Abstract
Purpose
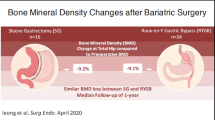
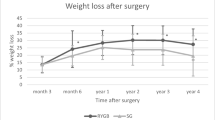
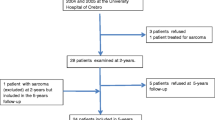
Patients with severe obesity submitted to Roux-en-Y gastric bypass (RYGB) are at risk of developing long-term hypovitaminosis D and secondary hyperparathyroidism (SHPT) as well as osteometabolic disease. This study aimed to evaluate calcium-vitamin D-PTH axis and bone mineral density (BMD) changes from post-RYGB patients who were followed-up until a median of 5 years.
Materials and Methods
Vitamin D deficiency was defined as 25-hydroxyvitamin D <20 ng/mL and SHPT as PTH >68 pg/mL, in patients with normal serum creatinine and calcium. BMD was estimated by dual-energy X-ray absorptiometry (DXA, g/cm2).
Results
We included 127 post-RYGB patients (51±10.6 years, 87.4% self-declared White, 91.3% female, 52.8% postmenopausal). Vitamin D deficiency prevalence was the highest (41.5%) in the second year and the lowest (21.2%) in the third year (p<0.05). SHPT prevalence was 65.4% in the second year and increased to 83.7% in the sixth year (p<0.05). Patients with low BMD in lumbar, femoral neck, and total proximal femur were older and presented menopausal status more frequently than normal BMD group (p<0.05). Older age was a risk marker for altered BMD in femoral neck (OR=1.185; 95% CI 1.118–1.256) and in total proximal femur (OR=1.158; 95% CI 1.066–1.258), both after adjusting for follow-up and excess weight loss.
Conclusion
After 5 years, most bariatric patients presented calcium-vitamin D-PTH axis disruption, in which SHPT was more frequent than hypovitaminosis D. Older patients and menopausal women presented higher rates of low BMD, and older age was a risk marker, especially for low BMD in femoral sites.
Graphical Abstract



Similar content being viewed by others
References
GBD 2015 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioral, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1659–724. https://doi.org/10.1016/S0140-6736(16)31679-8. Erratum in: Lancet. 2017 Jan 7;389(10064):e1. PMID: 27733284; PMCID: PMC5388856
Vigitel Brasil 2021. Vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico / Ministério da Saúde, Secretaria de Vigilância em Saúde, Departamento de Vigilância de Doenças e Agravos não Transmissíveis e Promoção da Saúde. Brasília: Ministério da Saúde; 2022.
Nguyen NT, Varela JE. Bariatric surgery for obesity and metabolic disorders: state of the art. Nat Rev Gastroenterol Hepatol. 2017;14(3):160–9. https://doi.org/10.1038/nrgastro.2016.170. Epub 2016 Nov 30
Reges O, Greenland P, Dicker D, Leibowitz M, Hoshen M, Gofer I, Rasmussen-Torvik LJ, Balicer RD. Association of bariatric surgery using laparoscopic banding, Roux-en-Y gastric bypass, or laparoscopic sleeve gastrectomy vs. usual care obesity management with all-cause mortality. JAMA. 2018;319(3):279–90. https://doi.org/10.1001/jama.2017.20513. PMID: 29340677; PMCID: PMC5833565
Adams TD, Gress RE, Smith SC, Halverson RC, Simper SC, Rosamond WD, Lamonte MJ, Stroup AM, Hunt SC. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357(8):753–61. https://doi.org/10.1056/NEJMoa066603.
Via MA, Mechanick JI. Nutritional and micronutrient care of bariatric surgery patients: current evidence update. Curr Obes Rep. 2017;6(3):286–96. https://doi.org/10.1007/s13679-017-0271-x.
Mahawar KK, Clare K, O'Kane M, Graham Y, Callejas-Diaz L, Carr WRJ. Patient perspectives on adherence with micronutrient supplementation after bariatric surgery. Obes Surg. 2019;29(5):1551–6. https://doi.org/10.1007/s11695-019-03711-z.
Dewey M, Heuberger R. Vitamin D and calcium status and appropriate recommendations in bariatric surgery patients. Gastroenterol Nurs. 2011;34(5):367–74. https://doi.org/10.1097/SGA.0b013e318229bcd0.
Wei JH, Lee WJ, Chong K, Lee YC, Chen SC, Huang PH, Lin SJ. High Incidence of Secondary Hyperparathyroidism in Bariatric Patients: Comparing Different Procedures. Obes Surg. 2018;28(3):798–804. https://doi.org/10.1007/s11695-017-2932-y.
