Abstract
Introductions
Revision surgery because of weight recurrence is performed in 2.5–33% of primary vertical banded gastroplasty (VBG), laparoscopic sleeve gastrectomy (LSG), and gastric band (GB) cases. These cases qualify for revisional Roux-en-Y gastric bypass (RRYGB).
Methods
This retrospective cohort study analyzed data from 2008 to 2019. A stratification analysis and multivariate logistic regression for prediction modeling compared the possibility of sufficient % excess weight loss (%EWL) ≥ 50 or insufficient %EWL < 50 between three different RRYGB procedures, with primary Roux-en-Y gastric bypass (PRYGB) as the control during 2 years of follow-up. A narrative review was conducted to test the presence of prediction models in the literature and their internal and external validity.
Results
A total of 558 patients underwent PRYGB, and 338 underwent RRYGB after VBG, LSG, and GB, and completed 2 years of follow-up. Overall, 32.2% of patients after RRYGB had a sufficient %EWL ≥ 50 after 2 years, compared to 71.3% after PRYGB (p ≤ 0.001). The total %EWL after the revision surgeries for VBG, LSG, and GB was 68.5%, 74.2%, and 64.1%, respectively (p ≤ 0.001). After correcting for confounding factors, the baseline odds ratio (OR) or sufficient %EWL ≥ 50 after PRYGB, LSG, VBG, and GB was 2.4, 1.45, 0.29, and 0.32, respectively (p ≤ 0.001). Age was the only significant variable in the prediction model (p = 0.0016). It was impossible to develop a validated model after revision surgery because of the differences between stratification and the prediction model. The narrative review showed only 10.2% presence of validation in the prediction models, and 52.5% had external validation.
Conclusion
Overall, 32.2% of all patients after revisional surgery had a sufficient %EWL ≥ 50 after 2 years, compared to PRYGB. LSG had the best outcome in the revisional surgery group in the sufficient %EWL group and the best outcome in the insufficient %EWL group. The skewness between the prediction model and stratification resulted in a partially non-functional prediction model.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric metabolic surgery (BMS) is an efficient procedure that can result in considerable sustained weight loss (WL) in patients with obesity, resolve medical problems associated with obesity, and improve quality of life [1]. The long-term health effects are essential for good outcomes in BMS [2, 3]. Unfortunately, weight recurrence occurs between 18 and 24 months after surgery in 30% of patients [4]. The rate of conversion due to insufficient WL or weight recurrence is between 2.5 and 33% after primary vertical banded gastroplasty (VBG), laparoscopic sleeve gastrectomy (LSG), and gastric band (GB) procedures [5,6,7].
Revisional Roux-en-Y gastric bypass (RRYGB) is commonly employed to revise bariatric procedures because it can effectively manage weight recurrence and obstructive complications [8,9,10,11,12].
Primary Roux-en-Y gastric bypass (PRYGB) and primary VBG, LSG, or GB are different techniques. RYGB is a mixed procedure with restrictive and malabsorptive functions, whereas VBG, LSG, and GB are primarily restrictive procedures. All these procedures also involve changes to the gut hormones and microbiomes [13,14,15].
Generally, the outcome of results analyses can provide an overestimation or underestimation of the treatment effect. One solution to correct or test for this is stratification analysis, which is defined as sorting data into distinct groups or layers and creating multiple subgroups. Thus, confounding of interest can be defined and corrected, and a more realistic outcome can be presented. Stratification has become an increasingly popular approach [16]. Reflecting this technique on BMS, comparing different surgical techniques and testing the groups within and between each other based on stratified outcomes is more interesting than analyzing different surgeries in the same single revision group.
This study aimed to test how well stratification outcomes compared to unstratified outcome results in a stratified revisional surgery group in combination with testing a prediction model and comparing them with PRYGB as a control to understand the treatment effect and identify the predictive value.
In addition, we tested the presence of prediction models and validation status in the literature by searching for (revisional) BMS models and conducting a narrative review of the presence of prediction models and their associated internal and external validity.
Methods
This retrospective study on stratification and predictive variables of sufficient %EWL between PRYGB and RRYGB weight recurrence in VBG, GB, and LSG surgery was conducted with patients who completed a 2-year follow-up between 2008 and 2019 at Madina Women’s Hospital and Medical Research Institute, Alexandria University, Alexandria, Egypt, and Ain shams University, Cairo, Egypt. The study was approved by the appropriate ethics committee and was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki. All patients provided informed consent for the data to be used for research publication.
Patient Selection
Two groups were defined as responders or non-responders to WL after PRYGB and RRYGB according to %EWL ≥ 50 and %EWL < 50, respectively [17].
%EWL was calculated using the formula: %EWL = (initial body weight − current body weight) / (initial body weight − ideal body weight) × 100% (in which ideal body weight is defined by the weight corresponding to a BMI of 25 kg/m2).
Percentage total weight loss (%TWL) was calculated using the formula: %TWL = ((initial body weight − current body weight) / initial body weight) × 100%.
Study Endpoints
First, testing the differences in stratification and unstratified outcome results in different revisional surgery groups. In addition, prediction models were built and tested using the stratified outcomes. All were compared with PRYGB as the control to understand the treatment effect and identify predictive values.
Second, conducting a narrative review of the presence of prediction models and validation status in the BMS field literature.
Data Collection
The analyzed data included demographic characteristics and associated medical conditions, laboratory investigations, preoperative workups, postoperative follow-ups, and time between surgeries.
Body mass index (BMI), nadir BMI, pre-revision BMI, %EWL, %TWL, percentage of excess BMI loss (%EBMIL) after primary surgery, BMI 3 months post-revision in the RRYGB group, as well as BMI, %EWL, %TWL, and %EBMIL 2 years after surgery for PRYGB were measured in the RRYGB group.
Surgical Technique
RRYGB and PRYGB surgeries were performed by two independent surgeons (who operate on approximately 800 patients/year) and four assistant surgeons, per the standard protocols and international guidelines. For PRYGB and RRYGB, the lengths of the biliopancreatic and alimentary limbs were 100 cm each (Appendix 1).
