Abstract
The aim of this study was to evaluate the association between adipose tissue trans-fatty acid isomers and adiposity. This cross-sectional study included 1,785 subjects from Costa Rica. Fatty acid concentrations (as a percentage of the total fatty acids) in subcutaneous adipose tissue were assessed by gas–liquid chromatography. Dietary intakes were assessed with a food frequency questionnaire. Multivariate linear regression models were used to relate adipose tissue trans-fatty acid content to BMI, waist circumference, and skinfold thickness while adjusting for age, sex, and area of residence. To account for variations in lifestyle, we adjusted for smoking, physical activity, income, self-reported history of diabetes and hypertension, and for adipose tissue alpha-linolenic acid and energy intake in a third model. After adjustments, positive associations were found between 18:2t-fatty acids (primarily from partially hydrogenated oils) and BMI, waist circumference, and skinfold thickness (P for each association <0.01). Rumenic acid was positively associated with skinfold thickness (P < 0.0001), but not with BMI or waist circumference (P > 0.05). Inverse associations were found between 16:1n-7t-fatty acids and skinfold thickness and between 18:1t-fatty acids and BMI and waist circumference (P < 0.0001). This study suggests that individual trans-fatty acid isomers may have divergent effects on adiposity. 18:2t-fatty acids show consistent positive associations with measures of adiposity. These isomer-specific associations are an interesting new finding. Other prospective and intervention studies are necessary to examine these relationships further.
Similar content being viewed by others
Introduction
trans-Fatty acids are unsaturated fatty acids characterized by the trans configuration of their double bonds. The two main industrially produced trans-isomers,18:1t-and 18:2t-fatty acids are created by partial hydrogenation of unsaturated fats and have well documented adverse effects on health [1, 2]. The health effects of 16:1n-7t-fatty acids and 18:2n-7t fatty acids collectively known as conjugated linoleic acid (CLA) are less well understood.
The 9c, 11t isomer of CLA, also known as rumenic acid, is found in ruminant food products. These natural trans-fats originate mainly from biohydrogenation of linoleic acid by fermentive bacteria in ruminants and by endogenous synthesis from vaccenic acid by delta-9 desaturase [3]. Rumenic acid, represents ~80% of all CLA isomers in the diet [4], and is mainly found in dairy products in this population [5].
In humans and monkeys, high 18:1t and 18:2t-fatty acid intake appears to predispose to accumulation of body fat, particularly abdominal fat [6, 7]. Among more than 16,000 men who provided two measurements of abdominal circumference at an interval of 9 years, each 2% increase in total energy from trans-fatty acids (versus the same percent of energy from cis-polyunsaturated fat) was associated with a 2.7-cm increase in abdominal circumference (P < 0.001) after adjustment for measurement error and other risk factors [7]. Among more than 41,000 women who provided two measurements of body weight at an interval of 8 years, increases in trans-fatty acid intake were robustly associated with increases in body weight in both cross-sectional and longitudinal analyses, whereas intakes of other types of fat were not [8]. In a 6-year randomized controlled trial among 42 male African green monkeys feeding ~8% of energy 18:1t- and 18:2t-fatty acids resulted in a threefold greater weight gain compared with controls assigned to a diet containing cis-monounsaturated fatty acids (P < 0.05) [6]. However, evidence from human intervention studies has been inconclusive [9, 10].
The purpose of this study was to evaluate the associations between the most common trans-fatty acid isomers (18:1t, 18:2t, 16:1n-7t and rumenic acid) and adiposity in a population of Costa Rican adults. We used adipose tissue levels of trans-fatty acids as a marker for intake because the trans-fatty acid content of foods has changed considerably and subcutaneous adipose tissue is considered the best choice for the study of long-term fatty acid intake [11, 12].
Methods
Study Population
Subjects were randomly selected population controls from a case–control study on diet and heart disease conducted in Costa Rica as previously described [13]. Participation was 88%. We included a total of 1,334 men and 451 women. Subjects gave informed consent on documents approved by the Human Subjects Committee of the Harvard School of Public Health and the University of Costa Rica.
