Abstract
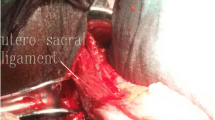
This video’s objective was to describe our spiral technique and surgical steps of robotic-assisted laparoscopic apical suspension (RALAS) in the treatment of patients with symptomatic apical vaginal prolapse. A 70-year-old Caucasian woman, gravida 3, para 2 had symptomatic pelvic organ prolapse (POP) apical/anterior stage III. At pelvic ultrasound evaluation, the uterus was small and normal appearing of adnexa bilaterally. She failed pessaries and is sexually active. The most relevant complaints were vaginal bulging and pressure. She denied urinary incontinence. During the surgery, we used (1) 3-0, V-Loc™ (Covidien) and we reinforced these absorbable sutures with (2) 2-0, GORE-TEX® Suture (Gore Medical). The Si da Vinci Surgical System was used with 4 arms and 5 trocars configuration, docked on the patient’s left side. On the right/left apical support, we used V-Loc and Gore-Tex and these provided the initial 2 points suspension on the uterosacral ligaments (USL). We like to attach the left to the right USL. We then developed the space between the bladder and vagina and proceed with a plication of the pubocervical fascia with V-loc sutures. Two anterior apical support sutures were taken from the vagina to the transversalis fascia on the anterior abdominal wall and then hid behind the bladder peritoneum. The tension of these sutures was maintained with Hem-o-lock (TeleFlex) and LAPRA-TY (Ethicon). With the spiral technique, we secured these sutures through aponeurosis of abdominal muscle inside-outside-inside using a Carter-Thomason (Cooper Surgical) laparoscopic port closure system. This technique may provide a better long-term support for the anterior apical compartment.


Similar content being viewed by others
References
Gerten KA, Markland AD, Lloyd LK et al (2008) Prolapse and incontinence surgery in older women. J Urol 179(6):2111–2118
Division of Small Manufacturers, International and Consumer Assistance (DSMICA) (2011) Update on serious complications associated with transvaginal placement of surgical mesh for pelvic organ prolapse: FDA safety communication [Internet]. Silver Spring (MD, USA). US Food and Drug Administration; Jul 13 [cited 2015 Nov 9]. http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm262435.htm
Sedrakyan A, Chughtai B, Mao J (2016) Regulatory warnings and use of surgical mesh in pelvic organ prolapse. JAMA Intern Med [Internet]. [cited 2017 May 6];176(2):275–277. http://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2475021
Cosson M, Rajabally R, Bogaert E, Querleu D, Crepin G (2002) Laparoscopic sacrocolpopexy, hysterectomy, and burch colposuspension: feasibility and short-term complications of 77 procedures. JSLS 6:115–119
Nezhat CH, Nezhat F, Nezhat C (1994) Laparoscopic sacral colpopexy for vaginal vault prolapse. Obstet Gynecol 84:885–888
Ostrzenski A (1996) Laparoscopic colposuspension for total vaginal prolapse. Int J Gynaecol Obstet 55:147–152
Nygaard IE, McCreery R, Brubaker L, Connolly AM, Cundiff G, Weber AM et al (2004) Abdominal sacrocolpopexy: a comprehensive review. Obstet Gynecol 104:805–823
Serati M, Bogani G, Sorice P, Braga A, Torella M, Salvatore S, Uccella S, Cromi A, Ghezzi F (2014 Aug) Robot-assisted sacrocolpopexy for pelvic organ prolapse: a systematic review and meta-analysis of comparative studies. Eur Urol 66(2):303–318
Nygaard IE, McCreery R, Brubaker L et al (2004) Pelvic floor disorders network. abdominal sacrocolpopexy: a comprehensive review. Obstet Gynecol 104(4):805–823
Davila HH, Gallo T, Bruce L, Landrey C (2016) Robotic and laparoendoscopic single-site utero-sacral ligament suspension for apical vaginal prolapse: evaluation of our technique and perioperative outcomes. J Robot Surg 11:171–177
Davila HH, Bruce L, Goodman L, Gallo T (2017) Robotic assisted laparoscopic apical suspension. Description of a 4 points technique (RALAS-4): first case reported. Open J Obstetr Gynecol 7:944–950. https://doi.org/10.4236/ojog.2017.79095
Jelovsek JE, Barber MD, Brubaker L, Norton P, Gantz M, Richter HE, Weidner A, Menefee S, Schaffer J, Pugh N, Meikle S; NICHD Pelvic Floor Disorders Network (2018) Effect of uterosacral ligament suspension vs sacrospinous ligament fixation with or without perioperative behavioral therapy for pelvic organ vaginal prolapse on surgical outcomes and prolapse symptoms at 5 years in the OPTIMAL Randomized Clinical Trial. JAMA 319(15):1554–1565. https://doi.org/10.1001/jama.2018.2827
DeLancey JO (1992) Anatomic aspects of vaginal eversion after hysterectomy. Am J Obstet Gynecol 166(6 Pt 1):1717–1784
Blaisdell FE (1917) The anatomy of the sacro-uterine ligaments. Anat Rec 12:1–42
Petros PE, Ulmsten U (1990) An integral theory of female urinary incontinence. Acta Obstet Gynecol Scand 69(Suppl 153):7–31
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Hugo H Davila, MD, Karisa Brown MS, Prajwal Dara MS, Lindsey Bruce MD, Lindsey Goodman MD and Taryn Gallo MD. Declare that they have no conflict of interest.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Consent section
Written informed consent was obtained from the patient for publication of this Case Report/any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Video. Robotic-Assisted Laparoscopic Apical Suspension with spiral technique (RALAS-4 s). Descriptions of surgical steps (MP4 353885 KB)
Rights and permissions
About this article
Cite this article
Davila, H.H., Brown, K., Dara, P. et al. Robotic-assisted laparoscopic apical suspension: description of the spiral technique. J Robotic Surg 13, 519–523 (2019). https://doi.org/10.1007/s11701-018-0879-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-018-0879-1