Abstract
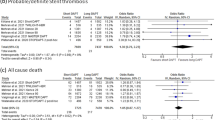
Optimal dual antiplatelet therapy (DAPT) strategy in high-bleeding risk (HBR) patients presenting with acute coronary syndrome remains debated. We sought to investigate the use of clopidogrel versus ticagrelor in HBR patients with acute coronary syndrome and their impact on ischemic and bleeding events at 1 year. In the START-ANTIPLATELET registry (NCT02219984), consecutive patients with ≥ 1 HBR criteria were stratified by DAPT type in clopidogrel versus ticagrelor groups. The primary endpoint was net adverse clinical endpoints (NACE), defined as a composite of all-cause death, myocardial infarction, stroke, and major bleeding. Of 1209 patients with 1-year follow-up, 553 were defined at HBR, of whom 383 were considered eligible for the study as on DAPT with clopidogrel (174 or 45.4%) or ticagrelor (209 or 54.6%). Clopidogrel was more often administered in patients at increased ischemic and bleeding risk, while ticagrelor in those undergoing percutaneous coronary intervention. Mean DAPT duration was longer in the ticagrelor group. At 1 year, after multivariate adjustment, no difference in NACEs was observed between patients on clopidogrel versus ticagrelor (19% vs. 11%, adjusted hazard ratio 1.27 [95% CI 0.71–2.27], p = 0.429). Age, number of HBR criteria, and mean DAPT duration were independent predictors of NACEs. In a real-world registry of patients with acute coronary syndrome, 45% were at HBR and frequently treated with clopidogrel. After adjustment for potential confounders, the duration of DAPT, but not DAPT type (stratified by clopidogrel vs. ticagrelor), was associated with the risk of ischemic and bleeding events at 1 year.



Similar content being viewed by others
References
Valgimigli M, Bueno H, Byrne RA et al (2018) 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS. Eur Heart J 39:213–254
Neumann F-J, Sousa-Uva M, Ahlsson A et al (2018) 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J 40:87–165
Crisci M, Gragnano F, Di Maio M et al (2019) Improving adherence to Ticagrelor in patients after acute coronary syndrome: results from the PROGRESS trial. Curr Vasc Pharmacol 18:294–301
Wallentin L, Becker RC, Budaj A et al (2009) Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 361:1045–1057
Eikelboom JW, Mehta SR, Anand SS et al (2006) Adverse impact of bleeding on prognosis in patients with acute coronary syndromes. Circulation 114:774–782
Valgimigli M, Costa F, Lokhnygina Y et al (2017) Trade-off of myocardial infarction vs. bleeding types on mortality after acute coronary syndrome: lessons from the Thrombin Receptor Antagonist for Clinical Event Reduction in Acute Coronary Syndrome (TRACER) randomized trial. Eur Heart J 38:804–810
Urban P, Mehran R, Colleran R et al (2019) Defining high bleeding risk in patients undergoing percutaneous coronary intervention: a consensus document from the Academic Research Consortium for High Bleeding Risk. Eur Heart J 40:2632–2653
Ueki Y, Bär S, Losdat S, et al (2020) Validation of bleeding risk criteria (ARC-HBR) in patients undergoing percutaneous coronary intervention and comparison with contemporary bleeding risk scores. EuroIntervention EIJ-D-20-00052
Gragnano F, Cattano D, Calabrò P (2018) Perioperative care of cardiac patient’s candidate for non-cardiac surgery: a critical appraisal of emergent evidence and international guidelines. Intern Emerg Med 13:1185–1190
Prisco D (2018) A focus on direct oral anticoagulants: “old” and possible new indications and efforts for a better clinical management. Intern Emerg Med 13:985–988
Testa S, Ageno W, Antonucci E et al (2018) Management of major bleeding and outcomes in patients treated with direct oral anticoagulants: results from the START-Event registry. Intern Emerg Med 13:1051–1058
Alexopoulos D, Xanthopoulou I, Deftereos S et al (2016) Contemporary antiplatelet treatment in acute coronary syndrome patients undergoing percutaneous coronary intervention: 1-year outcomes from the GReek AntiPlatElet (GRAPE) Registry. J Thromb Haemost 14:1146–1154
Beigel R, Iakobishvili Z, Shlomo N et al (2017) Real-world use of novel P2Y12 inhibitors in patients with acute myocardial infarction: a treatment paradox. Cardiology 136:21–28
Sahlén A, Varenhorst C, Lagerqvist B et al (2016) Contemporary use of ticagrelor in patients with acute coronary syndrome: insights from Swedish web system for enhancement and development of evidence-based care in heart disease evaluated according to recommended therapies (SWEDEHEART). Eur Hear J Cardiovasc Pharmacother 2:5–12
Gragnano F, Fimiani F, Di Maio M et al (2019) Impact of lipoprotein(a) levels on recurrent cardiovascular events in patients with premature coronary artery disease. Intern Emerg Med 14:621–625
Patti G, Cavallari I, Antonucci E et al (2017) Prevalence and predictors of dual antiplatelet therapy prolongation beyond one year in patients with acute coronary syndrome. PLoS ONE 12:e0186961
Calabrò P, Moscarella E, Gragnano F et al (2019) Effect of body mass index on ischemic and bleeding events in patients presenting with acute coronary syndromes (from the START-ANTIPLATELET Registry). Am J Cardiol 124:1662–1668
Calabrò P, Gragnano F, Di Maio M et al (2018) Epidemiology and management of patients with acute coronary syndromes in contemporary real-world practice: evolving trends from the EYESHOT study to the START-ANTIPLATELET registry. Angiology 69:795–802
Costa F, van Klaveren D, James S et al (2017) Derivation and validation of the predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy (PRECISE-DAPT) score: a pooled analysis of individual-patient datasets from clinical trials. Lancet 389:1025–1034