Data Collection
Data were collected by trained personnel visiting the subjects at their homes. Subjects provided information on socioeconomic, demographic, diet, and medical history during an interview. Anthropometric measures collected were height, weight, waist circumference and skinfold thickness for subscapular, suprailiac and triceps. All anthropometric measurements were taken from subjects wearing light clothing and no shoes, and collected in duplicate and averaged out for analyses. Field workers measured triceps (posterior upper arm, midway between the elbow and acromion), subscapular (1 cm below the lower tip of the scapula), and suprailiac (at the midline and above the iliac crest) using Holtain skinfold calipers. All measurements were taken on the right side of the body. Nonstretching fiberglass or metal tapes were used to measure the waist (smallest horizontal trunk circumference) and hip (largest horizontal circumference around the hip and buttocks) girths. A steel anthropometer and a Detecto bathroom scale or a Seca Alpha Model 770 digital scale accurate to 50 g were used to measure height and weight, respectively. The two scales were calibrated biweekly. Body mass index (BMI) was then calculated as weight (kg) divided by the square of the height (m2). BMI categories were defined by general accepted cut-off points. Normal weight was determined as a BMI lower than 25 kg/m2, overweight as a BMI between 25 and 30 kg/m2 and obesity was defined as a BMI above 30 kg/m2.
A subcutaneous adipose tissue biopsy was collected from the upper buttock with a 16-gauge needle and disposable syringe following procedures previously described [14]. Samples were stored in a cooler at 4 °C and transported to the fieldwork station where they were stored at −80 °C. Within 6 months, they were shipped on dry ice to the Harvard School of Public Health for long term storage in nitrogen tanks. Energy and nutrient intakes were assessed with a food frequency questionnaire developed and validated specifically for use among Costa Ricans [14, 15]. Dietary information obtained by the food frequency questionnaire was used for validation purposes and to assess confounding by dietary factors that do not have good biomarkers of intake. The fatty acid composition of all foods commonly used in Costa Rica was determined [16] and incorporated into the nutrient calculation.
Fatty Acid Analysis
Fatty acids were extracted from adipose tissue and analyzed by gas–liquid chromatography (GLC) [14]. The fatty acids in the adipose tissue biopsy were extracted using hexane/isopropanol (3:2) mixture and esterified with methanol and acetyl chloride. After esterification, the methanol and acetyl chloride were evaporated and the fatty acid methyl esters were dissolved in isooctane. The methyl esters were quantified by GLC using the following parameters: fused silica capillary cis/trans-column SP2560, 100 m × 250 mm internal diameters × 0.20 mm film (Supelco, Belefonte, PA); splitless injection port at 240 °C; hydrogen carrier gas at 1.3 ml/min, constant flow; Hewlett-Packard Model (now Agilent) GC 6890 FID gas chromatograph with 7673 Autosampler injector (Palo Alto, CA); 1 ml of sample injected; temperature program of 90–170 °C at 10 °C/min, 170 °C for 5 min, 170–175 °C at 5 °C/min, 175–185 °C at 2 °C/min, 185–190 °C at 1 °C/min, 190–210 at 5 °C/min, 210 °C for 5 min, 210–250 °C at 5 °C/min, 250 °C for 10 min. Peak retention time and area percentages of total fatty acids were identified by injecting known standards (catalog numbers 47791, GLC-463, GLC-481b, N-16-M, N-21-M, N-23-M, N-24-M, U-45-M, U-46-M, U-59-M, U-71-M and UC-60-M, Nu-Chek_prep, Elysium, MN), and analyzed with the Agilent Technologies ChemStation A.08.03 software (Agilent Technologies, Inc., Palo Alto, CA). Twelve identical samples were analyzed throughout the study. The inter-assay coefficients of variation for 18:1t, 18:2t, and 18:2n-7t (9c,11t) fatty acids were 15.7, 6.4, and 5.2%, respectively. We previously showed that the trans-fatty acid concentration in adipose tissue is a good biomarker of trans-fatty acid intake in the Costa Rican population [14].
