Abstract
Background
Fasting during Ramadan is one of the five pillars of the Muslim faith. Despite the positive effects of fasting on health, there are no guidelines or clear recommendations regarding fasting after metabolic/bariatric surgery (MBS). The current study reports the result of a modified Delphi consensus among expert metabolic/bariatric surgeons with experience in managing patients who fast after MBS.
Methods
A committee of 61 well-known metabolic and bariatric surgeons from 24 countries was created to participate in the Delphi consensus. The committee voted on 45 statements regarding recommendations and controversies around fasting after MBS. An agreement/disagreement ≥ of 70.0% was regarded as consensus.
Results
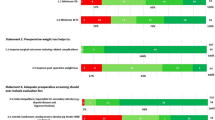
The experts reached a consensus on 40 out of 45 statements after two rounds of voting. One hundred percent of the experts believed that fasting needs special nutritional support in patients who underwent MBS. The decision regarding fasting must be coordinated among the surgeon, the nutritionist and the patient.
At any time after MBS, 96.7% advised stopping fasting in the presence of persistent symptoms of intolerance. Seventy percent of the experts recommended delaying fasting after MBS for 6 to 12 months after combined and malabsorptive procedures according to the patient’s situation and surgeon’s experience, and 90.1% felt that proton pump inhibitors should be continued in patients who start fasting less than 6 months after MBS.
There was consensus that fasting may help in weight loss, improvement/remission of non-alcoholic fatty liver disease, dyslipidemia, hypertension and type 2 diabetes mellitus among 88.5%, 90.2%, 88.5%, 85.2% and 85.2% of experts, respectively.
Conclusion
Experts voted and reached a consensus on 40 statements covering various aspects of fasting after MBS.
Graphical abstract

Similar content being viewed by others
References
Nachvak SM, Pasdar Y, Pirsaheb S, et al. Effects of Ramadan on food intake, glucose homeostasis, lipid profiles and body composition composition. Eur J Clin Nutr. 2019;73(4):594–600.
Urooj A, PaiKotebagilu N, Shivanna LM, et al. Effect of Ramadan fasting on body composition, biochemical profile, and antioxidant status in a sample of healthy individuals. International journal of endocrinology and metabolism. 2020;18(4):e107641.
Osman F, Haldar S, Henry CJ. Effects of time-restricted feeding during Ramadan on dietary intake, body composition and metabolic outcomes. Nutrients. 2020;12(8).
Al-Rawi N, Madkour M, Jahrami H, et al. effect of diurnal intermittent fasting during Ramadan on ghrelin, leptin, melatonin, and cortisol levels among overweight and obese subjects: A prospective observational study. PloS one. 2020;15(8):e0237922.
Mahawar KK, Aggarwal S, Carr WR, et al. Consensus statements and bariatric surgery. Obes Surg. 2015;25(6):1063–5.
Mattson MP, Wan R. Beneficial effects of intermittent fasting and caloric restriction on the cardiovascular and cerebrovascular systems. J Nutr Biochem. 2005;16(3):129–37.
Antoni R, Johnston KL, Collins AL, Robertson MD. Effects of intermittent fasting on glucose and lipid metabolism. Proc Nutr Soc. 2017;76(3):361–8.
Antunes F, Erustes AG, Costa AJ, et al. Autophagy and intermittent fasting: the connection for cancer therapy? Clinics (Sao Paulo, Brazil). 2018;73(suppl 1):e814s.
Al-Ozairi E, Al Kandari J, AlHaqqan D, et al. Obesity surgery and Ramadan: a prospective analysis of nutritional intake, hunger and satiety and adaptive behaviours during fasting. Obes Surg. 2015;25(3):523–9.
Grajower MM, Horne BD. Clinical management of intermittent fasting in patients with diabetes mellitus. Nutrients. 2019;11(4).
Chan F, Slater C, Syed AA. Diabetes and Ramadan. Fasts after bariatric surgery. BMJ (Clinical research ed). 2010;341:c3706.
Benaiges D, Más-Lorenzo A, Goday A, et al. Laparoscopic sleeve gastrectomy: more than a restrictive bariatric surgery procedure? World J Gastroenterol. 2015;21(41):11804–14.
Sweeney TE, Morton JM. Metabolic surgery: action via hormonal milieu changes, changes in bile acids or gut microbiota? A summary of the literature. Best Pract Res Clin Gastroenterol. 2014;28(4):727–40.
Jastrzębska-Mierzyńska M, Ostrowska L, Wasiluk D, et al. Dietetic recommendations after bariatric procedures in the light of the new guidelines regarding metabolic and bariatric surgery. Rocz Panstw Zakl Hig. 2015;66(1):13–9.
Handzlik-Orlik G, Holecki M, Orlik B, et al. Nutrition management of the post-bariatric surgery patient. Nutrition in clinical practice : official publication of the American Society for Parenteral and Enteral Nutrition. 2015;30(3):383–92.
Bettini S, Belligoli A, Fabris R, et al. Diet approach before and after bariatric surgery. Rev Endocr Metab Disord. 2020;21(3):297–306.
Parent B, Martopullo I, Weiss NS, et al. Bariatric Surgery in Women of Childbearing Age, Timing Between an Operation and Birth, and Associated Perinatal Complications. JAMA Surg. 2017;152(2):128–35.