Garcia-Garcia HM, McFadden EP, Farb A et al (2018) Standardized end point definitions for coronary intervention trials: the academic research consortium-2 consensus document. Circulation 137:2635–2650
Sacco RL, Kasner SE, Broderick JP et al (2013) An updated definition of stroke for the 21st century. Stroke 44:2064–2089
Jolly SS, Cairns JA, Yusuf S et al (2015) Randomized trial of primary PCI with or without routine manual thrombectomy. N Engl J Med 372:1389–1398
Zocca P, Van Der Heijden LC, Kok MM et al (2017) Clopidogrel or ticagrelor in acute coronary syndrome patients treated with newer-generation drug-eluting stents: CHANGE DAPT. EuroIntervention 13:1168–1176
Zocca P, Kok MM, van der Heijden LC et al (2018) High bleeding risk patients with acute coronary syndromes treated with contemporary drug-eluting stents and Clopidogrel or Ticagrelor: insights from CHANGE DAPT. Int J Cardiol 268:11–17
De Luca L, De Servi S, Musumeci G, Bolognese L (2018) Is ticagrelor safe in octogenarian patients with non-ST elevation acute coronary syndromes? Eur Heart J Cardiovasc Pharmacother 4:12–14
De Luca L, Zeymer U, Claeys MJ, et al (2020) Comparison of P2Y12 receptor inhibitors in patients with ST-elevation myocardial infarction in clinical practice: a propensity score analysis of five contemporary European registries. Eur Heart J Cardiovasc Pharmacother 22; pvaa002
Li L, Geraghty OC, Mehta Z, Rothwell PM (2017) Age-specific risks, severity, time course, and outcome of bleeding on long-term antiplatelet treatment after vascular events: a population-based cohort study. Lancet 390:490–499
Porta L, Baorda F, Fusco A, Gruppo di Autoformazione Metodologica (GrAM) (2018) Is proton pump inhibitors’ prophylaxis indicated for patients on antiplatelet therapy? Intern Emerg Med 13:585–587
Valgimigli M, Frigoli E, Leonardi S et al (2018) Radial versus femoral access and bivalirudin versus unfractionated heparin in invasively managed patients with acute coronary syndrome (MATRIX): final 1-year results of a multicentre, randomised controlled trial. Lancet 392:835–848
Bianchi R, D’Acierno L, Crisci M et al (2017) From femoral to radial approach in coronary intervention. Angiology 68:281–287
Gragnano F, Manavifar N, Gargiulo G et al (2019) Femoral access with or without vascular closure device or radial access in acute coronary syndrome. JACC Cardiovasc Interv 12:2116–2118
Gragnano F, Calabrò P, Valgimigli M (2019) Is triple antithrombotic therapy, or rather its duration and composition, the true culprit for the excess of bleeding events observed in patients with atrial fibrillation undergoing coronary intervention? Eur Heart J 40:216–217
Acknowledgements
The START-ANTIPLATELET Collaborators: Fabio Fimiani, Raffaella Antonia Vitale, Alessandra Schiavo, Marzia Conte, Dario Di Maio: Department of Translational Medical Sciences, University of Campania “Luigi Vanvitelli”, Naples, Italy; Daniele Pastori, Danilo Menichelli: I Clinica Medica, Atherothrombosis Centre, Department of Clinical Internal, Anesthesiologic, and Cardiovascular Sciences, Sapienza University of Rome, Rome, Italy; Guido Grossi, Luigi Di Serafino: Department of Experimental and Clinical Medicine, Center for Atherothrombotic diseases, University of Florence, Florence, Italy; Vittorio Taglialatela: Department of Advanced Biomedical Sciences, School of Medicine, “Federico II” University, Naples, Italy; Raffaele Galiero, Carlo Acierno: University of Campania “Luigi Vanvitelli” Department of Advanced Medical and Surgical Sciences; Maurizio del Pinto, Giuseppe Gugliemini: Department of Medicine, Division of Internal and Cardiovascular Medicine, University of Perugia, Perugia, Italy.
Funding
None.
Author information
Authors and Affiliations
Consortia
Contributions
FG and PC designed the work. FG and EM drafted the manuscript. FG, EM, PC, and PCP worked to the acquisition, analysis, and interpretation of data. All authors revised data critically for important intellectual content, approved the final version, and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
FG: Research grant from the European Society of Cardiology (ESC). GP: speaker/consultant/advisory board for Amgen, Sanofi, Bayer, Boehringer-Ingelheim, BMS-Pfizer, Daiichi Sankyo, Astra Zeneca, Sigma-Tau, Malesci, PIAM and MSD. IC: speaker for BMS-Pfizer, AstraZeneca, and Boeringher-Ingelheim. Other Authors have no conflicts of interest to disclose.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Statement of human and animal rights
The study protocol was approved by the local ethics committees and was conducted in accordance with the Declaration of Helsinki.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Informed consent was obtained from all individual participants included in the study.
Availability of data and material
All study data are available on request to the principal investigator.
Code availability
Statistical analysis plan and data analysis are available on request to the principal investigator.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The list of the START-ANTIPLATELET Collaborators are given in Acknowledgements.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gragnano, F., Moscarella, E., Calabrò, P. et al. Clopidogrel versus ticagrelor in high-bleeding risk patients presenting with acute coronary syndromes: insights from the multicenter START-ANTIPLATELET registry. Intern Emerg Med 16, 379–387 (2021). https://doi.org/10.1007/s11739-020-02404-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-020-02404-1