Statistical Analysis
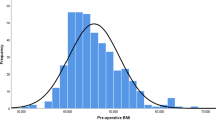
Descriptive and inferential statistics were used for the analyses. All data were tested for normality using the Kolmogorov − Smirnov test, Q-Q plot, and Levene’s test. Categorical variables are expressed as numbers and percentages. Normally and non-normally distributed continuous variables are presented as means and standard deviations (SDs) and medians and interquartile ranges, respectively. When appropriate, categorical variables were tested using Pearson’s chi-square test or Fisher’s exact test. Normally distributed continuous data were tested with dependent samples utilizing Student’s t-test for pre and postoperative results. The Wilcoxon signed-rank test was used for skewed (non-parametric) data. For the three RRYGB subgroups and PRYGB, a one-way ANOVA test was performed with multiple Tukey pairwise comparisons between the groups.
Predictors were evaluated and corrected using univariate and multivariate logistic regression analyses. All independent variables, including over 10 events with P-values < 0.1, were eligible for multivariate analysis, which was achieved through backward selection. The prediction model was evaluated using a − 2 log-likelihood test. P-values < 0.05 were considered statistically significant. Statistical analyses were performed using R-studio (version 4.0.4).
Stratification
Multiple stratification strategies were used to identify differences and trends within and between all groups. Two main stratifications of %EWL > 50 were performed, whereby the revisional cohort was stratified into three sub-strata (VBG, LSG, and GB). All were compared within and between each stratification and sub-stratification. Stratification 1 and 2 included patients with %EWL ≥ 50 and %EWL < 50, respectively.
Sample Size
G*power version 3.1.9.5 was used for sample size calculation. As this was a retrospective database study, we determined the minimum quantity required to identify the differences in %EWL. To detect a difference of delta 0.1 in the %EWL between PRYGB and RRYGB with an alpha of 0.05 and a beta > 0.8, we needed 51 patients per arm. Thus, a minimum of 306 patients, 153 for RRYGB and 153 for PRYGB, were required.
Methods for Narrative Review
All relevant and present studies on prediction modeling and internal or external validation in (revisional) BMS were collected for the narrative review.
PubMed was searched from its inception to November 28, 2022. We used the following terms and their synonyms, which were truncated where necessary:
-
Prediction/Predictors/Prediction/predictive/predict*/Model/modeling/model*/ AND Validation/validating/valid*/internal/external AND bariatric surgery/ bariatric surger*
Grey literature was also searched, and a reference crosscheck was performed to detect eligible articles that were not identified in the previous search. This search was conducted without restrictions on the language or publication date. The risk of bias for the methodological quality of each included study was not assessed because this narrative review aimed only to identify studies on prediction modeling and validation in BMS and baseline outcomes.
Two reviewers (BT and MH) independently screened the titles and abstracts of the studies based on the inclusion criteria, prediction model, validation study, and BMS. Thereafter, the same reviewers independently reviewed the remaining full-text reports for eligibility.
Furthermore, questions regarding prediction and validation requirements were analyzed and discussed under the purview of this review.
Results
This retrospective cohort study analyzed data between 2008 and 2019. A total of 558 and 338 patients underwent PRYGB and RRYGB after VBG, LSG, and GB, respectively, and completed 2 years of follow-up.
Lost to Follow-up Patients
Between 2008 and 2019, 691 patients underwent PRYGB, of whom 558 (80.8%) completed 2 years of follow-up, and 133 (19.2%) were lost to follow-up. In the revisional cohort, 516 patients underwent revision surgery; 97 (18.8%) were excluded because of other revision surgery than RYGB; in total, 338 (65.5%) completed 2 years of follow-up, and 81 (15.7%) were lost to follow-up.
Unstratified
Baseline Characteristics
BMI before primary surgery was 47.6 ± 7.04 and 50.4 ± 8.5 kg/m2 (p ≤ 0.001) in the PRYGB and RRYGB cohorts, respectively. Pre-revisional surgery, the BMI of 42.4 ± 6.04; %EWL, %TWL, and %EBMIL were 22.1, 11.3, and 14.0%, respectively (Table 1).
After 2 years, %EWL and %TWL within the PRYGB cohort were 89.8 ± 52.7 and 39.4 ± 60.1, respectively. For the RRYGB cohort, this was 38.6 ± 27.6 and 19.1 ± 22.4, respectively (p = 0.001) (the rest of the baseline characteristics are presented in Table 1).
Stratified
Percentage of Sufficient and Insufficient EWL (≥ 50% and <) Within the Group EWL Classes Between PRYGB and RRYGB
Overall, 78.5% of patients in the PRRYGB group had a sufficient EWL ≥ 50%, compared to 21.5% in the RRYGB.
41.1% in the PRYGB had insufficient (%EWL < 50), compared to 67.8% in the RRYGB.
Percentage of Sufficient and Insufficient EWL (≥ 50% and <) Within PRYGB and RRYGB
Overall, 71.3% of patients in the PRYGB group had sufficient EWL (≥ 50%) compared to 28.7% who were insufficient.
In the RRYGB group, 32.2% had sufficient EWL, compared to 67.8% who had insufficient %EWL (< 50%) (p < 0.001) (Table 1).
Before Revision Surgery
WL, %EWL, %TWL, %EBMIL, and BMI after primary surgery and before revision surgery, stratified in both %EWL classes and revisional surgery groups, were not significantly different (p ≥ 0.48).
Stratified Characteristics of Sufficient %EWL ≥ 50 (Stratum 1)
Patients who underwent LSG after revision surgery had the best outcomes, compared to VBG and GB (p ≤ 0.001). Patients in stratum 1 for PRYGB were significantly younger than those in PRYGB stratum 2 and both RRYGB strata (p ≤ 0.0001).
