Place 8(2):129–139
World Health Organization (1997) Integrated management of childhood illness (documents WHO/CHD 97.3 A-G). World Health Organization, Geneva
World Health Organization (2000) The world health report 2000—health systems: improving performance. World Health Organization, Geneva
Acknowledgments
I would like to thank the Central Pollution Control Board (CPCB), Delhi, for providing the funding to carry out the study. I would also like to thank all of the children, parents, teachers, and school principals, without whose enthusiasm and cooperation the study would have been impossible.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Siddique, S., Ray, M.R. & Lahiri, T. Effects of air pollution on the respiratory health of children: a study in the capital city of India. Air Qual Atmos Health 4, 95–102 (2011). https://doi.org/10.1007/s11869-010-0079-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11869-010-0079-2