Statistical Analysis
Data are presented as means ± SD or n (%). The trans-fatty acids that we used in the analysis were defined as follows: 18:1t = 18:1t (n-7t) + 18:1t (n-9t) + 18:1t (n-11t); 18:2t = 18:2t (n-6tt) + 18:2t (n-6ct) + 18:2t (n-6tc). Data were analyzed with the SAS software v9.1 (SAS Institute, Cary, NC, USA) with the significance level set at P < 0.05. Partial Spearman correlation coefficients were calculated, adjusted for age, sex, and area of residence for the association between adipose tissue fatty acids and several subject characteristics and potential confounders.
Multivariate regression was used to estimate the β coefficients and P values of the association between adipose tissue trans-fatty acid isomer content and indicators of adiposity. These calculations were adjusted for the matching factors age, sex and area of residence. To account for variation in lifestyle and dietary habits, further models adjusted for smoking status, physical activity and income, and self-reported history of diabetes and hypertension. In a third model we also adjusted for adipose tissue alpha-linolenic acid, which is present in partially hydrogenated soybean oil used for cooking and was the major dietary source of 18:2t-fatty acids in this population [13].
Other potential confounders that were examined but not included in the final models were alcohol intake, fruit and vegetable intake, currently on weight loss diet, menopausal status, adipose tissue linoleic acid, arachidonic acid, long chain omega-3 fatty acids, and dietary patterns.
Results
The average BMI of all subjects was 26.4 kg/m2 (Table 1). Subjects in the obese category were more likely to be female, have a higher income, a history of diabetes and hypertension and less likely to be physically active or smoke. Obese subjects had higher adipose levels of 18:2t-fatty acids and arachidonic acid, and lower levels of 18:1t-fatty acids, linoleic acid and alpha-linolenic acid.
The mean percentage plus standard deviation (SD) of trans-fatty acids in adipose tissue as percentage of total fatty acids was 2.7 ± 0.7 for total trans-fatty acids, 1.47 ± 0.53 for 18:1t, 1.15 ± 0.35 for 18:2t, 0.15 ± 0.06 for 16:1n-7t and 0.56 ± 0.18 for rumenic acid (Table 1).
Adipose tissue trans-fatty acid content corresponded with their intake from the diet. The average trans-fatty acid intake as a percentage of total calories was 0.77 ± 0.30% for 18:1t, 0.07 ± 0.07% for 18:2t, 0.06 ± 0.03% for 16:1n-7t and 0.10 ± 0.05% for rumenic acid.
Adipose tissue 18:1t, 18:2t and rumenic acid, but not 16:1n-7t were inversely associated with physical activity (Table 2). Within adipose tissue, the strongest correlation was between 18:1t and 18:2t-fatty acids (Spearman r = 0.51). Rumenic acid was weakly inversely associated with linoleic acid and alpha-linolenic acid (Spearman r = − 0.17 and −0.08, respectively) and weakly positively with arachidonic acid (Spearman r = 0.06) (data not shown).
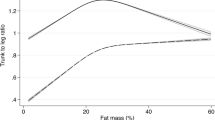
Results of the multivariate regression models for associations were reported as one SD unit increase in adipose tissue trans-fatty acids and measures of adiposity (Table 3). Increased adipose tissue 16:1n-7t- and 18:2t-fatty acids were associated with higher BMI and waist circumference, and 18:1t-fatty acids were associated with lower BMI and waist circumference. In contrast, 16:1n-7t-fatty acids were inversely associated with individual skinfold thicknesses, while rumenic acid was positively associated with each skinfold thickness. Adipose tissue 18:1t-fatty acids were not significantly associated with skinfold thickness. Rumenic acid was not significantly associated with BMI or waist circumference, but was positively related to skinfold thicknesses. In additional analyses, alpha-linolenic acid was inversely associated with BMI (model 3, beta −4.2, p < 0.0001) and waist circumference (model 3, beta −10.0, p < 0.0001).
Discussion
This cross-sectional study in the Costa Rican population evaluated the association between adipose tissue trans-fatty acid isomers and adiposity. We included both industrially produced (18:1t and 18:2t) and naturally occurring (16:1n-7t and 18:2n-7, 9c, 11t) trans-fatty acids. The most striking result was the apparent heterogeneity in the associations between the different trans-fatty acid isomers in adipose tissue and measures of adiposity.
