Abstract
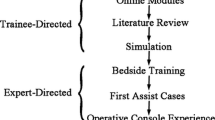
Robotic surgery is experiencing a rapidly-increasing presence in the field of general surgery. The adoption of any new technology carries the challenge of training current and future surgeons in a safe and effective manner. We report our experience with the initiation of a robotic general surgery program at an academic institution while simultaneously incorporating surgical trainees. The initial procedure performed was robotic-assisted cholecystectomy (RAC). Concurrent with the introduction of a robotic general surgical program, our institution implemented a progressive surgical trainee curriculum for all active residents and fellows. Immediately after being credentialed to perform RAC, attending surgeons began incorporating surgical trainees into robotic procedures. We retrospectively reviewed our first 50 RACs and compared them with our previous 50 standard laparoscopic cholecystectomies (SLC) to determine the impact of rapid integration of surgical trainees on developing technologies. Despite new technology and novice surgeons, there was no difference in mean operative time between the SLC and RAC groups (75.3 vs. 84.1 min, p = 0.077). Two patients in the robotic-assisted group required intraoperative conversion. Hospital length of stay was similar between groups, with the majority of patients leaving the same day. There were no postoperative complications in either group. A robotic general surgery program can be initiated while concurrently instructing surgical trainees on robotic surgery in a safe and efficient manner. We report our initial experience with the adoption of this rapidly advancing technology and describe our training model.

Similar content being viewed by others
References
Martin RC 2nd, Kehdy FJ, Allen JW (2005) Formal training in advanced surgical technologies enhances the surgical residency. Am J Surg 190(2):244–248
Escarce JJ (1996) Externalities in hospitals and physician adoption of a new surgical technology: an exploratory analysis. J Health Econ 15(6):715–734
Haluck RS, Krummel TM (2000) Computers and virtual reality for surgical education in the 21st century. Arch Surg 135(7):786–792
Grantcharov TP, Reznick RK (2009) Training tomorrow’s surgeons: what are we looking for and how can we achieve it? ANZ J Surg 79(3):104–107. doi:10.1111/j.1445-2197.2008.04823.x
Philibert I, Friedmann P, Williams WT, ACGME Work Group on Resident Duty Hours, Accreditation Council for Graduate Medical Education (2002) New requirements for resident duty hours. JAMA 288(9):1112–1114
Wilson EB (2009) The evolution of robotic general surgery. Scand J Surg 98(2):125–129
Menon M, Shrivastava A, Tewari A, Sarle R, Hemal A, Peabody JO, Vallancien G (2002) Laparoscopic and robot assisted radical prostatectomy: establishment of a structured program and preliminary analysis of outcomes. J Urol 168(3):945–949
Ferguson JL, Beste TM, Nelson KH, Daucher JA (2004) Making the transition from standard gynecologic laparoscopy to robotic laparoscopy. JSLS 8(4):326–328
Beste TM, Nelson KH, Daucher JA (2005) Total laparoscopic hysterectomy utilizing a robotic surgical system. JSLS 9(1):13–15
Hanly EJ, Talamini MA (2004) Robotic abdominal surgery. Am J Surg 188(4A Suppl):19S–26S
Liss MA, Abdelshehid C, Quach S, Lusch A, Graversen J, Landman J, McDougall EM (2012) Validation, correlation, and comparison of the da Vinci trainer(™) and the daVinci surgical skills simulator(™) using the Mimic(™) software for urologic robotic surgical education. J Endourol 26(12):1629–1634. doi:10.1089/end 2012.0328
Finnegan KT, Meraney AM, Staff I, Shichman SJ (2012) da Vinci Skills Simulator construct validation study: correlation of prior robotic experience with overall score and time score simulator performance. Urology 80(2):330–335. doi:10.1016/j.urology.2012.02.059
Kelly DC, Margules AC, Kundavaram CR, Narins H, Gomella LG, Trabulsi EJ, Lallas CD (2012) Face, content, and construct validation of the Da Vinci Skills Simulator. Urology 79(5):1068–1072. doi:10.1016/j.urology.2012.01.028
Rosser JC Jr, Murayama M, Gabriel NH (2000) Minimally invasive surgical training solutions for the twenty-first century. Surg Clin North Am 80(5):1607–1624
Hashimoto DA, Gomez ED, Danzer E, Edelson PK, Morris JB, Williams NN, Dumon KR (2012) Intraoperative resident education for robotic laparoscopic gastric banding surgery: a pilot study on the safety of stepwise education. J Am Coll Surg 214(6):990–996. doi:10.1016/j.jamcollsurg.2012.02.001
Seamon LG, Fowler JM, Richardson DL, Carlson MJ, Valmadre S, Phillips GS, Cohn DE (2009) A detailed analysis of the learning curve: robotic hysterectomy and pelvic-aortic lymphadenectomy for endometrial cancer. Gynecol Oncol 114(2):162–167. doi:10.1016/j.ygyno.2009.04.017
Vidovszky TJ, Smith W, Ghosh J, Ali MR (2006) Robotic cholecystectomy: learning curve, advantages, and limitations. J Surg Res 136(2):172–178
Stegemann AP, Ahmed K, Syed JR, Rehman S, Ghani K, Autorino R, Sharif M, Rao A, Shi Y, Wilding GE, Hassett JM, Chowriappa A, Kesavadas T, Peabody JO, Menon M, Kaouk J, Guru KA (2013) Fundamental skills of robotic surgery: a multi-institutional randomized controlled trial for validation of a simulation-based curriculum. Urology 81(4):767–774. doi:10.1016/j.urology.2012.12.033
Conflict of interest
Ryan M. Juza, Randy S. Haluck, Eugene J. Won, Laura M. Enomoto, Ann M. Rogers, Vinay Singhal, Tung Tran, Stephanie Estes, and Jerome R. Lyn-Sue declare that they have no conflicts of interest. Eric M. Pauli is a compensated speaker for Bard, Synthes, and Synapse corporations. This work was not supported by any industry funding.
Ethical standard
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5).
Informed consent
Informed consent was obtained from all patients for being included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Juza, R.M., Haluck, R.S., Won, E.J. et al. Training current and future robotic surgeons simultaneously: initial experiences with safety and efficiency. J Robotic Surg 8, 227–231 (2014). https://doi.org/10.1007/s11701-014-0455-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-014-0455-2