Those who underwent VBG had the greatest number of years between surgery (median [IQR] 10 [3.75]) and LSG, where the shortest with 5 (2.0) years (p = 0.001); however, no difference was observed between the p1 and p2 main strata (p = 0.452) (Table 2).
Weight Factors
The %EWL achieved 2 years after the revision surgeries for VBG, LSG, and GB was 68.5, 74.2, and 64.1%, respectively; the %TWL was 24.7, 30.4, and 24.6%, respectively. The LSG group had the highest %EWL and %TWL, which significantly differed from that of GB (p = 0.04, 0.03), but not VBG (p = 0.32, 0.38).
Compared with PRYGB as the control, the %EWL was 93.7 ± 15.5% and the %TWL was 47.3 ± 9.8% (p ≤ 0.001).
The BMI after 2 years remained significantly higher in the RRYGB group compared with the control PRYGB group (27.2, 26.8, and 28.3 kg/m3 vs. 24.6 kg/m3) (p ≤ 0.001).
Patients who underwent VBG had the highest nadir weight after primary surgery (92.8 ± 10.3) compared to the lowest (LSG 87.5 ± 11.2) (p = 0.06). Patients who underwent LSG had significantly more WL after revision than those who underwent VBG and GB (34.2 vs. 26.4 and 25.9) (p = 0.006, 0.01).
The lowest nadir weight after the first surgery was associated with the highest %EWL and %EBMIL after 2 years in the RRYGB group (Table 2, Fig. 1).
Stratified Characteristics of Insufficient %EWL < 50 (Stratum 2)
The %EWL achieved 2 years after the revision surgeries for VBG, LSG, and GB was 33.3, 33.2, and 28.4% (p ≤ 0.001), respectively; the %TWL was 15.7, 15.6, and 13.7%, respectively. Compared with PRYGB as the control, the %EWL was 38.4 ± 8.3% and %TWL was 19.6 ± 5.7% (p ≤ 0.001).
Patients who underwent VBG had the most insufficient %EWL < 50 after revision surgery compared to those who underwent GB and LSG (32.9, 17.7, and 8.2%), and combined with GB, had the longest follow-up time between surgeries (p ≤ 0.001).
The nadir weight and BMI in the LSG group were significantly lower than in the VBG and GB groups: nadir weight, 105.9 vs. 115.3 and 115.0 kg (p = 0.009), respectively.
The PRYGB group had significantly more WL than the RRYGB group after revision surgery (27.25 kg vs. 19.2 kg, 19.0 kg, and 17.3 kg, respectively) (p = 0.008). However, PRYGB showed no significant difference in BMI after 2 years compared to RRYGB (Table 3, Fig. 1).
Prediction Modeling
The baseline OR for sufficient %EWL ≥ 50 (with estimated LnOdds and p-values) were 2.4 (0.928, p ≤ 0.001), 1.45 (− 0.523, p = 0.003), 0.29 (− 2.143, p ≤ 0.001), and 0.32 (− 2.027, p = 0.004) for PRYGB, LSG, VBG, and GB, respectively.
Regarding the corrected factors after univariate and multivariate backward selection, age (estimated LnOdds, − 1.192, p = 0.0016) was the only significant variable in this study.
After testing all models, all other variables in this study were not significant predictors for %EWL ≥ 50 (p ≥ 0.05) (Tables 2 and 3, and Appendices 2, 3, and 4).
Narrative Review
From the inception of PubMed to November 28, 2022, 41,266 studies on BMS were identified. After applying the search strategy to prediction models and BMS, 672 (1.62%) studies were found (years of publication from 1992 to 2022). After title and abstract (TiAb) selection, 486 studies did not meet the inclusion “prediction model AND bariatric surgery” criteria, and 186 remained (0.45%).
A new TiAb selection was performed for “internal/ external validation” criteria, and 19 articles (0.046% of the 41, 266 BMS studies or 10.2% of the 186 prediction studies) that met this criterion remained (Fig. 2).
Seven studies (36.8%) were published in 2022 [18,19,20,21,22,23,24], five (26.3%) in 2021[25,26,27,28,29], one (5.3%) in 2020 [30], two (10.5%) in 2017 [31, 32], and one each (5.3%) in 2015, 2012, 2009, and 2007 [33,34,35,36].
Validation in Patients with Obesity
In total, 10 (52.6%) studies performed an internal validation [18, 19, 23,24,25,26, 28, 32, 34, 36], and 10 (52.6%) performed an external validation [18, 20,21,22, 27, 29,30,31, 33, 35] of the prediction model. One study tested internal and external validation. A median (min–max) 760 (70–750, 498) patients were included in the models.
Prediction and validation patients were evaluated once (5.3%) for complication risk, three times (15.8%) for mortality risk, once (5.3%) for gastroesophageal reflux disease (GERD), four times (21.1%) for diabetes remission, once (5.3%) for internal herniation, once (5.3%) for adverse cardiac events, once (5.3%) for frailty scores, twice (10.6%) on the outcome of sufficient and insufficient WL after BMS, three times (15.8%) for WL prediction, once (5.3%) for gastrointestinal leak and venous thromboembolism, and once (5.3%) for BMS quality of life. No studies were found on the prediction and validation of revision BMS.
Used Variables in the Included Studies
Extraction was conducted on models that presented and predicted variables the most in the validation stage of the studies.
Associated Medical Problems
Variables associated with medical problems were utilized for obstructive sleep apnea (OSA) 10 times (52.5%), GERD 10 times (52.5%), hypertension 11 times (57.9%), hyperlipidemia nine times (47.4%), coronary diseases eight times (42.1%), renal problems five times (26.3%), diabetes 14 times (74.7%), liver problems six times (31.6%), arthritis three times (15.7%), cardiac infarct five times (26.3%), and anastomotic leakage three times (15.8%).
General Variables
Furthermore, age was included 15 times (78.9%), gender 15 times (78.9%), short-term complication < 30 days once (5.3%), smoking nine times (47.4%), weight 12 times (63.2%), BMI 13 times (68.4%), %EWL five times (26.3%), ethnicity six times (31.6%), and neck, waist circumference, and continuous positive airway pressure/bilevel positive airway pressure (CPAP/BiPAP) once (5.3%).