Among the specific trans-fatty acids, the most consistent finding was that the industrial 18:2t-fatty acids, coming from partially hydrogenated oils used for cooking, were associated with increased visceral and subcutaneous adiposity.
In addition to positive associations with adiposity, 18:2 trans-fatty acids have been found to be more adversely related to risk of cardiovascular disease (CVD) than are 18:1 trans-fatty acids [17–19]. A possible explanation for these adverse effects on CVD is that 18:2t-fatty acids are incorporated in the sn-2 position of phospholipids, where polyunsaturated fatty acids are usually found. This substitution might affect membrane properties and have effects on atherosclerotic pathways through increased macrophage adhesion [20].
16:1n-7t-fatty acids, from ruminant food sources, have not been widely investigated. In this study 16:1n-7t-fatty acids were positively associated with BMI and waist circumference, and inversely with skinfold thickness. This suggests that 16:1n-7t-may be associated with increased visceral, rather than subcutaneous fat storage. These findings are in contrast with rumenic acid, also from ruminant food sources, which is associated with increased subcutaneous adiposity. Although differences in fatty acid metabolism between visceral and subcutaneous fat depots have been found [21], we cannot explain the different associations of these natural trans-fatty acids with visceral and subcutaneous adiposity.
The finding of an inverse association between adipose tissue 18:1t-fatty acids and BMI is unexpected, given the positive associations found in other studies where 18:1t-fatty acids were the main trans-fatty acids in the diet [6, 8]. However, although the distribution of fat in monkeys fed a trans-fat diet favored an intra-abdominal distribution, the increases in body weight, weight circumference, subcutaneous and intra-abdominal fat were not significant, which is in line with our study [6]. We cannot exclude that this redistribution of fat also happened in our subjects. Also, Koh-Banerjee et al. [7] reported an increase in waist gain with higher trans-fat intake, but they did not validate the intake of trans-fatty acids in their food frequency questionnaire, which could introduce considerable bias since trans-fat content of foods has changed over time. In addition, short term studies conducted in small animals fed 18:1t-fatty acids as their main source of trans-fatty acids support our findings. These randomized controlled trials with rabbits and mice showed decreases in body weight, and perirenal and epididymal weight when fed diets high in 18:1t-fatty acids [22, 23]. The discrepancy between the observations in this study and those in other studies on industrial trans-fatty acids and weight might also be explained by the relatively low consumption of 18:1t-fatty acids in Costa Rica.
Adipose tissue rumenic acid was not significantly associated with BMI or waist circumference but did relate positively to skinfold thickness. Studies in rodents show associations between CLA and decreases in body fat [24], but in humans the effects of CLA consumption on body weight are inconsistent [9, 10], which is in line with our findings.
Adiposity is primarily caused by an imbalance in energy consumption, leading to deposition of excess calories. However, Flint et al. [25] showed that trans-fatty acid consumption had no effect on either appetite or energy expenditure. Food sources of 18:1t-fatty acids are mostly processed baked goods, while the main source of 18:2t-fatty acids in our population is cooking oil. However, this does not logically explain why 18:1t-fatty acids are associated with decreased adiposity, and 18:2t-fatty acids with increased adiposity. A clear mechanism for the observed associations cannot be given. Also, biochemical mechanisms to explain these observations such as interference with essential fatty acid desaturation and elongation [26], insulin sensitivity [27] and fat cell size [28] does not explain the inverse associations we see with 18:1t-fatty acids and adiposity.
Together with the studies on trans-fatty acid isomers and CVD risk, the results from this study suggest that different associations exist between the individual trans-fatty acid isomers and health outcomes. Currently there is a trend among the food industry to reduce trans-fatty acids in common foods, which then might be replaced with oils that are less hydrogenated and contain relatively more 18:2t-fatty acids. Although the primary goal is to improve public health, this might have more adverse effects because of the adverse associations of 18:2t-fatty acids with CVD and adiposity. While a causal effect cannot be determined in this study, extrapolation of our findings suggests that eliminating all industrial 18:2t-fatty acids would be associated with a 7.1-cm decrease in waist circumference.
