Abstract
A crucial element of any surgical training program is the ability to provide procedure-specific, objective, and reliable measures of performance. During robotic surgery, objective clinically relevant performance metrics (CRPMs) can provide tailored contextual feedback and correlate with clinical outcomes. This review aims to define CRPMs, assess their validity in robotic surgical training and compare CRPMs to existing measures of robotic performance. A systematic search of Medline and Embase databases was conducted in May 2022 following the PRISMA guidelines. The search terms included Clinically Relevant Performance Metrics (CRPMs) OR Clinically Relevant Outcome Measures (CROMs) AND robotic surgery. The study settings, speciality, operative context, study design, metric details, and validation status were extracted and analysed. The initial search yielded 116 citations, of which 6 were included. Citation searching identified 3 additional studies, resulting in 9 studies included in this review. Metrics were defined as CRPMs, CROMs, proficiency-based performance metrics and reference-procedure metrics which were developed using a modified Delphi methodology. All metrics underwent both contents and construct validation. Two studies found a strong correlation with GEARS but none correlated their metrics with patient outcome data. CRPMs are a validated and objective approach for assessing trainee proficiency. Evaluating CRPMs with other robotic-assessment tools will facilitate a multimodal metric evaluation approach to robotic surgery training. Further studies should assess the correlation with clinical outcomes. This review highlights there is significant scope for the development and validation of CRPMs to establish proficiency-based progression curricula that can be translated from a simulation setting into clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The need for high-quality robotic surgical training is becoming more relevant with the increasing uptake of robotic surgery across multiple specialities. A crucial element of any surgical training program is the ability to provide procedure-specific, objective, and reliable measures of performance [1]. Metric-based assessment in surgical training has been shown to improve trainee performance [1]. Proficiency-based training is a concept where trainees are given objective goals or benchmarks they are required to achieve at each level of surgical training, before progressing to the next [2]. It focuses on improving performance and maintaining the proficiency of that performance rather than relying on caseload as a representation of surgical skill [2]. It has been shown that this approach produces overall higher proficiency scores and reduced intra-operative complications in comparison to conventional operating-room training [3]. Hence, proficiency-based progression (PBP) training utilises simulation to allow trainees to achieve proficiency in a “risk-free environment” before operating on a patient and improve clinical outcomes [2]. However, to evaluate whether benchmarks have been achieved and provide feedback to trainees, surgical trainers require metrics to objectively assess performance [2]. Therefore, to meet the requirements of PBP training in robotic surgery, there is a need for validated metrics to provide tailored feedback and guide trainee progression.
Currently, automated performance metrics (APMs) are objective, reproducible measures derived from kinemetric data that assess surgical skill [4]. However, they are not readily available in live operating settings and thus lack translation from simulation to clinical contexts. Additionally, APMs rely on the availability of annotated datasets used to evaluate performance and the transferability of these datasets across various operating techniques, toolsets and procedures remain poor [5]. Similarly, several tools have been created and utilised to measure surgical proficiency during robotic surgery such as the Global Evaluative Assessment of Robotic Skills (GEARS). GEARS, though previously validated, provides overall proficiency feedback about robotic surgical skills by grading six domains without adapting them to be procedure specific [6,7,8]. It also remains reliant on assessor subjectivity and human rating which introduces the risk of bias [4]. Another tool, the Robotic Anastomosis Competency Evaluation (RACE), is a validated, objective scoring system to assess surgical performance during ureterovesical anastomosis (UVA) and provide structured feedback [9]. Whilst UVA is a critical step in surgical procedures, such as robot-assisted radical prostatectomy (RARP), it represents one task and not an entire procedure [9, 10]. Collectively, there is a need for clinically relevant objective metrics which can quantify a surgeon’s performance, provide feedback and ultimately improve both surgical and patient outcomes.