Laboratory Values
High-density lipoproteins were included four times (21.1%), low-density lipoproteins three times (15.8%), triglycerides four times (21.1%), total cholesterol four times (21.1%), fasting blood sugar levels five times (26.3%), and hemoglobin A1C three times (15.8%).
Type of Surgery
The types of surgery used were RYGB 16 times (84.2%), LSG 13 times (68.4%), open RYGB twice (10.5%), biliopancreatic diversion with duodenal switch three times (15.7%), single anastomosis duodenal-ileal bypass with sleeve gastrectomy twice (10.5%), and gastric band twice (10.5%).
Area Under the Curve (AUC)
In total, 15 studies (78.9%) calculated an AUC for the validation, with an unweighted median (min–max) of the AUC of 0.79 (0.599–0.985) [18,19,20,21,22,23, 25, 26, 28,29,30,31,32, 34, 36]. The remaining studies used correlation coefficients (R or R2) for all the variables used [24, 27, 33, 35].
Discussion
This was a retrospective study on stratification that compared unstratified results in created stratified revisional surgery groups, combined with prediction modeling. Additionally, a narrative review of validation and prediction models in the literature was conducted.
BMS has proven effective in achieving significant long-term WL and improving or eliminating associated medical problems [37]. However, only 15–35% of patients reach a desirable %EWL ≥ 50 after surgery [37,38,39,40]. To our knowledge, no descriptions are available comparing different stratification analyses with a control group. No studies were found in the narrative review that investigated revision surgery as a model for testing and validating. Our results are consistent with those of other studies. A meta-analysis showed a 20% lower weight reduction after RRYGB than after PRYGB [8].
Insufficient WL is inherent in revisional procedures. The LSG had the best outcome in the sufficient and insufficient groups in our study. Fibrous capsules were found when removing the band, which may cause difficulties when creating a smaller pouch for RYGB. During VBG, scarring was visible through the mesh, and pouch construction was more difficult. Minimal adhesions were visible during LSG; therefore, pouch construction was simpler. Consequently, proper resection is more complex, resulting in a less well-constructed pouch and possibly less WL.
The strength of stratification was clearly visible in this study. First, by comparing the results of the unstratified %EWL and %TWL (as a continuous variable), we confirmed the results for PRYGB and RRYGB [8, 41]. However, when we stratified this (to the dichotomous outcome), the percentage of sufficient (%EWL ≥ 5 0) in PRYGB was only 71.3% compared to 28.7% of insufficient EWL (%EWL < 50). In RRYGB, the sufficient effect was only visible in 32.2% of the cases.
This will initiate debate on when it is unsuitable for stratifying EWL > 50%, EWL < 50%, or any subclassification with an outcome. The results may overestimate “sufficient” in a small group of patients (± 30% was insufficient in PRYGB), which is not achieved by the criteria of EWL50%. Therefore, more stratification, rather than only presenting continuous variables, must be applied. Also, multiple SRs found the outcome in weight loss as continuous %EWL what highlights the misconception that outcomes in the PRYGB and RRYGB possibly have poor responses in sufficient effect. The problem is that we do not know from all the other studies on EWL% outcome the ratio of sufficient effect since it is not stratified in the dichotomous outcomes [31, 42,43,44,45], whereby studies define sufficient EWL confirm our findings in both cohorts [25, 46,47,48].
Furthermore, the focus should be on sufficient and insufficient cut-off criteria and patients who show insufficient effect in both primary and revision surgery.
Several criteria, including weight gain, sufficient, and %EWL > 25%, have been used [49,50,51,52]. However, many studies use Reinhold’s criteria [53] for sufficient weight loss > 50%.
We continue to use %EWL > 50 because of the patient effects. Within our profession, the focus remains on the health gain for the patient after BMS. If sufficient WL is achieved at a lower %EWL, the patient may not have achieved sufficient health benefits, such as reducing associated medical problems.
This study showed that 28.7% of PRYGB patients and 67.8% of RRYGB patients did not reach the goal of EWL > 50%. The question remains as to why patients do not respond, even after a second attempt, with a procedure known as the truth-worth procedure. Additionally, why the patient showed insufficient WL on the first attempt? This study showed that with the differences in stratification and prediction models, we could not find any correlations.
Future of Prediction Models and External Validation
The last decade has witnessed a surge in the development of prognostic prediction models in medicine. A PubMed search by Ramspek et al. showed 84,032 studies on prediction models, of which only 4309 (5%) mentioned external validation in the title or abstract [54]. This narrative review showed that only 10.2% of validation was performed in prediction models. Additionally, only 52.6% of the studies conducted an external validation, consistent with the results of Ramspek et al. [54]. Furthermore, 68.4% of the validation research was conducted in the last 3 years (2022–2020). This reflects that validation studies in the field of BMS are new and should be highlighted, as 95% of prediction models are not externally validated.
Before any prediction model can be implemented, external validation is crucial because prediction models generally perform more poorly in external validation than in the development phase [55]. Ideally, external validation is performed in a separate study by different researchers to prevent adjusting of the model formula based on external validation results [55, 56].
Although it is preferable to have one validated prediction model in all settings and individuals, scientists should strive to validate models in clinically relevant subgroups; as seen in our study, mixed results can occur after the stratification of subgroups.
Contradictions Between Prediction and Stratification Models in This Study
In the study, it was impossible to create a prediction model that could assist in identifying sufficient WL in patients. However, new contradictions between the prediction and stratification were noted, which can assist us in validating models.
For example, our study showed that preoperative BMI was not a predictor for sufficient %EWL ≥ 50. However, significant differences were observed within and between the stratified PRYGB and RRYGB groups. In the unstratified analysis, there was a significant preoperative BMI difference in favor of PRYGB, although this was not visible in the prediction model.
