Abstract
Background
Despite many patients doing well after laparoscopic adjustable gastric band (LAGB) several studies caution offering this procedure for weight loss. The aim of our study was to review our long-term results over a decade.
Methods
Following IRB approval, the Metabolic and Bariatric Surgery Quality Improvement Program (MBSAQIP) Data Registry was used to identify LAGB placement between 2007 and 2013 by a single surgeon. We sought to determine complications of initial operation, weight loss and resolution of comorbidities over time, the indications for reoperation including removal, revision or conversion to another weight loss surgery. Chi-square test was used to analysis.
Results
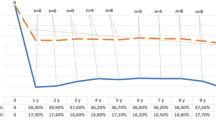
From 403 LAGB performed between January 2007 and December 2013, 75 patients required reoperation with total 79 procedures, including band revision and/or conversion. Mean follow-up time was 5.78 years (73.67 months). The rate of reoperation was at least 18.61%. There were 60 band removals, 10 band revisions, 9 conversions to either sleeve or gastric bypass. Only 16 patients (20.25%) required reoperation due to inadequate weight loss. Band slippage/prolapse remained the most common non weight-related indication for reoperation (23, 29.11%). Reoperation associated with longer length of stay compared to index procedures (2.12 days vs 1.63 days, p < 0.0001) but no statistical difference in 30_days_complication. Of those who did not require reoperation, BMI at 10th year follow-up was 37.50 from initial BMI of 42.23 with EWL of 39.22%.
Conclusions
Lap band is effective for most patients with long-term durability. Over time approximately one fifth will need additional surgery. Only one fifth of reoperation relates to inadequate weight loss.








Similar content being viewed by others
References
Hales CM, Carroll MD, Fryar CD, Ogden CL (2020) Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief 360:1–8
Finkelstein EA, Trogdon JG, Cohen JW, Dietz W (2009) Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff (Millwood) 28(5):822–831
Schauer PR, Bhatt DL, Kirwan JP, Aminian A, STAMPEDE Investigators et al (2017) Bariatric surgery versus intensive medical therapy for diabetes—5-year outcomes. N Engl J Med 376(7):641–651
Sheng B, Truong K, Spitle H et al (2017) The long-term effects of bariatric surgery on type 2 diabetes remission, microvascular and macrovascular complications, and mortality: a systematic review and meta-analysis. Obes Surg 27(10):2724–2732
Buchwald H, Oien DM (2009) Metabolic/bariatric surgery worldwide 2008. Obes Surg 19(12):1605–1611
Buchwald H, Oien DM (2013) Metabolic/bariatric surgery worldwide 2011. Obes Surg 23(4):427–436
The American Society of Metabolic and Bariatric Surgery. Estimate of bariatric surgery numbers, 2011–2015. Accessed November 2021
Mognol P, Chosidow D, Marmuse JP (2005) Laparoscopic gastric bypass versus laparoscopic adjustable gastric banding in the super-obese: a comparative study of 290 patients. Obes Surg 15(1):76–81
Poulose BK, Griffin MR, Zhu Y et al (2005) National analysis of adverse patient safety for events in bariatric surgery. Am Surg 71(5):406–413
Victorzon M, Tolonen P (2013) Mean fourteen-year, 100% follow-up of laparoscopic adjustable gastric banding for morbid obesity. Surg Obes Relat Dis 9(5):753–757
Ding S-A, Simonson DC, Wewalka M et al (2015) Adjustable gastric band surgery or medical management in patients with type 2 diabetes: a randomized clinical trial. J Clin Endocrinol Metab 100(7):2546–2556
Spivak H, Abdelmelek MF, Beltran OR, Ng AW, Kitahama S (2012) Long-term outcomes of laparoscopic adjustable gastric banding and laparoscopic Roux-en-Y gastric bypass in the United States. Surg Endosc 26(7):1909–1919
Wee CC, Fleishman A, McCarthy AC, Jones DB et al (2019) Decision regret up to 4 years after gastric bypass and gastric banding. Obes Surg 29(5):1624–1631
Athanasiadis DI, Martin A, Kapsampelis P, Monfared S, Stefanidis D (2021) Factors associated with weight regain post-bariatric surgery: a systematic review. Surg Endosc 35(8):4069–4084
Clapp B, Wynn M, Martyn C, Foster C, O’Dell M, Tyroch A (2018) Long term (7 or more years) outcomes of the sleeve gastrectomy: a meta-analysis. Surg Obes Relat Dis 14(6):741–747
Tran DD, Nwokeabia ID, Purnell S, Zafar SN, Ortega G, Hughes K, Fullum TM (2016) Revision of Roux-En-Y gastric bypass for weight regain: a systematic review of techniques and outcomes. Obes Surg 26(7):1627–1634
Dang JT, Switzer NJ, Wu J et al (2016) Gastric band removal in revisional bariatric surgery, one-step versus two-step: a systematic review and meta-analysis. Obes Surg 26(4):866–873
Gonzalez-Heredia R, Masrur M, Patton K, Bindal V et al (2015) Revisions after failed gastric band: sleeve gastrectomy and Roux-en-Y gastric bypass. Surg Endosc 29(9):2533–2537
Valle E, Luu MB, Autajay K, Francescatti AB et al (2012) Frequency of adjustments and weight loss after laparoscopic adjustable gastric banding. Obes Surg 22(12):1880–1883
O’Brien PE, MacDonald L, Anderson M, Brennan L, Brown WA (2013) Long-term outcomes after bariatric surgery: fifteen-year follow-up of adjustable gastric banding and a systematic review of the bariatric surgical literature. Ann Surg 257(1):87–94
Altieri MS, Yang J, Telem DA, Meng Z et al (2016) Lap band outcomes from 19,221 patients across centers and over a decade within the state of New York. Surg Endosc 30(5):1725–1732
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Bao-Ngoc Nasri, Daniel B. Jones, and Linda Trainor have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nasri, BN., Trainor, L. & Jones, D.B. Laparoscopic adjustable gastric band remains a safe, effective, and durable option for surgical weight loss. Surg Endosc 36, 7781–7788 (2022). https://doi.org/10.1007/s00464-022-09278-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09278-8