Abstract
Objective
To conduct a meta-analysis of studies assessing abnormal glucose metabolism (AGM) prevalence among patients with primary aldosteronism (PA), calculating a combined pooled prevalence and summarizing metabolic parameters associated the pooled prevalence for comparative group.
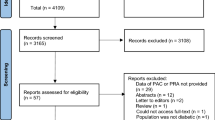
Method
Four electronic databases (PubMed, EMBASE, Cochrane CENTRAL, and ISI-Web of Science) were systematically retrieved with no language and time restriction. Studies about elevated level of glucose metabolism in primary aldosteronism were included.
Result
Data were available in 16 studies. The pooled analysis revealed that the prevalence of elevated glucose in PA was 22.41 % (95 % CI 16.77–28.05 %), the retrospectively calculated prevalence was 31.20 % (95 % CI 15.81–46.60 %) for impaired fasting glucose, 26.19 % (95 % CI 15.17–37.21 %) for impaired glucose tolerance, 15.22 % (95 % CI 9.93–20.51 %) for diabetes mellitus. Prevalence of AGM in PA was higher than that in essential hypertension (OR = 1.55, 95 % CI 1.01–2.36, p = 0.04). From comparative groups, patients with primary aldosteronism had a lower level of insulin sensitivity indicators in comparison with normal group (p < 0.01). On the other hand, insulin resistance which presented by HOMA index was stronger in PA group than in normal control group (WMD = 0.41, 95 % CI 0.17, 0.65; p = 0.001), whereas it was weaker than that in EH group (WMD = −0.37, 95 % CI −0.62, −0.13; p = 0.003).
Conclusion
There is a significant prevalence of elevated level of glucose metabolism in patients with PA. Awareness and treatment of this pre-diabetic or diabetic state are necessary.



Similar content being viewed by others
References
Conn JW (1965) Hypertension, the potassium ion and impaired carbohydrate tolerance. N Engl J Med 273(21):1135–1143
Fallo F, Veglio F, Bertello C et al (2006) Prevalence and characteristics of the metabolic syndrome in primary aldosteronism. J Clin Endocrinol Metab 91(2):454–459
Connell JM, MacKenzie SM, Freel EM et al (2008) A lifetime of aldosterone excess: long-term consequences of altered regulation of aldosterone production for cardiovascular function. Endocr Rev 29(2):133–154
Quinkler M, Born-Frontsberg E, Fourkiotis VG (2010) Comorbidities in primary aldosteronism. Horm Metab Res 42(6):429–434
Strauch B, Widimsky J, Sindelka G et al (2003) Does the treatment of primary hyperaldosteronism influence glucose tolerance? Physiol Res 52(4):503–506
Colussi G, Catena C, Lapenna R et al (2007) Insulin resistance and hyperinsulinemia are related to plasma aldosterone levels in hypertensive patients. Diabetes Care 30(9):2349–2354
Giacchetti G, Ronconi V, Turchi F et al (2007) Aldosterone as a key mediator of the cardiometabolic syndrome in primary aldosteronism: an observational study. J Hypertens 25(1):177–186
Kreze AS, Kreze-Spirova E, Mikulecky M (2000) Diabetes mellitus in primary aldosteronism. Bratisl Lek Listy 101(4):187–190
Choi CS, Thompson CB, Leong PK et al (2001) Short-term K(+) deprivation provokes insulin resistance of cellular K(+) uptake revealed with the K(+) clamp. Am J Physiol Renal Physiol 280(1):F95–F102
Stroup DF, Berlin JA, Morton SC et al (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 283(15):2008–2012
Singer S, Das-Munshi J, Brahler E (2010) Prevalence of mental health conditions in cancer patients in acute care–a meta-analysis. Ann Oncol 21(5):925–930
Biddle DA, Morris SB (2011) Using Lancaster’s mid-P correction to the Fisher’s exact test for adverse impact analyses. J Appl Psychol 96(5):956–965