In our stratified results, we noted that after the primary intervention in the RRYGB group, a higher %EWL or %EBMIL before the revision intervention correlated with higher sufficient WL after 2 years; this was not visible in our prediction model.
The best sufficient WL was observed in the prediction model at younger ages in the PRYGB group compared with the sufficient %EWL ≥ 50 in the RRYGB group. Several other studies found that age is one of the most consistent predictive factors; older patients had poor results [46, 57, 58].
A notable finding was observed within the stratification of insufficient EWL in this study: %EWL < 50 patients in the PRYGB group were significantly older than those in the insufficient RRYGB group (average 51.5 years vs. 42.5 years, respectively). They had significantly higher %EWL and %EBMIL (38.4% vs. an average of 33.2% in the RRYGB p ≤ 0.001). The number of years between primary and revisional surgery was not significantly different between the two strata (%EWL < 50 and %EWL > 50). However, there was a significant difference within both strata (sufficient and insufficient EWL) in favor of LSG (5 vs. 8–9 years). LSG showed the best result for predicted sufficiently %EWL within the revision group (OR LSG 1.45 vs. VBG 0.29, p ≤ 0.001; GB OR 0.32, p = 0.004).
The prediction model was determined by sufficient EWL, resulting in a model with missed prediction, despite the stratification results favoring a shorter time in both strata as the best sufficient %EWL. Several studies reported that a longer postoperative duration (> 2 years) significantly affected BMS outcomes [58,59,60,61].
The results show efficacy when stratified but not when a model is built. Therefore, caution is required when making assumptions based only on a prediction model; this may over or underestimate the outcome.
What Do We Need to Improve?
Correcting for confounding and bias and creating predictions is always essential; however, we cannot correct or predict what we do not measure.
In the future, external validation and prediction models that provide the entire model formula and specify the prediction horizon with absolute risk calculations are needed to achieve more insight, transparency, and the possibility to develop prediction models. Unfortunately, only 2 of the 19 studies in this narrative review published the intercept or baseline hazard [29], in combination with a beta coefficient [27, 29].
Limitations
During the analyses, the study’s retrospective design rendered the presentation of all variables a barrier to developing an accurate prediction model. A possible explanation could be that we included PRYGB and RRYGB in one prediction model (since PRYGB was the control and every patient had the chance for a %EWL > 50). One case could have affected the outcomes of the other. Predictive modeling may not be able to test on different data types for datasets and surgery outcomes; this may be tested in the future through external validation. Additionally, the follow-up time in our study cohort was 2 years, which may have been too short of making good predictions. We selected a cut-off of 2 years because it provided the most power for the presented number of patients; with longer follow-ups, the power of the study would decrease for the revisional cases. A longer follow-up could have been used for PRYGB; however, we used the 2-year follow-up to match the outcome. Finally, we conducted a narrative review, but no systematic review was conducted. Narrative reviews aim to identify and summarize what has been published, but no risk of bias assessment was performed, and only data on prediction models were checked. The results from this review will be extended to a systematic review while testing all the prediction studies that did not perform validation.
Conclusion
Approximately 32.2% of all the patients after revisional surgery had a sufficient %EWL ≥ 50 after 2 years, compared with 71.3% for PRYGB. LSG had the best outcome in the revisional surgery group in the sufficient %EWL group and the best outcome in the insufficient weight loss group. Skewness between the prediction model and stratification resulted in a non-functional prediction model. Extra attention to external validation is necessary to promote the creation of a prediction model that can be generalizable to all patients.
Data Availability
Data is available at the corresponding author.
References
Shah M, Simha V, Garg A. Long-term impact of bariatric surgery on body weight, comorbidities, and nutritional status. J Clin Endocrinol Metab. 2006;91:4223–31.
Carlsson LMS, Peltonen M, Ahlin S, et al. Bariatric surgery and prevention of type 2 diabetes in Swedish obese subjects. N Engl J Med. 2012;367:695–704.
Chen J-C, Hsu N-Y, Lee W-J, et al. Prediction of type 2 diabetes remission after metabolic surgery: a comparison of the individualized metabolic surgery score and the ABCD score. Surg Obes Relat Dis. 2018;14:640–5.
Magro DO, Geloneze B, Delfini R, et al. Long-term weight regain after gastric bypass: a 5-year prospective study. Obes Surg. 2008;18:648–51.
Guan B, Chong TH, Peng J, et al. Mid-long-term revisional surgery after sleeve gastrectomy: a systematic review and meta-analysis. Obes Surg. 2019;29:1965–75.
Lazzati A, Bechet S, Jouma S, et al. Revision surgery after sleeve gastrectomy: a nationwide study with 10 years of follow-up. Surg Obes Relat Dis. 2020;16:1497–504.
van Wezenbeek MR, Smulders FJF, de Zoete J-PJGM, et al. Long-term results after revisions of failed primary vertical banded gastroplasty. WJGS. 2016;8:238.
Pędziwiatr M, Małczak P, Wierdak M, et al. Revisional gastric bypass is inferior to primary gastric bypass in terms of short- and long-term outcomes—systematic review and meta-analysis. Obes Surg. 2018;28:2083–91.
Sanchez H, Cabrera A, Cabrera K, et al. Laparoscopic Roux-en-Y gastric bypass as a revision procedure after restrictive bariatric surgery. Obes Surg. 2008;18:1539–43.
Aelfers SCW, Schijns W, Ploeger N, et al. Patients’ preoperative estimate of target weight and actual outcome after bariatric surgery. Obes Surg. 2017;27:1729–34.
van Wezenbeek MR, van Oudheusden TR, de Zoete JPJGM, et al. Conversion to gastric bypass after either failed gastric band or failed sleeve gastrectomy. Obes Surg. 2017;27:83–9.
Oyefule O, Do T, Karthikayen R, et al. Secondary bariatric surgery—does the type of index procedure affect outcomes after conversion? J Gastrointest Surg. 2022;26:1830–7.
