Abstract
Purpose
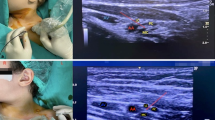
Supraclavicular brachial plexus block is considered as one of the most effective anesthetic methods for upper extremity surgeries. Its major drawback, especially in children, is the risk of pneumothorax, vascular puncture, and failure of the procedure due to inaccurate placement of the needle. Ultrasound-guided needle placement may reduce the risk of complications and increase the accuracy of block, particularly in pediatric patients. There are few published experiences about the efficacy and safety of ultrasound-guided supraclavicular block in children and to our knowledge, it seems that there is no published report about its usage in younger children (less than 6 years of age).
Methods
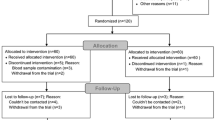
In order to consider the efficacy of ultrasound in younger children, 17 patients aged between 6 months and 6 years were randomly selected. The ultrasound probe was used for proper placement of the needle. After confirmation of the needle location using a nerve locator, the anesthetic agent was injected. The procedure time, establishment time, duration of analgesia, any complications related to the procedure, and the surgeon’s satisfaction were recorded and analyzed.
Results
The procedure time was 10.35 ± 1.22 min, the establishment time was 89.59 ± 18 s, and the duration of analgesia was between 6 and 16 h (mean 9.76 ± 2.57 h). The recovery time was 24.4 ± 6.5 min (range 15–37 min) and the duration of surgeries was 61.3 ± 25.9 min (range 15–110 min). There was no failure of the procedure. Also, there were no complications related to the procedure and the surgeon’s satisfaction during surgery was good or excellent.
Conclusions
This study demonstrates the efficacy and safety of the ultrasound-guided supraclavicular brachial plexus block for orthopedic upper extremity surgeries in patients younger than 6 years of age.



Similar content being viewed by others
References
Gray AT (2006) Ultrasound-guided regional anesthesia: current state of the art. Anesthesiology 104(2):368–373
Chan VW, Perlas A, Rawson R et al (2003) Ultrasound-guided supraclavicular brachial plexus block. Anesth Analg 97(5):1514–1517
Bashein G, Haschke RH, Ready LB (1984) Electrical nerve location: numerical and electrophoretic comparison of insulated vs uninsulated needles. Anesth Analg 63(10):919–924
Keschner MT, Michelsen H, Rosenberg AD et al (2006) Safety and efficacy of the infraclavicular nerve block performed at low current. Pain Pract 6(2):107–111
Sinha SK, Abrams JH, Weller RS (2007) Ultrasound-guided interscalene needle placement produces successful anesthesia regardless of motor stimulation above or below 0.5 mA. Anesth Analg 105(3):848–852
Chan VW, Perlas A, McCartney CJ et al (2007) Ultrasound guidance improves success rate of axillary brachial plexus block. Can J Anaesth 54(3):176–182
Li L, Liu X, Herr K (2007) Postoperative pain intensity assessment: a comparison of four scales in Chinese adults. Pain Med 8(3):223–234
Beyer JE, McGrath PJ, Berde CB (1990) Discordance between self-report and behavioral pain measures in children aged 3–7 years after surgery. J Pain Symptom Manage 5(6):350–356
Jacobson SJ, Kopecky EA, Joshi P et al (1997) Randomised trial of oral morphine for painful episodes of sickle-cell disease in children. Lancet 350(9088):1358–1361
McGrath PJ, Rosmus C, Canfield C et al (1998) Behaviours caregivers use to determine pain in non-verbal, cognitively impaired individuals. Dev Med Child Neurol 40:340–343
McGrath PJ, McAlpine L (1993) Psychologic perspectives on pediatric pain. J Pediatr 122(5 Pt 2):S2–S8
Mitchell P (1999) Understanding a young child’s pain. Lancet 354(9191):1708
Pande R, Pande M, Bhadani U et al (2000) Supraclavicular brachial plexus block as a sole anaesthetic technique in children: an analysis of 200 cases. Anaesthesia 55(8):798–802
Tobias JD (2001) Brachial plexus anaesthesia in children. Paediatr Anaesth 11(3):265–275
Suresh S, Wheeler M (2002) Practical pediatric regional anesthesia. Anesthesiol Clin North America 20(1):83–113
De José María B, Banús E, Navarro Egea M et al (2008) Ultrasound-guided supraclavicular vs infraclavicular brachial plexus blocks in children. Paediatr Anaesth 18(9):838–844
Dalens B (1995) Proximal blocks of the upper extremity: benefit/risk ratio. In: Dalens B (ed) Regional anaesthesia in infants, children, and adolescents. Williams & Wilkins, Baltimore, pp 275–314
Riazi S, Carmichael N, Awad I et al (2008) Effect of local anaesthetic volume (20 vs 5 ml) on the efficacy and respiratory consequences of ultrasound-guided interscalene brachial plexus block. Br J Anaesth 101(4):549–556
Kapral S, Krafft P, Eibenberger K et al (1994) Ultrasound-guided supraclavicular approach for regional anesthesia of the brachial plexus. Anesth Analg 78(3):507–513
Williams SR, Chouinard P, Arcand G et al (2003) Ultrasound guidance speeds execution and improves the quality of supraclavicular block. Anesth Analg 97(5):1518–1523
Stone MB, Wang R, Price DD (2008) Ultrasound-guided supraclavicular brachial plexus nerve block vs procedural sedation for the treatment of upper extremity emergencies. Am J Emerg Med 26(6):706–710
Casati A, Danelli G, Baciarello M et al (2007) A prospective, randomized comparison between ultrasound and nerve stimulation guidance for multiple injection axillary brachial plexus block. Anesthesiology 106(5):992–996
Marhofer P, Sitzwohl C, Greher M et al (2004) Ultrasound guidance for infraclavicular brachial plexus anaesthesia in children. Anaesthesia 59(7):642–646
Rubin K, Sullivan D, Sadhasivam S (2009) Are peripheral and neuraxial blocks with ultrasound guidance more effective and safe in children? Paediatr Anaesth 19(2):92–96
Oberndorfer U, Marhofer P, Bösenberg A et al (2007) Ultrasonographic guidance for sciatic and femoral nerve blocks in children. Br J Anaesth 98(6):797–801
Willschke H, Marhofer P, Bösenberg A et al (2005) Ultrasonography for ilioinguinal/iliohypogastric nerve blocks in children. Br J Anaesth 95(2):226–230
Marhofer P, Chan VW (2007) Ultrasound-guided regional anesthesia: current concepts and future trends. Anesth Analg 104(5):1265–1269
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Amiri, H.R., Espandar, R. Upper extremity surgery in younger children under ultrasound-guided supraclavicular brachial plexus block: a case series. J Child Orthop 4, 315–319 (2010). https://doi.org/10.1007/s11832-010-0264-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11832-010-0264-8