Busetto L, Dicker D, Azran C, et al. Obesity Management Task Force of the European Association for the Study of Obesity Released “Practical Recommendations for the Post-Bariatric Surgery Medical Management.” Obes Surg. 2018;28(7):2117–21.
Di Lorenzo N, Antoniou SA, Batterham RL, et al. Clinical practice guidelines of the European Association for Endoscopic Surgery (EAES) on bariatric surgery: update 2020 endorsed by IFSO-EC. EASO and ESPCOP Surgical endoscopy. 2020;34(6):2332–58.
Shawe J, Ceulemans D, Akhter Z, et al. Pregnancy after bariatric surgery: Consensus recommendations for periconception, antenatal and postnatal care. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2019;20(11):1507–22.
Kalhor M, Malekpour K, Pazouki A, et al. The effects of Islamic fasting on blood biochemical parameters in morbidly obese patients undergone bariatric surgery. 2020:1–5.
Sadiya A, Ahmed S, Siddieg HH, et al. Effect of Ramadan fasting on metabolic markers, body composition, and dietary intake in Emiratis of Ajman (UAE) with metabolic syndrome. Diabetes, metabolic syndrome and obesity : targets and therapy. 2011;4:409–16.
Aloui A, Baklouti H, Souissi N, et al. Effects of Ramadan fasting on body composition in athletes: a systematic review. Tunis Med. 2019;97(10):1087–94.
Gokakin AK, Kurt A, Akgol G, et al. Effects of Ramadan fasting on peptic ulcer disease as diagnosed by upper gastrointestinal endoscopy. Arab journal of gastroenterology : the official publication of the Pan-Arab Association of Gastroenterology. 2012;13(4):180–3.
Kocakusak A. Does Ramadan fasting contribute to the increase of peptic ulcer perforations? Eur Rev Med Pharmacol Sci. 2017;21(1):150–4.
Abdullah A, Peeters A, de Courten M, et al. The magnitude of association between overweight and obesity and the risk of diabetes: a meta-analysis of prospective cohort studies. Diabetes Res Clin Pract. 2010;89(3):309–19.
Omar I, Madhok B, Parmar C, et al. Analysis of national bariatric surgery related clinical incidents: lessons learned and a proposed safety checklist for bariatric surgery. Obes Surg. 2021;31(6):2729–42. https://doi.org/10.1007/s11695-021-05330-z.
Salti I, Bénard E, Detournay B, et al. A population-based study of Diabetes and its characteristics during the fasting month of Ramadan in 13 countries: results of the epidemiology of diabetes and Ramadan 1422/2001 (EPIDIAR) study. Diabetes Care. 2004;27(10):2306–11.
Ahmedani MY, Alvi SF, Haque MS, et al. Implementation of Ramadan-specific diabetes management recommendations: a multi-centered prospective study from Pakistan. J Diabetes Metab Disord. 2014;13(1):37.
Hassanein M, Al-Arouj M, Hamdy O, et al. Diabetes and Ramadan: practical guidelines. Diabetes Res Clin Pract. 2017;126:303–16.
Ahmed SH, Chowdhury TA, Hussain S, et al. Ramadan and diabetes: a narrative review and practice update. Diabetes therapy : research, treatment and education of diabetes and related disorders. 2020:1–44.
Ajabnoor GM, Bahijri S, Borai A, et al. Health impact of fasting in Saudi Arabia during Ramadan: association with disturbed circadian rhythm and metabolic and sleeping patterns. PloS one. 2014;9(5):e96500.
Faris MAE, Jahrami HA, Alhayki FA, et al. Effect of diurnal fasting on sleep during Ramadan: a systematic review and meta-analysis. Sleep & breathing = Schlaf & Atmung. 2020;24(2):771–82.
Lee SWH, Ng KY, Chin WK. The impact of sleep amount and sleep quality on glycemic control in type 2 diabetes: a systematic review and meta-analysis. Sleep Med Rev. 2017;31:91–101.
Khan NN, Siddiqui S, Ali S. Qamar SJJoF, Health. Effect of physical activities and obesity on Ramadan fasting among hypertensive patients. 2016;4(4):156–62.
Mahawar KK, Himpens J, Shikora SA, et al. The first consensus statement on one anastomosis/mini gastric bypass (OAGB/MGB) using a modified Delphi approach. Obes Surg. 2018;28(2):303–12.
Pouwels S, Omar I, Aggarwal S, et al. The first modified Delphi consensus statement for resuming bariatric and metabolic surgery in the COVID-19 times. Obes Surg. 2021;31(1):451–6.
Mahawar KK, Omar I, Singhal R, et al. The first modified Delphi consensus statement on sleeve gastrectomy. Surgical endoscopy. 2021.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
This article does not contain any studies with human participants or animals performed by any of the authors. For this type of study, formal consent is not required.
Informed Consent
Informed consent does not apply.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Fasting is safe after metabolic and bariatric surgery [MBS].
• Fasting needs special nutritional support in patients after MBS.
• Patients after MBS should avoid fasting if they have food intolerance.
• Fasting after MBS helps in weight loss and improvement of obesity-related medical problems.
Rights and permissions
About this article
Cite this article
Kermansaravi, M., Omar, I., Mahawar, K. et al. Religious Fasting of Muslim Patients After Metabolic and Bariatric Surgery: a Modified Delphi Consensus. OBES SURG 31, 5303–5311 (2021). https://doi.org/10.1007/s11695-021-05724-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05724-z