The use of adipose tissue trans-fatty acids is both a strength and a limitation of the study. Adipose tissue levels are not dependent on imperfect measures of dietary intake or food composition tables to determine the amount of trans-fatty acids in foods, which can pose a problem in dietary analyses since the trans-fatty acid content of foods can vary considerably over time. However, the concentration of fatty acids in adipose tissue not only reflects intake, but also metabolism and substitutions between fatty acids.
Reverse causation may influence the associations found in this study; increases in body weight are readily noticed by participants, which can lead to changes in energy intake and the choice of foods or to increased physical activity. Also, residual confounding is possible because of imperfect measurements of physical activity, dietary factors, and health consciousness.
In summary, our study provides evidence that individual trans-fatty isomers have divergent effects on adiposity. The main finding is the consistent adverse association between industrial 18:2t and all measures of adiposity. Also, 16:1n-7t and rumenic acid, both trans-isomers mainly found in dairy foods, have divergent effects which has not been reported previously. These isomer-specific associations pose new questions on how trans-fatty acids influence metabolism and weight. Other prospective and intervention studies are necessary to examine this further. Regardless of an association with adiposity, elimination of partially hydrogenated oils from the diet is important in efforts to reduce the burden of cardiovascular disease.
Abbreviations
- BMI:
-
Body mass index
- CLA:
-
Conjugated linoleic acid
- CVD:
-
Cardiovascular disease
- GLC:
-
Gas–liquid chromatography
References
Katan MB, Zock PL, Mensink RP (1995) Dietary oils, serum lipoproteins, and coronary heart disease. Am J Clin Nutr 61:1368S–1373S
Mozaffarian D, Katan MB, Ascherio A, Stampfer MJ, Willett WC (2006) Trans-fatty acids and cardiovascular disease. N Engl J Med 354:1601–1613
Griinari JM, Corl BA, Lacy SH, Chouinard PY, Nurmela KV, Bauman DE (2000) Conjugated linoleic acid is synthesized endogenously in lactating dairy cows by Delta(9)-desaturase. J Nutr 130:2285–2291
Kepler CR, Hirons KP, McNeill JJ, Tove SB (1966) Intermediates and products of the biohydrogenation of linoleic acid by Butyrinvibrio fibrisolvens. J Biol Chem 241:1350–1354
Smit LA, Baylin A, Campos H (2010) Conjugated linoleic acid in adipose tissue and risk of myocardial infarction. Am J Clin Nutr 92(1):34–40
Kavanagh K, Jones KL, Sawyer J, Kelley K, Carr JJ, Wagner JD, Rudel LL (2007) Trans fat diet induces abdominal obesity and changes in insulin sensitivity in monkeys. Obesity (Silver Spring) 15:1675–1684
Koh-Banerjee P, Chu NF, Spiegelman D, Rosner B, Colditz G, Willett W, Rimm E (2003) Prospective study of the association of changes in dietary intake, physical activity, alcohol consumption, and smoking with 9-year gain in waist circumference among 16,587 US men. Am J Clin Nutr 78:719–727
Field AE, Willett WC, Lissner L, Colditz GA (2007) Dietary fat and weight gain among women in the nurses’ health study. Obesity (Silver Spring) 15:967–976
Salas-Salvado J, Marquez-Sandoval F, Bullo M (2006) Conjugated linoleic acid intake in humans: a systematic review focusing on its effect on body composition, glucose, and lipid metabolism. Crit Rev Food Sci Nutr 46:479–488
Li JJ, Huang CJ, Xie D (2008) Anti-obesity effects of conjugated linoleic acid, docosahexaenoic acid, and eicosapentaenoic acid. Mol Nutr Food Res 52:631–645
Baylin A, Kim MK, Donovan-Palmer A, Siles X, Dougherty L, Tocco P, Campos H (2005) Fasting whole blood as a biomarker of essential fatty acid intake in epidemiologic studies: comparison with adipose tissue and plasma. Am J Epidemiol 162:373–381