Mahawar KK, Graham Y, Carr WRJ, et al. Revisional Roux-en-Y gastric bypass and sleeve gastrectomy: a systematic review of comparative outcomes with respective primary procedures. Obes Surg. 2015;25:1271–80.
Carandina S, Maldonado PS, Tabbara M, et al. Two-step conversion surgery after failed laparoscopic adjustable gastric banding. Comparison between laparoscopic Roux-en-Y gastric bypass and laparoscopic gastric sleeve. Surg Obes Relat Dis. 2014;10:1085–91.
Kermansaravi M, Shahmiri SS, DavarpanahJazi AH, et al. One anastomosis/mini-gastric bypass (OAGB/MGB) as revisional surgery following primary restrictive bariatric procedures: a systematic review and meta-analysis. Obes Surg. 2021;31:370–83.
Ganju J, Zhou K. The benefit of stratification in clinical trials revisited. Statist Med. 2011;30:2881–9.
Binda A, Jaworski P, Kudlicka E, et al. The impact of selected factors on parameters of weight loss after sleeve gastrectomy. WIITM. 2016;4:288–94.
Akpinar EO, Ghaferi AA, Liem RSL, et al. Predicting serious complication risks after bariatric surgery: external validation of the Michigan Bariatric Surgery Collaborative risk prediction model using the Dutch Audit for Treatment of Obesity. Surg Obes Relat Dis. 2023;19(3):212–21. https://doi.org/10.1016/j.soard.2022.09.008.
Emile SH, Ghareeb W, Elfeki H, et al. Development and validation of an artificial intelligence-based model to predict gastroesophageal reflux disease after sleeve gastrectomy. Obes Surg. 2022;32:2537–47.
Fatima F, Hjelmesæth J, Hertel JK, et al. Validation of Ad-DiaRem and ABCD diabetes remission prediction scores at 1-year after Roux-en-Y gastric bypass and sleeve gastrectomy in the randomized controlled oseberg trial. Obes Surg. 2022;32:801–9.
Giudicelli G, Poletti P-A, Platon A, et al. Development and validation of a predictive model for internal hernia after Roux-en-Y gastric bypass in a multicentric retrospective cohort: the Swirl, weight excess loss, liquid score. Ann Surg. 2022;275:1137–42.
Karpińska IA, Choma J, Wysocki M, et al. External validation of predictive scores for diabetes remission after metabolic surgery. Langenbecks Arch Surg. 2022;407:131–41.
Mocanu V, Dang JT, Delisle M, et al. 30-day Major Adverse Cardiac Events (MACE) after elective bariatric surgery: the development and validation of the Bari-MACE clinical predictive tool. Surg Obes Relat Dis. 2022;18:357–64.
Sebastian R, Ghanem OM, Cornejo J, et al. Validation of the cumulative deficit theory in bariatric surgery: new bariatric frailty score is associated with non-home discharge, prolonged hospital stay and mortality in the era of fast-track bariatric surgery. Surg Obes Relat Dis. 2022;18:779–88.
Bioletto F, Pellegrini M, D’Eusebio C, et al. Development and validation of a scoring system for pre-surgical and early post-surgical prediction of bariatric surgery unsuccess at 2 years. Sci Rep. 2021;11:21067.
Blume CA, Brust-Renck PG, Rocha MK, et al. Development and validation of a predictive model of success in bariatric surgery. Obes Surg. 2021;31:1030–7.
Karpińska IA, Kulawik J, Pisarska-Adamczyk M, et al. Is it possible to predict weight loss after bariatric surgery?—external validation of predictive models. Obes Surg. 2021;31:2994–3004.
Nudel J, Bishara AM, de Geus SWL, et al. Development and validation of machine learning models to predict gastrointestinal leak and venous thromboembolism after weight loss surgery: an analysis of the MBSAQIP database. Surg Endosc. 2021;35:182–91.
Plaeke P, Beunis A, Ruppert M, et al. Review, performance comparison, and validation of models predicting type 2 diabetes remission after bariatric surgery in a Western European population. Obes Surg. 2021;31:1549–60.
Tewksbury C, Geng Z, Foster M, et al. Validation and improvement of a highly predictive bariatric surgery mortality risk calculator to include sleeve gastrectomy using MBSAQIP 2015–2017 data. Surg Obes Relat Dis. 2020;16:725–31.
Sharples AJ, Charalampakis V, Daskalakis M, et al. Systematic review and meta-analysis of outcomes after revisional bariatric surgery following a failed adjustable gastric band. Obes Surg. 2017;27:2522–36.
Slotman GJ. Prospectively validated preoperative prediction of weight and co-morbidity resolution in individual patients comparing five bariatric operations. Surg Obes Relat Dis. 2017;13:1590–7.
Sampaio-Neto J, Nassif LS, Branco-Filho AJ, et al. External validation of the diarem score as remission predictor of diabetes mellitus type 2 in obese patients undergoing Roux-en-Y gastric bypass. ABCD Arq Bras Cir Dig. 2015;28:19–22.
Ramanan B, Gupta PK, Gupta H, et al. Development and validation of a bariatric surgery mortality risk calculator. J Am Coll Surg. 2012;214:892–900.
Weiner S, Sauerland S, Weiner R, et al. Validation of the adapted Bariatric Quality of Life Index (BQL) in a prospective study in 446 bariatric patients as one-factor model. Obes Facts. 2009;2:63–6.
DeMaria EJ, Murr M, Byrne TK, et al. Validation of the obesity surgery mortality risk score in a multicenter study proves it stratifies mortality risk in patients undergoing gastric bypass for morbid obesity. Ann Surg. 2007;246:578–82 (discussion 583-584).
Maggard MA, Shugarman LR, Suttorp M, et al. Meta-analysis: surgical treatment of obesity. Ann Intern Med. 2005;142(7):547–59. https://doi.org/10.7326/0003-4819-142-7-200504050-00013.
Brolin RE, Cody RP. Adding malabsorption for weight loss failure after gastric bypass. Surg Endosc. 2007;21:1924–6.