The idea of objective, clinically relevant metrics emerges with Clinically Relevant Performance Metrics (CRPMs) or Clinically Relevant Outcome Measures (CROMs) which have been explored to a limited degree in literature. CRPMs are applicable to a clinical context and can potentially correlate with patient outcomes. Specifically, they can inform trainee progression in the proctored operating phase of robotic training beyond simulation. In this review, we aimed to define CRPMs and assess their validity in robotic surgery training. As a secondary outcome, we aimed to compare the utility between CRPMs and existing measures of robotic performance, such as GEARS.
Methods
This review was registered in May 2022 (PROSPERO ID: CRD42022332901). A systematic search of Medline and Embase databases was conducted in May 2022 following the PRISMA guidlienes. The search terms used were Clinically Relevant Performance Metrics (CRPMs) OR Clinically Relevant Outcome Measures (CROMs) AND robotic surgery. Additional articles were obtained via citation searching of included publications. After the exclusion of duplicate articles, two independent reviewers (MY, GT) initially screened articles based on title and abstract. Selection was completed by screening full-text articles based on eligibility criteria. Conflicts were resolved by a senior third independent reviewer (KL).
Inclusion and exclusion criteria
The studies that were included addressed clinically relevant metrics including CRPMs, CROMs and clinically relevant metrics assessing intra-operative robotic performance. Studies assessing solely automated performance metrics (APMs), cognitive performance metrics (CPMs), patient-reported metrics or generalised measures of performance such as RACE, and GEARS were excluded. All settings of soft-tissue robot-assisted surgeries were included with dry laboratory, wet laboratory, animal models, and in-vivo operating. Articles addressing open surgery, laparoscopic surgery or not utilising a soft-tissue robot were excluded. Included studies investigated participants from multiple categories: surgeons (novice, experts), trainees (i.e. residents, interns), and medical students. Commentaries, conference abstracts, and reviews were excluded.
Data extraction
For the included articles, data were extracted including, authors, study objective, context (speciality and operation), study design (participants and robotic setting), metric details, measurement of metrics, metric validation status, and comparison outcome data to existing methods of assessment (RACE and GEARS).
Risk of assessment bias
A modified Newcastle–Ottawa scale was performed to assess the quality of included studies in this review (Appendix Table 3).
Results
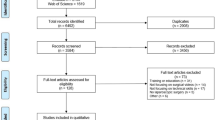
The initial database search yielded 116 articles with 75 unique articles remaining after the removal of duplicates. A further eight articles were retrieved through citation searching. After initial and full-text screening against eligibility criteria, nine studies were included in this review. Reasons for exclusion were the sole use of APMs, CPMs, subjective measures of performance, and utilising non-soft tissue robotics (see Fig. 1).
Individual study characteristics are summarised in Table 1. Included studies covered the specialities of urology (n = 5), coloproctology (n = 2), gastroenterology (n = 1) and the basic skills of robotic suturing and knot-tying (n = 1). Publication dates spanned the years 2017 to 2022. Together, their description of metrics included CRPMs, CROMs, PBP metrics, and reference-procedure metrics. Countries of publication included Germany [11, 12], England [13,14,15,16,17], and the USA [6, 18].
Definition of clinically relevant performance metrics
Throughout the articles, there was a lack of a clear consensus or homogenous definition for clinically relevant performance metrics in robotic surgery. As a result, this explicit terminology was utilised in only three of the included papers. Witthaus et al., introduced CRPMs as “concepts to design a conceptual framework for incorporating measures pertinent to a surgical task within a high-fidelity procedural simulation construct” [17]. Ghazi et al., defined CROMs as measures that “extend beyond basic robotic skills training into procedure-specific training” and provide tailored feedback to allow surgeons to progress based on individualised capabilities [15]. Ma et al., stated that CRPMs were those utilized to provide procedure-tailored feedback for surgical training and therefore “expedite the acquisition of robotic suturing skills” for each individual surgeon [18]. Other terminology utilised in the included publications were “procedure specific assessment tools” that provided an objective assessment of robotic intraoperative performance and enabled tailored training feedback to achieve competency [6, 12]. A further 4 articles used the term proficiency-based progression (PBP) metrics [11, 13, 14, 16].
