Abstract
Background
Fasting for religious or lifestyle reasons poses a challenge to people who have undergone bariatric surgery. A total fast (abstaining from all forms of nourishment including liquids) during long summer days puts these patients at risk of dehydration and poor calorie and nutrient intake.
Methods
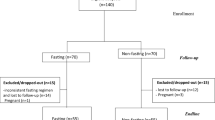
We undertook telephone surveys of 24-h food recall, hunger and satiety scores, medication use, adverse symptoms and depression scores on a fasting day in Ramadan and a non-fasting day subsequently.
Results
We studied 207 participants (166 women) who had undergone sleeve gastrectomy. The mean (standard error) age was 35.2 (0.7) years. Men and women consumed 20.4 % (P = 0.018) and 16.9 % (P < 0.001) fewer calories and 44.8 % (P < 0.001) and 32.4 % (P < 0.001) less protein during fasting, respectively. There was no significant difference in the intake of fluids or incidence of adverse gastrointestinal, hypoglycaemic and sympathoadrenal symptoms. Of participants on pharmacotherapy, 89.5 % took their prescribed medications; 86.3 % made no changes to the doses, but 80.4 % changed the timing of the medications. Both women and men reported feeling less hungry and a preference for savoury foods during Ramadan. There was no difference in depression and work impairment scores.
Conclusions
Fasting was well tolerated in persons who had undergone sleeve gastrectomy. It may be advisable to raise awareness about dietary protein intake and managing medications appropriately during fasting.
Similar content being viewed by others
References
Mohammed N, Ammori BJ, Syed AA. Investigating iron deficiency in the severely obese: challenges and solutions. Br J Hosp Med (Lond). 2012;73(11):606–7. PMID: 23147357.
Eisenberg MJ, Atallah R, Grandi SM, et al. Legislative approaches to tackling the obesity epidemic. CMAJ. 2011;183(13):1496–500. PMID: 21540168.
Bourn J, National Audit Office. Tackling obesity in England. Report by the Comptroller and Auditor General. London: The Stationery Office 2001.
Lau DC, Douketis JD, Morrison KM, et al. 2006 Canadian clinical practice guidelines on the management and prevention of obesity in adults and children. CMAJ. 2007;176(8):1–117. PMID: 17420481.
Tsigos C, Hainer V, Basdevant A, et al. Management of obesity in adults: European clinical practice guidelines. Obes Facts. 2008;1(2):106–16. PMID: 20054170.
NICE clinical guideline 43. Obesity: guidance on the prevention, identification, assessment and management of overweight and obesity in adults and children. London: National Institute for Health and Care Excellence (NICE); 2006.
NHLBI Obesity Education Initiative Expert Panel on the Identification, Evaluation, and Treatment of Obesity in Adults. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. Bethesda (MD): National Heart, Lung, and Blood Institute (NHLBI) in cooperation with the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK); 1998.
SIGN guideline 115. Management of obesity: a national clinical guideline. Edinburgh: Scottish Intercollegiate Guidelines Network (SIGN); 2010.
Plourde G, Prud’homme D. Managing obesity in adults in primary care. CMAJ. 2012;184(9):1039–44. PMID: 22586330.
Picot J, Jones J, Colquitt JL, et al. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technol Assess. 1-190;13(41):1–15-357. iii-iv. PMID: 19726018.
Buchwald H. Consensus conference statement bariatric surgery for morbid obesity: health implications for patients, health professionals, and third-party payers. Surg Obes Relat Dis. 2005;1(3):371–81. PMID: 16925250.
Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013;23(4):427–36. PMID: 23338049.
Bal BS, Finelli FC, Shope TR, et al. Nutritional deficiencies after bariatric surgery. Nat Rev Endocrinol. 2012;8(9):544–56. PMID: 22525731.
Alkandari JR, Maughan RJ, Roky R, et al. The implications of Ramadan fasting for human health and well-being. J Sports Sci. 2012;30 Suppl 1:S9–19. PMID: 22742901.
Trepanowski JF, Bloomer RJ. The impact of religious fasting on human health. Nutr J. 2010;9:57. PMID: 21092212.
Chan F, Slater C, Syed AA. Fasts after bariatric surgery. BMJ. 2010;341:c3706. PMID: 20659987.
Holmstrup ME, Stearns-Bruening K, Rozelle J. Quantifying accurate calorie estimation using the “think aloud” method. J Nutr Educ Behav. 2013;45(1):77–81. PMID: 23141076.
INFOODS. International network of food data systems. Rome: Food and Agriculture Organization of the United Nations; 2014.
Food Standards Agency. McCance and Widdowson’s the composition of foods. Sixth summary ed. Cambridge: Royal Society of Chemistry; 2002.
Flint A, Raben A, Blundell JE, et al. Reproducibility, power and validity of visual analogue scales in assessment of appetite sensations in single test meal studies. Int J Obes Relat Metab Disord. 2000;24(1):38–48. PMID: 10702749.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. PMID: 11556941.
Andreu A, Moize V, Rodriguez L, et al. Protein intake, body composition, and protein status following bariatric surgery. Obes Surg. 2010;20(11):1509–15. PMID: 20820937.
Custodio Afonso Rocha V, Ramos de Arvelos L, Pereira Felix G, et al. Evolution of nutritional, hematologic and biochemical changes in obese women during 8 weeks after Roux-en-Y gastric bypass. Nutr Hosp. 2012;27(4):113–40. PMID: 23165553.
Faria SL, Faria OP, Buffington C, et al. Dietary protein intake and bariatric surgery patients: a review. Obes Surg. 2011;21(11):1798–805. PMID: 21590346.
Sadiya A, Ahmed S, Siddieg HH, et al. Effect of Ramadan fasting on metabolic markers, body composition, and dietary intake in Emiratis of Ajman (UAE) with metabolic syndrome. Diabetes Metab Syndr Obes. 2011;4:409–16. PMID: 22253539.
Moize V, Andreu A, Rodriguez L, Flores L, Ibarzabal A, Lacy A, Jimenez A, Vidal J. Protein intake and lean tissue mass retention following bariatric surgery. Clin Nutr. 2012 Nov 14. PMID: 23200926.
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 update: cosponsored by American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery. Obesity (Silver Spring). 2013;21 Suppl 1:S1–S27. PMID: 23529939.
Rao RS. Bariatric surgery and the central nervous system. Obes Surg. 2012;22(6):967–78. PMID: 22488684.
Acknowledgments
An abstract of this work was presented at the 18th World Congress of the International Federation for the Surgery of Obesity & Metabolic Disorders (IFSO), Istanbul, Turkey 28–31 August 2013 (Obes Surg 2013; 23(8):1221) and published as an electronic letter in bmj.com (http://www.bmj.com/content/341/bmj.c3706/rr/651889).
Conflict of Interest
None of the authors have conflict of interest in relation to this work.
Funding
No special funding.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Al-Ozairi, E., Al Kandari, J., AlHaqqan, D. et al. Obesity Surgery and Ramadan: a Prospective Analysis of Nutritional Intake, Hunger and Satiety and Adaptive Behaviours During Fasting. OBES SURG 25, 523–529 (2015). https://doi.org/10.1007/s11695-014-1373-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-014-1373-0