Rawlins ML, Teel D, Hedgcorth K, et al. Revision of Roux-en-Y gastric bypass to distal bypass for failed weight loss. Surg Obes Relat Dis. 2011;7:45–9.
Parikh M, Pomp A, Gagner M. Laparoscopic conversion of failed gastric bypass to duodenal switch: technical considerations and preliminary outcomes. Surg Obes Relat Dis. 2007;3:611–8.
Slegtenhorst BR, van der Harst E, Demirkiran A, et al. Effect of primary versus revisional Roux-en-Y gastric bypass: inferior weight loss of revisional surgery after gastric banding. Surg Obes Relat Dis. 2013;9:253–8.
Chen G, Zhang G, Peng B, et al. Roux-en-Y gastric bypass versus sleeve gastrectomy plus procedures for treatment of morbid obesity: systematic review and meta-analysis. Obes Surg. 2021;31:3303–11.
Brunaldi VO, Jirapinyo P, de Moura DTH, et al. Endoscopic treatment of weight regain following Roux-en-Y gastric bypass: a systematic review and meta-analysis. Obes Surg. 2018;28:266–76.
Fehervari M, Banh S, Varma P, et al. Weight loss specific to indication, remission of diabetes, and short-term complications after sleeve gastrectomy conversion to Roux-en-Y gastric bypass: a systematic review and meta-analysis. Surg Obes Relat Dis. 2022;S1550-7289(22):00757–2. https://doi.org/10.1016/j.soard.2022.11.004.
Uhe I, Douissard J, Podetta M, et al. Roux-en-Y gastric bypass, sleeve gastrectomy, or one-anastomosis gastric bypass? A systematic review and meta-analysis of randomized-controlled trials. Obesity. 2022;30:614–27.
Cazzo E, da Silva FP, Pareja JC, et al. Predictors for weight loss failure following Roux-en-Y gastric bypass. Arq Gastroenterol. 2014;51:328–30.
Cadena-Obando D, Ramírez-Rentería C, Ferreira-Hermosillo A, et al. Are there really any predictive factors for a successful weight loss after bariatric surgery? BMC Endocr Disord. 2020;20:20.
Łabul M, Wysocki M, Bartosiak K, et al. Analysis of the factors contributing to bariatric success after laparoscopic redo bariatric procedures: results from multicenter Polish Revision Obesity Surgery Study (PROSS). Obes Surg. 2022;32:3879–90.
Nedelcu M, Khwaja HA, Rogula TG. Weight regain after bariatric surgery—how should it be defined? Surg Obes Relat Dis. 2016;12(5):1129–1130. https://doi.org/10.1016/j.soard.2016.04.028.
El Ansari W, Elhag W. Weight regain and insufficient weight loss after bariatric surgery: definitions, prevalence, mechanisms, predictors, prevention and management strategies, and knowledge gaps—a scoping review. Obes Surg. 2021;31:1755–66.
Lauti M, Kularatna M, Hill AG, et al. Weight regain following sleeve gastrectomy—a systematic review. Obes Surg. 2016;26:1326–34.
Nasri B-N, Trainor L, Jones DB. Laparoscopic adjustable gastric band remains a safe, effective, and durable option for surgical weight loss. Surg Endosc. 2022;36:7781–8.
Reinhold RB. Critical analysis of long term weight loss following gastric bypass. Surg Gynecol Obstet. 1982;155:385–94.
Ramspek CL, Jager KJ, Dekker FW, et al. External validation of prognostic models: what, why, how, when and where? Clin Kidney J. 2021;14:49–58.
Siontis GCM, Tzoulaki I, Castaldi PJ, et al. External validation of new risk prediction models is infrequent and reveals worse prognostic discrimination. J Clin Epidemiol. 2015;68:25–34.
Steyerberg EW, Harrell FE. Prediction models need appropriate internal, internal–external, and external validation. J Clin Epidemiol. 2016;69:245–7.
Al-Khyatt W, Ryall R, Leeder P, et al. Predictors of inadequate weight loss after laparoscopic gastric bypass for morbid obesity. OBES SURG. 2017;27:1446–52.
Barhouch AS, Padoin AV, Casagrande DS, et al. Predictors of excess weight loss in obese patients after gastric bypass: a 60-month follow-up. Obes Surg. 2016;26:1178–85.
Scozzari G, Passera R, Benvenga R, et al. Age as a long-term prognostic factor in bariatric surgery. Ann Surg. 2012;256:724–9.
Bastos ECL, Barbosa EMWG, Soriano GMS, et al. Fatores determinantes do reganho ponderal no pós-operatório de cirurgia bariátrica. ABCD Arq Bras Cir Dig. 2013;26:26–32.
Hany M, Hafez Mohammad MK, AbdElhafeez NA, et al. A cross-sectional survey of patients attending follow-up visits after sleeve gastrectomy: Factors affecting weight loss. Obesity Pillars. 2022;3: 100029.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
1. Overall, 32.2% of all patients after revisional RYGB had a sufficient %EWL ≥ 50 after 2 years.
2. LSG had the best outcome in the revisional surgery group in the sufficient %EWL group and the best outcome in the insufficient weight loss group.
3. This narrative review showed only a 10.2% presence of validation in the prediction models.
4. This narrative review showed that 52.6% of the studies performed an external validation.
Appendices
Appendix 1. Surgical workflow per procedure
Revisional RYGB from VBG
The port sites were modified to avoid the expected areas of adhesions; pneumoperitoneum was created using a visual entry trocar at the left mid-clavicular line approximately 10 cm below the costal margin; this port would be used as a right-hand working port. In cases of adhesions, with the anterior abdominal wall hindering the insertion of the camera and left working ports, the assistant’s port in the left anterior clavicular line was first inserted to dissect these adhesions.