Development of clinically relevant performance metrics
Individual details and the specific metrics assessed by each study are represented in Table 1. Witthaus et al., and Ghazi et al., took a similar approach in defining their metrics. They used hydrogel models in conjunction with the Da Vinci Surgical System to develop anatomically and mechanically validated simulation models [15, 17]. This enabled the incorporation of tailored clinically relevant performance metrics in training for nerve-sparing robot-assisted radical prostatectomy (NS-RARP) and Robot-assisted partial nephrectomy (RAPN). The metrics included: applied force to the neurovascular bundle during dissection, post-simulation margin status, UVA integrity, task-specific operating tasks, estimated blood loss [17] as well as console time, warm ischemia time (WIT), and positive surgical margins (PSMs) [15], respectively.
Methodology for developing clinically relevant metrics for UVA utilised pre-existing validated metrics including APMs and RACE score [18]. The remaining 6 articles used a modified Delphi process, to identify and describe specific metrics for a reference procedure. These reference procedures included RARP [6, 14], robot-assisted low anterior resection (RA-LAR) [13, 16], robotic suturing and knot tying anastomosis [12], and intestinal anastomosis [11]. To create the reference metrics, a modified Delphi methodology using a panel of experts, outlined a combination of domains, procedure phases, steps, errors and critical errors. The metrics were edited, and a level of consensus was established before the final metrics were voted upon and finalised [14]. This is the only example in the literature of a structured approach to the development of clinically relevant performance metrics.
Validation of clinically relevant performance metrics
Content validation
Content validity is defined as “the degree to which elements of an assessment instrument are relevant to a representative of the targeted construct for a particular assessment purpose” [19]. For clinically relevant metrics, this refers to how accurately they reflect performance in the clinical context they were intended to measure. CRPMs for NS-RARP were content validated by performing nerve sensor calibration, surgical margin verification and using the standard 180 ml UVA leak test [17]. An iterative development process was used to assess feedback and the feasibility of the CROMs in relation to the RAPN [15]. APMs related to UVA steps were collated from data from the Da Vinci robotic system, and combined with technical skill scores from RACE, which was previously validated [18]. Considering the articles that utilised a Delphi panel to create their reference metrics, content validation was achieved by voting upon each metric, and ensuring high-level consensus was achieved before the metrics were accepted and included as part of the finalised reference metrics [6, 11,12,13,14, 16]. Content validation measures for each study is represented in Table 2.
Construct validation (response process evidence)
Construct validation refers to the ability of CRPMs to differentiate between surgical skill, such as novices, intermediates and experts. All studies demonstrated that their metrics were able to distinguish between skill levels, though not all reached statistical significance (see Table 2).
Witthaus et al. showed that experts outperformed novices on all NS-RARP CRPMs including reduced nerve forces applied and total energy, superior margin results (p = 0.011), UVA integrity and all task-specific operating times except seminal vesicle dissection. Although not statistically significant, experts had a reduced EBL [17]. Similarly, Ghazi and colleagues demonstrated construct validity of their RAPN CROMs whereby experts significantly outperformed novices in all metrics, except for positive surgical margins [15]. Ma et al. found the feedback group, which received tailored feedback based on the CRPMs from UVA training tasks, outperformed the control group across all metrics except the needle entry score [18]. In addition to this, the effect size was measured to detect which metrics were more sensitive in detecting differences between the control and feedback group. For the UVA task, needle positioning, tissue approximation, and master clutch usage were found to have a higher effect size [18]. PACE was also found to have construct validity for RARP with the expert group outperforming the novices across all seven domains [6]. Puliatti et al. demonstrated construct validity for the reference approach to suturing and knot tying in anastomotic models, where novices had an increased mean task completion time, mean number of errors, and anastomotic leakage in comparison to experts [12]. Novices were also 12.5 times more likely to fail to progress throughout the task [12].