Kim J, Nimeri A, Khorgami Z, El Chaar M, Lima AG, Vosburg RW, American Society for Metabolic and Bariatric Surgery (ASMBS) Clinical Issues Committee. Metabolic bone changes after bariatric surgery: 2020 update, American Society for Metabolic and Bariatric Surgery Clinical Issues Committee position statement. Surg Obes Relat Dis. 2021;17(1):1–8. https://doi.org/10.1016/j.soard.2020.09.031.
Gagnon C, Schafer AL. Bone health after bariatric surgery. JBMR Plus. 2018;2(3):121–33. https://doi.org/10.1002/jbm4.10048. PMID: 30283897; PMCID: PMC6124196
Saad R, Habli D, El Sabbagh R, Chakhtoura M. Bone health following bariatric surgery: an update. J Clin Densitom. 2020;23(2):165–81. https://doi.org/10.1016/j.jocd.2019.08.002. Epub 2019 Aug 9
Geoffroy M, Charlot-Lambrecht I, Chrusciel J, Gaubil-Kaladjian I, Diaz-Cives A, Eschard JP, Salmon JH. Impact of bariatric surgery on bone mineral density: observational study of 110 patients followed up in a specialized center for the treatment of obesity in France. Obes Surg. 2019;29(6):1765–72. https://doi.org/10.1007/s11695-019-03719-5.
Brzozowska MM, Tran T, Bliuc D, Jorgensen J, Talbot M, Fenton-Lee D, Chen W, Hong A, Viardot A, White CP, Nguyen TV, Pocock N, Eisman JA, Baldock PA, Center JR. Roux-en-Y gastric bypass and gastric sleeve surgery result in long term bone loss. Int J Obes (Lond). 2021;45(1):235–46. https://doi.org/10.1038/s41366-020-00660-x. Epub 2020 Aug 26
Yu EW, Bouxsein ML, Putman MS, Monis EL, Roy AE, Pratt JS, Butsch WS, Finkelstein JS. Two-year changes in bone density after Roux-en-Y gastric bypass surgery. J Clin Endocrinol Metab. 2015;100(4):1452–9. https://doi.org/10.1210/jc.2014-4341. Epub 2015 Feb 3. PMID: 25646793; PMCID: PMC4399296
Lindeman KG, Greenblatt LB, Rourke C, Bouxsein ML, Finkelstein JS, Yu EW. Longitudinal 5-year evaluation of bone density and microarchitecture after Roux-en-y gastric bypass surgery. J Clin Endocrinol Metab. 2018;103(11):4104–12. https://doi.org/10.1210/jc.2018-01496. PMID: 30219833; PMCID: PMC6194805
Raoof M, Näslund I, Rask E, Szabo E. Effect of gastric bypass on bone mineral density, parathyroid hormone and vitamin D: 5 years follow-up. Obes Surg. 2016;26(5):1141–5. https://doi.org/10.1007/s11695-016-2114-3.
Paccou J, Martignène N, Lespessailles E, Babykina E, Pattou F, Cortet B, Ficheur G. Gastric bypass but not sleeve gastrectomy increases risk of major osteoporotic fracture: French population-based cohort study. J Bone Miner Res. 2020;35(8):1415–23. https://doi.org/10.1002/jbmr.4012. Epub 2020 Apr 16
Vilarrasa N, San José P, García I, Gómez-Vaquero C, Miras PM, de Gordejuela AG, Masdevall C, Pujol J, Soler J, Gómez JM. Evaluation of bone mineral density loss in morbidly obese women after gastric bypass: 3-year follow-up. Obes Surg. 2011;21(4):465–72. https://doi.org/10.1007/s11695-010-0338-1.
Beavers KM, Greene KA, Yu EW. Management of endocrine disease: bone complications of bariatric surgery: updates on sleeve gastrectomy, fractures, and interventions. Eur J Endocrinol. 2020;183(5):R119–32. https://doi.org/10.1530/EJE-20-0548. PMID: 32869608; PMCID: PMC8254876
Mechanick JI, Apovian C, Brethauer S, Garvey WT, Joffe AM, Kim J, Kushner RF, Lindquist R, Pessah-Pollack R, Seger J, Urman RD, Adams S, Cleek JB, Correa R, Figaro MK, Flanders K, Grams J, Hurley DL, Kothari S, et al. Clinical practice guidelines for the perioperative nutrition, metabolic, and nonsurgical support of patients undergoing bariatric procedures - 2019 update: cosponsored by American Association of Clinical Endocrinologists/American College of Endocrinology, The Obesity Society, American Society for Metabolic & Bariatric Surgery, Obesity Medicine Association, and American Society of Anesthesiologists. Surg Obes Relat Dis. 2020;16(2):175–247. https://doi.org/10.1016/j.soard.2019.10.025. Epub 2019 Oct 31
Ieong K, Ardila-Gatas J, Yang J, Zhang X, Tsui ST, Spaniolas K, Pryor AD. Bone mineral density changes after bariatric surgery. Surg Endosc. 2021;35(8):4763–70. https://doi.org/10.1007/s00464-020-07953-2.