Lydersen S, Laake P (2003) Power comparison of two-sided exact tests for association in 2 × 2 contingency tables using standard, mid p and randomized test versions. Stat Med 22(24):3859–3871
Brown L, Cai T, DasGupta A (2001) Interval estimation for a binomial proportion. Stat Sci 16:101–117
Higgins JP, Green S, Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0, in http://www.cochrane-handbook.org/
Egger M, Davey Smith G, Schneider M et al (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50(4):1088–1101
Catena C, Lapenna R, Baroselli S et al (2006) Insulin sensitivity in patients with primary aldosteronism: a follow-up study. J Clin Endocrinol Metab 91(9):3457–3463
Fallo F, Della Mea P, Sonino N et al (2007) Adiponectin and insulin sensitivity in primary aldosteronism. Am J Hypertens 20(8):855–861
Haluzik M, Sindelka G, Widimsky J Jr et al (2002) Serum leptin levels in patients with primary hyperaldosteronism before and after treatment: relationships to insulin sensitivity. J Hum Hypertens 16(1):41–45
Iacobellis G, Petramala L, Cotesta D et al (2010) Adipokines and cardiometabolic profile in primary hyperaldosteronism. J Clin Endocrinol Metab 95(5):2391–2398
Ishimori M, Takeda N, Okumura S et al (1994) Increased insulin sensitivity in patients with aldosterone producing adenoma. Clin Endocrinol (Oxf) 41(4):433–438
Matrozova J, Steichen O, Amar L et al (2009) Fasting plasma glucose and serum lipids in patients with primary aldosteronism: a controlled cross-sectional study. Hypertension 53(4):605–610
Mosso LM, Carvajal CA, Maiz A et al (2007) A possible association between primary aldosteronism and a lower beta-cell function. J Hypertens 25(10):2125–2130
Reincke M, Meisinger C, Holle R et al (2010) Is primary aldosteronism associated with diabetes mellitus? Results of the German Conn’s Registry. Horm Metab Res 42(6):435–439
Widimsky J Jr, Sindelka G, Haas T et al (2000) Impaired insulin action in primary hyperaldosteronism. Physiol Res 49(2):241–244
Widimsky J Jr, Strauch B, Sindelka G et al (2001) Can primary hyperaldosteronism be considered as a specific form of diabetes mellitus? Physiol Res 50(6):603–607
Sindelka G, Widimsky J, Haas T et al (2000) Insulin action in primary hyperaldosteronism before and after surgical or pharmacological treatment. Exp Clin Endocrinol Diabet 108(1):21–25
Fischer E, Adolf C, Pallauf A et al. (2013) Aldosterone excess impairs first phase insulin secretion in primary aldosteronism. J Clin Endocrin Metab 98(6):2513–2520
Nanba K, Tamanaha T, Nakao K et al (2012) Confirmatory testing in primary aldosteronism. J Clin Endocrinol Metab 97(5):1688–1694
Reungjui S, Pratipanawatr T, Johnson RJ et al (2008) Do thiazides worsen metabolic syndrome and renal disease? The pivotal roles for hyperuricemia and hypokalemia. Curr Opin Nephrol Hypertens 17(5):470–476
Yokoshiki H, Sunagawa M, Seki T et al (1998) ATP-sensitive K + channels in pancreatic, cardiac, and vascular smooth muscle cells. Am J Physiol 274(1 Pt 1):C25–C37
Fallo F, Pilon C, Urbanet R (2012) Primary aldosteronism and metabolic syndrome. Horm Metab Res 44(3):208–214
Underwood PC, Adler GK (2013) The renin angiotensin aldosterone system and insulin resistance in humans. Curr Hypertens Rep 15(1):59–70
Vaidya A, Underwood PC, Hopkins PN et al (2013) Abnormal aldosterone physiology and cardiometabolic risk factors. Hypertension 61(4):886–893
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chen, W., Li, F., He, C. et al. Elevated prevalence of abnormal glucose metabolism in patients with primary aldosteronism: a meta-analysis. Ir J Med Sci 183, 283–291 (2014). https://doi.org/10.1007/s11845-013-1007-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-013-1007-x