All the above studies used a caseload of procedures to differentiate between novice, intermediate and expert surgeons. Mottrie et al. and Gómez et al., however, found that within their expert surgeon groups, there existed two distinct populations: experienced surgeons with few errors and experienced surgeons with high errors [13, 14]. Those with the most errors demonstrated considerable performance variability, some performing worse than the weakest performing novice [13, 14]. To account for this variability, both studies considered two distinct populations. They found that experienced surgeons with the fewest errors performed significantly better across the metrics than those with high errors and novices, confirming construct validity [13, 14]. The neurovascular bundle dissection phase of the RARP and the rectal dissection in RA-LAR discriminated best between the total experienced surgeons and novices [13, 14]. Lastly, Schmidt et al. found that both the weighted and unweighted forms of the A-OSATS metric were unable to distinguish between surgical skill level according to caseload alone but achieved construct validity when participants were assigned to each skill level according to the OSATS global rating score (GRS) [11].
Criterion validity
Criterion validity refers to the relationship of CRPMs with other variables such as the validated semi-objective scoring systems, GEARS and RACE. Three studies examined the criterion validity of their metrics (Table 2). Witthaus et al. found that reduced force to neurovascular bundle during dissection correlated to higher force sensitivity (p = 0.019)) and total GEARS score (p = 0.000) [17]. UVA leak rate was also found to correlate with the total RACE score (p = 0.000) [17]. Ghazi and colleagues also found similar correlations between their CROMs and total GEARS score including console time, WIT, EBL and PSMs [15]. Gómez et al. found that GEARS had poor inter-rater reliability (IRR) for video scoring and weaker discrimination between surgical skill groups [13]. They concluded that PBP binary metrics demonstrated superior IRR than GEARS and robust discrimination amongst skill level, especially for total errors [13].
Clinical context
Schmidt et al. constructed weighted A-OSATS scores which highlighted steps pertinent for patient outcomes but did not explore its predictive capabilities in comparison to the unweighted score [11]. Collectively, no study investigated the correlation between clinically relevant performance metrics and patient outcomes, though was highlighted as a point for future research.
Discussion
Whilst the use of robotic surgery is increasing in clinical practice, training in robotic surgery and robotic skill assessments continue to require fundamental standardisation [20, 21]. For efficiency purposes, standardised robotic skill assessments should be readily available, operation-specific, objective and reproducible [20]. Having standardised and validated metrics is crucial for the development of safe proficiency-based robotic surgery training curricula [5]. In 2015, the first validated robotic training curriculum was developed which outlined training steps beginning with a baseline evaluation, simulation training, and observation of live operations [22]. This curriculum has not been tailored to specific operative procedures, and limitations include the inability to be objectively assessed, benchmarked and the lack of metrics for quality assurance [5]. Currently, metrics have been developed, such as automated performance metrics or semi-objective tools such as GEARS, that do provide overall robotic technical proficiency feedback, albeit lack transition to a clinical context. To investigate this current deficiency in standardised performance metrics, this review presents the findings of clinically relevant performance metrics with promising validity and the ability to provide tailored feedback.
It has become apparent that CRPMs lack a clear definition. Throughout this review, an emerging pattern of terminology associated with CRPMs or CROMs has emerged including objective assessment, proficiency-based progression, context-specific performance, competency training and tailored intra-operative feedback. Hence, we suggest that CRPMs can be defined as “context-specific metrics that objectively assess proficiency in robotic surgery training and provide tailored surgical feedback”.
Standardisation of robotic surgery training with objective performance metrics will allow easier detection of sub-optimised technique. This could translate to earlier post-operative complication detection and improved patient outcomes [5, 23, 24]. Given the heterogeneous development of CRPMs, it is important to identify which method is the most efficient and objective whilst still maintaining validity. Metrics that were identified in the review can be classified and divided into two groups: those that were procedure-specific or those that are generalisable to any operative procedure. Metrics identified as generalisable included applied force, post-simulation margin status, estimated blood loss, APMs, total console time/task completion time, warm ischemia time, and needle/suture breakage which constituted the CRPMs described by three studies [15, 17, 18]. It is not yet clear how performance differs with general versus specific procedure-based metric feedback. Given the aim of proficiency-based training it would be ideal to incorporate these clinically relevant metrics into a standard procedural description that can objectively assess both general and procedure-specific skills.