London SJ, Sacks FM, Caesar J, Stampfer MJ, Siguel E, Willett WC (1991) Fatty acid composition of subcutaneous adipose tissue and diet in postmenopausal US women. Am J Clin Nutr 54:340–345
Kabagambe EK, Baylin A, Ascherio A, Campos H (2005) The type of oil used for cooking is associated with the risk of nonfatal acute myocardial infarction in Costa Rica. J Nutr 135:2674–2679
Baylin A, Kabagambe EK, Siles X, Campos H (2002) Adipose tissue biomarkers of fatty acid intake. Am J Clin Nutr 76:750–757
Kabagambe EK, Baylin A, Allan DA, Siles X, Spiegelman D, Campos H (2001) Application of the method of triads to evaluate the performance of food frequency questionnaires and biomarkers as indicators of long-term dietary intake. Am J Epidemiol 154:1126–1135
Baylin A, Siles X, Donovan-Palmer A, Fernandez X, Campos H (2007) Fatty acid composition of Costa Rican foods including trans-fatty acid content. J Food Comp Anal 20:182–192
Baylin A, Kabagambe EK, Ascherio A, Spiegelman D, Campos H (2003) High 18:2 trans-fatty acids in adipose tissue are associated with increased risk of nonfatal acute myocardial infarction in Costa Rican adults. J Nutr 133:1186–1191
Lemaitre RN, King IB, Raghunathan TE, Pearce RM, Weinmann S, Knopp RH, Copass MK, Cobb LA, Siscovick DS (2002) Cell membrane trans-fatty acids and the risk of primary cardiac arrest. Circulation 105:697–701
Lemaitre RN, King IB, Mozaffarian D, Sotoodehnia N, Rea TD, Kuller LH, Tracy RP, Siscovick DS (2006) Plasma phospholipid trans-fatty acids, fatal ischemic heart disease, and sudden cardiac death in older adults: the cardiovascular health study. Circulation 114:209–215
Calder PC, Bond JA, Harvey DJ, Gordon S, Newsholme EA (1990) Uptake and incorporation of saturated and unsaturated fatty acids into macrophage lipids and their effect upon macrophage adhesion and phagocytosis. Biochem J 269:807–814
Hannukainen JC, Kalliokoski KK, Borra RJ, Viljanen AP, Janatuinen T, Kujala UM, Kaprio J, Heinonen OJ, Viljanen T, Haaparanta M, Iozzo P, Parkkola R, Nuutila P (2010) Higher free fatty acid uptake in visceral than in abdominal subcutaneous fat tissue in men. Obesity (Silver Spring) 18:261–265
Faulconnier Y, Roy A, Ferlay A, Chardigny JM, Durand D, Lorenz S, Gruffat D, Chilliard Y (2006) Effect of dietary supply of butters rich either in trans-10–18 : 1 or in trans-11–18 : 1 plus cis-9, trans-11–18 : 2 on rabbit adipose tissue and liver lipogenic activities. Br J Nutr 96:461–468
Atal S, Zarnowski MJ, Cushman SW, Sampugna J (1994) Comparison of body weight and adipose tissue in male C57Bl/6 J mice fed diets with and without trans-fatty acids. Lipids 29:319–325
Park Y, Albright KJ, Liu W, Storkson JM, Cook ME, Pariza MW (1997) Effect of conjugated linoleic acid on body composition in mice. Lipids 32:853–858
Flint A, Helt B, Raben A, Toubro S, Astrup A (2003) Effects of different dietary fat types on postprandial appetite and energy expenditure. Obes Res 11:1449–1455
Thomassen MS, Rortveit T, Christiansen EN, Norum KR (1984) Changes in the content of n-6 fatty acids in liver phospholipids in rats as a consequence of partially hydrogenated dietary oils. Br J Nutr 51:315–322
Ibrahim A, Natrajan S, Ghafoorunissa R (2005) Dietary trans-fatty acids alter adipocyte plasma membrane fatty acid composition and insulin sensitivity in rats. Metabolism 54:240–246
Ostlund-Lindqvist AM, Albanus L, Croon LB (1985) Effect of dietary trans-fatty acids on microsomal enzymes and membranes. Lipids 20:620–624
Conflict of interest statement
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Smit, L.A., Willett, W.C. & Campos, H. trans-Fatty Acid Isomers in Adipose Tissue Have Divergent Associations with Adiposity in Humans. Lipids 45, 693–700 (2010). https://doi.org/10.1007/s11745-010-3442-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11745-010-3442-z