Johnson JM, Maher JW, DeMaria EJ, Downs RW, Wolfe LG, Kellum JM. The long-term effects of gastric bypass on vitamin D metabolism. Ann Surg. 2006;243(5):701–4. https://doi.org/10.1097/01.sla.0000216773.47825.c1. PMID: 16633006; PMCID: PMC1570540
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Murad MH, Weaver CM, Endocrine Society. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911–30. https://doi.org/10.1210/jc.2011-0385. Epub 2011 Jun 6. Erratum in: J Clin Endocrinol Metab. 2011 Dec;96(12):3908
Alexandrou A, Tsoka E, Armeni E, Rizos D, Diamantis T, Augoulea A, Panoulis C, Liakakos T, Lambrinoudaki I. Determinants of secondary hyperparathyroidism in bariatric patients after Roux-en-Y gastric bypass or sleeve gastrectomy: a pilot study. Int. J Endocrinol. 2015;2015:984935. https://doi.org/10.1155/2015/984935. Epub 2015 Apr 9. PMID: 25949239; PMCID: PMC4408644
Ko BJ, Myung SK, Cho KH, Park YG, Kim SG, do Kim H, Kim SM. Relationship between bariatric surgery and bone mineral density: a Meta-analysis. Obes Surg. 2016;26(7):1414–21. https://doi.org/10.1007/s11695-015-1928-8.
Matos O, Ruthes EMP, Malinowski AKC, Lima AL, Veiga MS, Krause MP, Farah L, Souza CJF, Lass AD, Castelo-Branco C. Changes in bone mass and body composition after bariatric surgery. Gynecol Endocrinol. 2020;36(7):578–81. https://doi.org/10.1080/09513590.2020.1762558. Epub 2020 May 14
Vivan MA, Kops NL, Fülber ER, de Souza AC, Fleuri MASB, Friedman R. Prevalence of vitamin D depletion, and associated factors, among patients undergoing bariatric surgery in Southern Brazil. Obes Surg. 2019;29(10):3179–87. https://doi.org/10.1007/s11695-019-03963-9.
Schafer AL, Weaver CM, Black DM, Wheeler AL, Chang H, Szefc GV, Stewart L, Rogers SJ, Carter JT, Posselt AM, Shoback DM, Sellmeyer DE. Intestinal calcium absorption decreases dramatically after gastric bypass surgery despite optimization of vitamin D status. J Bone Miner Res. 2015;30(8):1377–85. https://doi.org/10.1002/jbmr.2467. Epub 2015 May 21. PMID: 25640580; PMCID: PMC4593653
Mônaco-Ferreira DV, Leandro-Merhi VA, Aranha NC, Brandalise A, Brandalise NA. Vitamin D deficiency and paratohommonium increase in late postoperative gastric bypass in Roux-en-Y. Arq Bras Cir Dig. 2018;31(4):e1407. https://doi.org/10.1590/0102-672020180001e1407. PMID: 30539982; PMCID: PMC6284378
Alejo Ramos M, Cano Rodríguez IM, Urioste Fondo AM, Pintor de la Maza B, Barajas Galindo DE, Fernández Martínez P, González Herráez L, González de Francisco T, Ballesteros Pomar MD. Secondary hyperparathyroidism in patients with biliopancreatic diversion after 10 years of follow-up, and relationship with vitamin D and serum calcium. Obes Surg. 2019;29(3):999–1006. https://doi.org/10.1007/s11695-018-03624-3.
Hewitt S, Aasheim ET, Søvik TT, Jahnsen J, Kristinsson J, Eriksen EF, Mala T. Relationships of serum 25-hydroxyvitamin D, ionized calcium and parathyroid hormone after obesity surgery. Clin Endocrinol (Oxf). 2018;88(3):372–9. https://doi.org/10.1111/cen.13531. Epub 2018 Jan 4
Botella-Carretero JI, Lafuente C, Montes-Nieto R, Balsa J, Vega-Piñero B, Garcia-Moreno F, Peromingo R, Galindo J, San-Millan JL, Escobar-Morreale H. Serum bioavailable vitamin D concentrations and bone mineral density in women after obesity surgery. Obes Surg. 2016;26(11):2732–7. https://doi.org/10.1007/s11695-016-2185-1.
Menegati GC, de Oliveira LC, Santos AL, Cohen L, Mattos F, Mendonça LM, Carneiro JR, Farias ML, Rosado EL. Nutritional status, body composition, and bone health in women after bariatric surgery at a University Hospital in Rio de Janeiro. Obes Surg. 2016;26(7):1517–24. https://doi.org/10.1007/s11695-015-1910-5.