Proficiency based performance (PBP) metrics are defined as “objective and validated performance metrics to track progression of the trainee and operative skill on a specific task or procedure” and “allows learners to progress in their training based on their proficiency, rather than the number of cases performed or duration of practice” [13, 14, 16]. Four of the studies presented in this review used “PBP metrics” with enabled the development of reference metrics covering all domains of a surgical procedure and were found to have content and construct validity [11, 13, 14, 16]. An important element of PBP is sustained deliberate practice (SDP) which is the process of continuous training and repetition of robotic surgical skills that are both defined and assessed by PBP metrics [5, 25]. SDP has been shown to reduce error rates by 50% during robotic surgery training [25]. However, SDP requires the skills to be outlined by CRPMs that are agreed upon by the trainer and trainee in order for skill learning to be efficient [26]. From the studies presented, it appears the optimal way to ensure consensus and content validation of metrics is by using a modified Delphi methodology for procedure deconstruction, development of a standardised procedural description and identification of specific procedural phases, steps, and critical errors. Once reference PBP metrics have been produced via Delphi methodology, the development of simulation models that reflect the metrics can be created. As a result, SDP can be established through the continuum of proficiency-based training [5]. This is highlighted by Puliatti and Schmidt et al., using animal simulation models reflecting their suturing and knot tying reference metrics and A-OSATS metrics, respectively [11, 12].
Robotic surgery simulation using 3D models enables higher reproducibility of relevant anatomy and physiology of specific operative procedures in comparison to other models [5]. These 3D models enable the incorporation of CRPMs, a chance for improved SDP and proficiency-based training, as well as a smoother transition from simulation to a live-operating context [5]. Novel 3D simulation models are cost-effective as they do not need wet-lab facilities and are also more accessible for training in comparison to attending live surgeries. These 3D models can support SDP across various settings and enable real-time feedback that can be tailored to trainee performance [5]. Both Witthaus et al. and Ghazi et al. used 3D PVA hydrogel models to reflect NS-RARP and RAPN procedures, respectively. However, the CRPMs they incorporated were more generalised and could benefit by introducing PBP reference metrics deconstructing the crucial steps, and errors of each operation using a Delphi methodology [15, 17]. Promoting robotic surgery simulation training and preventing trainees that are early on their learning curve being exposed to patient surgeries, can result in a “reduction of surgical errors leading to an overall decrease in prolonged surgeries, and serious patient injury or death”, as defined by the ECRI institute [27]. Collectively, from the current data presented, using the Delphi methodology to develop CRPMs to aid in proficiency-based progression and incorporating CRPMs into novel full-immersion simulation using 3D printed models, represents the most standardised process of assessing proficiency in robotic surgery training. The CRPMs can then be translated for use in clinical contexts, standardising surgical assessment from simulation to live operations. In turn, this provides a structured methodology for developing future robotic surgery training curricula, tailored for different operative contexts.
The secondary aim of this review was to compare the utility of CRPMs to existing measures of performance, such as the semi-objective GEARS tool. It has been found that despite its ready use in robotic surgery training, low IRR for GEARS assessment has begun to appear in literature [13, 28]. In this review, it was highlighted that GEARS had poor inter-rater reliability for video scoring and weaker discrimination between surgical skill groups in comparison to PBP binary metrics which demonstrated good IRR and robust discrimination amongst skill level. This supports the view that PBP metrics may represent a more efficient, and objective tool than GEARS in assessing surgical skill throughout robotic surgical training. Supporting these findings, Satava and colleagues found that binary PBP metrics were superior in assessing “quality of assessment” in comparison to using a Likert scale such as GEARS for robotic surgery training of basic skills [29]. However, due to the lack of a “gold standard” robotic surgery training method, it is necessary to evaluate novel CRPMS in relation to existing measures of performance that are being developed currently, not exclusively GEARS. A cross-method validity may be a viable option to infer the relative utility of novel robotic surgery metrics [30]. For example, a study by Hung and colleagues found a strong correlation between APMs and GEARS during RARP though stressed that a lack of statistical correlation between the two did not suggest superiority of either metric [31]. They suggested that refined clinical metrics correlated to clinical outcomes could help delineate superiority [31].