After creating the pneumoperitoneum, adhesions between the stomach and liver were dissected using the energy device Enseal (Ethicon Endo-Surgery, Cincinnati, OH, USA) to identify the mesh to create the correct plane; then, dissection continued up to the angle of His to identify the vertical staple line and expose the gastric serosa. The lesser omentum was dissected off the greater omentum at the body and fundus, with division of the short gastric vessels using the energy device to free the fundus and body. This was followed by dissection of the esophagogastric junction with crural repair using 2/0 V-Loc nonabsorbable sutures (Covidien, Mansfield, MA, USA), if a hiatal hernia was identified. Intraoperative endoscopy was performed at this step to identify the position of the mesh and vertical staple line. Small bowel exploration was attempted before creating the gastric pouch to exclude adhesions or short mesentery to ensure a tension-free gastro-jejunostomy.
The creation of the gastric pouch of RYGB is initiated by opening a window at the lesser curvature 1–2 cm above the mesh, cautiously avoiding injury to the blood supply, followed by horizontal stapling using an Echelon Flex Endopath 60-mm linear stapler (Ethicon Endo-Surgery, Cincinnati, OH, USA) with black reloads. This is continued up to the angle of His using black and green reloads over a 40 Fr bougie, while maintaining the staple line medial to the last vertical staple line inside the VBG pouch. Resection of the gastric fundus and part of the body, including the mesh and the previous staple line, was performed in all cases using the same stapler with green reloads transversely below the mesh.
Biliopancreatic and alimentary limbs lengths were equal, 100 cm each. Gastro-jejunostomy and jejuno-jejunostomy were performed using the same stapler with blue and white reloads, respectively; hand-sewn closure of the gastrostomy and enterostomies were performed using 3/0 V-Loc 180 sutures (Covidien, Mansfield, MA, USA). White reloads were used for dividing the jejunum.
All staple lines were reinforced with continuous seromuscular sutures (3/0 V-Loc 180 (Covidien, Mansfield, MA, USA)). Mesenteric defects were routinely closed using 3/0 V-Loc nonabsorbable sutures (Covidien, Mansfield, MA, USA) in all cases.
Endoscopic examination was repeated to visualize the mucosa of the pouch, and the gastro-jejunostomy was used to assess the vitality of the tissues, exclude intraluminal bleeding, and perform a leak test using air under a water seal. Blue dye leak testing was performed for the gastro-jejunostomy after endoscopy in all cases. A drain was inserted in the left sub-phrenic space at the end of the procedure.
Revisional RYGB from LSG
Adhesions were dissected around the gastric sleeve using the energy device EnSeal® (Ethicon Endo-Surgery, Cincinnati, OH, USA). The gastric pouch was created from 5 to 6 cm below the esophagogastric junction using an Echelon Flex Endopath 60-mm linear stapler (Ethicon Endo-Surgery, Cincinnati, OH, USA) over a 40 Fr bougie, with gold and blue reloads. The same stapler was used to construct the gastro-jejunostomy and jejuno-jejunostomy using blue and white reloads, respectively, with equal 100 cm biliopancreatic and alimentary limbs. The stapling defects were closed in two layers using barbed sutures (3/0 V-Loc 180 sutures (Covidien, Mansfield, MA, USA)). The staple line in the gastric pouch and remnant stomach was reinforced with seromuscular continuous sutures using the same barbed sutures. All mesenteric defects were closed using 3/0 V-Loc nonabsorbable sutures (Covidien, Mansfield, MA, USA).
Revisional RYGB from GB
All surgeries in our cohort were performed using a single-step conversion standard: five ports were used, including three 12-mm ports (for the camera and right and left working ports) and two 5-mm ports (for liver retraction and the assistant). A pneumoperitoneum was created after using optical trocars for entry. Adhesions around the stomach were dissected using the energy device EnSeal® (Ethicon Endo-Surgery, Cincinnati, OH, USA). Subsequently, the tube was disconnected at the level of the abdominal wall. Adhesions between the ventral aspect of the stomach and liver were removed to ensure optimal placement of the liver retractor. The entire scar capsule of the band was dismantled, considering that the band could have been placed “pars flaccida” or “perigastrically.” The entire band was then placed aside.
The gastric pouch was created from 5 to 6 cm below the esophagogastric junction using an Echelon Flex Endopath 60-mm linear stapler (Ethicon Endo-Surgery, Cincinnati, OH, USA) over a 40 Fr bougie using gold and blue reloads. Whenever possible, we tried to create the pouch above the level of the band. The same stapler was used to construct the gastro-jejunostomy and jejuno-jejunostomy using blue and white reloads, respectively, with equal 100-cm biliopancreatic and alimentary limbs. The stapling defects were closed in two layers using barbed 3/0 V-Loc 180 sutures (Covidien, Mansfield, MA, USA). The staple line in the gastric pouch and remnant stomach was reinforced with continuous seromuscular sutures using the same barbed sutures. All mesenteric defects were closed using 3/0 V-Loc nonabsorbable sutures (Covidien, Mansfield, MA, USA).
Primary RYGB
A pneumoperitoneum was created using visual entry trocars and a 0° angled lens; five standard ports were used, including three 12-mm ports (for the camera, and right and left working ports) and two 5-mm ports (for liver retraction and the assistant). The pouch was created with the same linear stapler using gold and blue reloads. The lengths of the biliopancreatic and alimentary limbs were equal, 100 cm each, as per revisional RYGB. The gastro-jejunostomy and the jejuno-jejunostomy were performed similarly to revisional RYGB.
All staple lines were reinforced with the same technique used for revisional RYGB. Mesenteric defects were also routinely closed. Intraoperative endoscopy was not routinely performed for primary RYGB. The blue dye leak test was routinely performed for the gastro-jejunostomy. A drain was routinely inserted in the left sub-phrenic space.
Appendix 2
Table 4
Appendix 3
Table 5
Appendix 4
Table 6
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hany, M., Zidan, A., Sabry, K. et al. How Good is Stratification and Prediction Model Analysis Between Primary and Revisional Roux-en-Y Gastric Bypass Surgery? A Multi-center Study and Narrative Review. OBES SURG 33, 1431–1448 (2023). https://doi.org/10.1007/s11695-023-06532-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-023-06532-3