Casimiro I, Sam S, Brady MJ. Endocrine implications of bariatric surgery: a review on the intersection between incretins, bone, and sex hormones. Physiol Rep. 2019;7(10):e14111. https://doi.org/10.14814/phy2.14111. PMID: 31134746; PMCID: PMC6536581
Khundmiri SJ, Murray RD, Lederer E. PTH and Vitamin D. Compr Physiol. 2016;6(2):561–601. https://doi.org/10.1002/cphy.c140071.
Luger M, Kruschitz R, Kienbacher C, Traussnigg S, Langer FB, Prager G, Schindler K, Kallay E, Hoppichler F, Trauner M, Krebs M, Marculescu R, Ludvik B. Vitamin D3 loading Is superior to conventional supplementation after weight loss surgery in vitamin D-deficient morbidly obese patients: a double-blind randomized placebo-controlled trial. Obes Surg. 2017;27(5):1196–207. https://doi.org/10.1007/s11695-016-2437-0. PMID: 27837387; PMCID: PMC5403855
Lanzarini E, Nogués X, Goday A, Benaiges D, de Ramón M, Villatoro M, Pera M, Grande L, Ramón JM. High-dose vitamin D supplementation is necessary after bariatric surgery: a prospective 2-year follow-up study. Obes Surg. 2015;25(9):1633–8. https://doi.org/10.1007/s11695-015-1572-3.
Ben-Porat T, Elazary R, Goldenshluger A, Sherf Dagan S, Mintz Y, Weiss R. Nutritional deficiencies four years after laparoscopic sleeve gastrectomy-are supplements required for a lifetime? Surg Obes Relat Dis. 2017;13(7):1138–44. https://doi.org/10.1016/j.soard.2017.02.021. Epub 2017 Mar 2
Sunil S, Santiago VA, Gougeon L, Warwick K, Okrainec A, Hawa R, Sockalingam S. Predictors of vitamin adherence after bariatric surgery. Obes Surg. 2017;27(2):416–23. https://doi.org/10.1007/s11695-016-2306-x.
Roth AE, Thornley CJ, Blackstone RP. outcomes in bariatric and metabolic surgery: an updated 5-year review. Curr Obes Rep. 2020;9(3):380–9. https://doi.org/10.1007/s13679-020-00389-8.
Courcoulas AP, King WC, Belle SH, Berk P, Flum DR, Garcia L, Gourash W, Horlick M, Mitchell JE, Pomp A, Pories WJ, Purnell JQ, Singh A, Spaniolas K, Thirlby R, Wolfe BM, Yanovski SZ. Seven-year weight trajectories and health outcomes in the longitudinal assessment of bariatric surgery (LABS) Study. JAMA Surg. 2018;153(5):427–34. https://doi.org/10.1001/jamasurg.2017.5025. PMID: 29214306; PMCID: PMC6584318
Viégas M, Vasconcelos RS, Neves AP, Diniz ET, Bandeira F. Bariatric surgery and bone metabolism: a systematic review. Arq Bras Endocrinol Metabol. 2010;54(2):158–63. https://doi.org/10.1590/s0004-27302010000200011.
Bellicha A, van Baak MA, Battista F, Beaulieu K, Blundell JE, Busetto L, Carraça EV, Dicker D, Encantado J, Ermolao A, Farpour-Lambert N, Pramono A, Woodward E, Oppert JM. Effect of exercise training before and after bariatric surgery: a systematic review and meta-analysis. Obes Rev. 2021;22(Suppl 4):e13296. https://doi.org/10.1111/obr.13296. Epub 2021 Jun 3. PMID: 34080281; PMCID: PMC8365633
Funding
This study was partly funded by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES - Finance Code 001) and Research Incentive Fund of the Hospital de Clínicas de Porto Alegre (FIPE). LFS received grants from Programa Especial para Doutorado em Pesquisa Médica (PDE-DPM) by CAPES.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval and Informed Consent
The study was approved by the Research Ethics Committee of HCPA, and data were collected from electronic medical records in accordance with the term of commitment for data use. This term is issued by the participant hospital as a means of certifying the commitment of the researchers in preserving the privacy of patients whose data will be collected in electronic medical records and database of the institution, ensuring that information can only be disclosed anonymously. For this type of study, formal consent is not required, and informed consent does not apply.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Hypovitaminosis D and SHPT are highly prevalent in late post-bariatric patients.
• Micronutrient supplementation seems to be insufficient in preventing bone disease.
• Low BMD is more related to age, sex, and menopausal status in femoral locations.
• Osteometabolic disease post-RYGB should be carefully studied and monitored.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sperb, L.F., Leotti, V.B., Silveiro, S.P. et al. Long-Term Changes in Bone Density and Bone Metabolism After Gastric Bypass Surgery: a Retrospective Cohort Study. OBES SURG 33, 911–919 (2023). https://doi.org/10.1007/s11695-022-06448-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06448-4