Limitations
This review aimed to evaluate the current use of CRPMs for robotic surgery training. A possible limitation is the utilisation of a single mode of metric evaluation narrows the available scope of feedback for trainees. Other forms of performance metrics exist including cognitive performance metrics, eye-tracking metrics and even APMs, that were not explored in this review. Ideally, all these metrics can be evaluated on their use in conjunction with one another, to determine if a synergistic effect exists in optimising trainee performance and translation to a clinical context. Future studies can explore a multimodal metric evaluation in simulation as well as in-vivo training in robotic surgery and its association with progression trainee performance.
Despite exploring CRPMs in this review, they have not been translated to a clinical context as they were indented. Patient outcome data has, however, been explored by Hung and colleagues in relation to APM’s and their correlation with early urinary continence after RARP [32]. They found that whilst clinical factors confounded patient outcome data, specific surgeon kinematic metrics including velocity and wrist articulation served as independent predicators of urinary continence after RARP. However, this research came after the extensive development and validation of APM’s for RARP [33]. Likewise, studies in this review are in the early stages of optimising their CRPMs and hope to explore the relation of their metrics to patient outcomes in a future study. In general, it has been found that skill level, rather than caseload, is a better predictor of both intra-operative performance and clinical outcome [13, 34, 35]. Therefore, future studies exploring construct-validated CRPMs and their association with clinical outcomes is promising.
Finally, the studies in this review were limited by small sample sizes and reduced power. The modified NOS scale for non-randomised studies identified two good-quality studies [15, 18], with the remaining seven being of poor quality. Most studies in this review were prospective cohort studies except for one unblinded randomised control trial by Ma et al. [18]. Future studies incorporating the validated CRPMS presented here will benefit from larger sample sizes to detect power and randomised controlled trials to build high-quality validity evidence for this approach.
Conclusion
This study highlights the described clinically relevant performance metrics in the setting of robotic surgery. There is significant scope for the development and validation of clinically relevant metrics in this context. Clinically relevant performance metrics can assist in the development of proficiency-based progression curricula that can be carried across from a simulation setting into clinical practice.
Data availability
The material in the manuscript is the original work of the authors and has not been presented or submitted elsewhere for publication.
References
Mazzone E, Puliatti S, Amato M, Bunting B, Rocco B, Montorsi F et al (2021) A systematic review and meta-analysis on the impact of proficiency-based progression simulation training on performance outcomes. Ann Surg 274(2):281–289
Gallagher AG, Ritter EM, Champion H, Higgins G, Fried MP, Moses G et al (2005) Virtual reality simulation for the operating room: proficiency-based training as a paradigm shift in surgical skills training. Ann Surg 241(2):364–372
Aydın A, Ahmed K, Abe T, Raison N, Van Hemelrijck M, Garmo H et al (2022) Effect of simulation-based training on surgical proficiency and patient outcomes: a randomised controlled clinical and educational trial. Eur Urol 81(4):385–393
Guerin S, Huaulme A, Lavoue V, Jannin P, Timoh KN (2022) Review of automated performance metrics to assess surgical technical skills in robot-assisted laparoscopy. Surg Endosc 36(2):853–870
Chen IA, Ghazi A, Sridhar A, Stoyanov D, Slack M, Kelly JD et al (2021) Evolving robotic surgery training and improving patient safety, with the integration of novel technologies. World J Urol 39(8):2883–2893
Hussein AA, Ghani KR, Peabody J, Sarle R, Abaza R, Eun D et al (2017) Development and validation of an objective scoring tool for robot-assisted radical prostatectomy: prostatectomy assessment and competency evaluation. J Urol 197(5):1237–1244
Vassiliou MC, Feldman LS, Andrew CG, Bergman S, Leffondré K, Stanbridge D et al (2005) A global assessment tool for evaluation of intraoperative laparoscopic skills. Am J Surg 190(1):107–113
Goh AC, Goldfarb DW, Sander JC, Miles BJ, Dunkin BJ (2012) Global evaluative assessment of robotic skills: validation of a clinical assessment tool to measure robotic surgical skills. J Urol 187(1):247–252
Khan H, Kozlowski JD, Hussein AA, Sharif M, Ahmed Y, May P et al (2018) Use of Robotic Anastomosis Competency Evaluation (RACE) for assessment of surgical competency during urethrovesical anastomosis. Can Urol Assoc J 13(1):E10–E16
Raza SJ, Field E, Jay C, Eun D, Fumo M, Hu JC et al (2015) Surgical competency for urethrovesical anastomosis during robot-assisted radical prostatectomy: development and validation of the robotic anastomosis competency evaluation. Urology 85(1):27–32
Schmidt MW, Haney CM, Kowalewski KF, Bintintan VV, Abu Hilal M, Arezzo A et al (2022) Development and validity evidence of an objective structured assessment of technical skills score for minimally invasive linear-stapled, hand-sewn intestinal anastomoses: the A-OSATS score. Surg Endosc 36(6):4529–4541
Puliatti S, Mazzone E, Amato M, De Groote R, Mottrie A, Gallagher AG (2021) Development and validation of the objective assessment of robotic suturing and knot tying skills for chicken anastomotic model. Surg Endosc 35(8):4285–4294
Gómez Ruiz M, Tou S, Gallagher AG, Cagigas Fernández C, Cristobal Poch L, Matzel KE (2022) Intraoperative robotic-assisted low anterior rectal resection performance assessment using procedure-specific binary metrics and a global rating scale. BJS Open 6(3):zrac041
Mottrie A, Mazzone E, Wiklund P, Graefen M, Collins JW, De Groote R et al (2021) Objective assessment of intraoperative skills for robot-assisted radical prostatectomy (RARP): results from the ERUS Scientific and Educational Working Groups Metrics Initiative. BJU Int 128(1):103–111
Ghazi A, Melnyk R, Hung AJ, Collins J, Ertefaie A, Saba P et al (2021) Multi-institutional validation of a perfused robot-assisted partial nephrectomy procedural simulation platform utilizing clinically relevant objective metrics of simulators (CROMS). BJU Int 127(6):645–653
Tou S, Gomez Ruiz M, Gallagher AG, Matzel KE, collaborative EA (2020) European expert consensus on a structured approach to training robotic-assisted low anterior resection using performance metrics. Colorectal Dis 22(12):2232–2242
Witthaus MW, Farooq S, Melnyk R, Campbell T, Saba P, Mathews E et al (2020) Incorporation and validation of clinically relevant performance metrics of simulation (CRPMS) into a novel full-immersion simulation platform for nerve-sparing robot-assisted radical prostatectomy (NS-RARP) utilizing three-dimensional printing and hydrogel casting technology. BJU Int 125(2):322–332
Ma R, Lee RS, Nguyen JH, Cowan A, Haque TF, You J, et al (2022) Tailored feedback based on clinically relevant performance metrics expedites the acquisition of robotic suturing skills-an unblinded pilot randomized controlled trial. J Urol 101097JU0000000000002691
Rossiter JR (2008) Content validity of measures of abstract constructs in management and organizational research. Br J Manag 19(4):380–388
Kutana S, Bitner DP, Addison P, Chung PJ, Talamini MA, Filicori F (2022) Objective assessment of robotic surgical skills: review of literature and future directions. Surg Endosc 36(6):3698–3707
Talamini MA, Chapman S, Horgan S, Melvin WS (2003) A prospective analysis of 211 robotic-assisted surgical procedures. Surg Endosc 17(10):1521–1524
Volpe A, Ahmed K, Dasgupta P, Ficarra V, Novara G, van der Poel H et al (2015) Pilot validation study of the European association of urology robotic training curriculum. Eur Urol 68(2):292–299
Collins JW, Tyritzis S, Nyberg T, Schumacher M, Laurin O, Khazaeli D et al (2013) Robot-assisted radical cystectomy: description of an evolved approach to radical cystectomy. Eur Urol 64(4):654–663
Schlomm T, Heinzer H, Steuber T, Salomon G, Engel O, Michl U et al (2011) Full functional-length urethral sphincter preservation during radical prostatectomy. Eur Urol 60(2):320–329
Angelo RL, Ryu RK, Pedowitz RA, Beach W, Burns J, Dodds J et al (2015) A proficiency-based progression training curriculum coupled with a model simulator results in the acquisition of a superior arthroscopic Bankart skill set. Arthroscopy 31(10):1854–1871
Ericsson KA, Harwell KW (2019) Deliberate practice and proposed limits on the effects of practice on the acquisition of expert performance: why the original definition matters and recommendations for future research. Front Psychol 10:2396
Institue E (2014) Top 10 health technology hazards for 2015. Health Devices 1:3–6
Satava RM, Stefanidis D, Levy JS, Smith R, Martin JR, Monfared S et al (2020) Proving the effectiveness of the Fundamentals of Robotic Surgery (FRS) skills curriculum: a single-blinded, multispecialty multi-institutional randomized control. Trial Ann Surg 272(2):384–392
Satava R, Gallagher AG (2020) Proficiency-based progression process training for fundamentals of robotic surgery curriculum development. Ann Laparosc Endosc Surg 5:14
Hung AJ, Jayaratna IS, Teruya K, Desai MM, Gill IS, Goh AC (2013) Comparative assessment of three standardized robotic surgery training methods. BJU Int 112(6):864–871
Hung A, Chen J, Jarc A, Gill I, Djaladat H (2017) Concurrent validation of automated evaluation of robotic surgery performance: correlation of performance metrics to global evaluative assessment of robotic surgery (GEARS). J Urol 197(4 Supplement 1):e693
Hung AJ, Ma R, Cen S, Nguyen JH, Lei X, Wagner C (2021) Surgeon automated performance metrics as predictors of early urinary continence recovery after robotic radical prostatectomy—a prospective bi-institutional study. Eur Urol Open Sci 27:65–72
Hung AJ, Chen J, Jarc A, Hatcher D, Djaladat H, Gill IS (2018) Development and validation of objective performance metrics for robot-assisted radical prostatectomy: a pilot study. J Urol 199(1):296–304
Birkmeyer JD, Finks JF, O’Reilly A, Oerline M, Carlin AM, Nunn AR et al (2013) Surgical skill and complication rates after bariatric surgery. N Engl J Med 369(15):1434–1442
Curtis NJ, Foster JD, Miskovic D, Brown CSB, Hewett PJ, Abbott S et al (2020) Association of surgical skill assessment with clinical outcomes in cancer surgery. JAMA Surg 155(7):590–598
Acknowledgements
KL would like to acknowledge the financial support of the Australian Government through the professional practice research training scholarship program.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. No other funding was received for the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. M.Y. and K.L. wrote the manuscript text and M.Y. prepared figure 1 and tables 1-2. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript
Corresponding author
Ethics declarations
Conflict of interest
The authors of this manuscript have no significant conflict of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Younes, M.M., Larkins, K., To, G. et al. What are clinically relevant performance metrics in robotic surgery? A systematic review of the literature. J Robotic Surg 17, 335–350 (2023). https://doi.org/10.1007/s11701-022-01457-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-022-01457-y