Abstract
Background
Bariatric surgery is currently the most effective treatment for morbid obesity. These procedures change the gastrointestinal system with the aim of reducing dietary intake. Improving diet quality is essential in maintaining nutritional health and achieving long-term benefits from the surgery. The aim of this systematic review was to examine the relationship between bariatric surgery and diet quality at least 1 year after surgery.
Methods
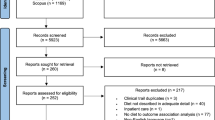
A systematic search of five databases was conducted. Studies were included that reported diet quality, eating pattern, or quality of eating in adult patients who had undergone laparoscopic-adjusted gastric banding (LAGB), Roux-en-Y gastric bypass (RYGB), and sleeve gastrectomy (SG) procedures. Data was extracted to determine the relationship between having had bariatric surgery and subsequent diet quality.
Results
A total of 34 study articles (described in 36 articles) met the inclusion criteria. The majority of studies were observational in nature and showed a reduction in energy intake following surgery, as well as inadequate intakes of micronutrients and protein, and an excessive intake of fats. There was evidence of nutrient imbalances, suboptimal compliance with multivitamin and mineral supplementation, and limited follow-up of patients.
Conclusion
The current evidence base suggests that despite being effective in reducing energy intake, bariatric surgery can result in unbalanced diets, inadequate micronutrient and protein intakes, and excessive intakes of fats. In combination with suboptimal adherence to multivitamin and mineral supplementation, this may contribute to nutritional deficiencies and weight regain. There is a need for high-quality nutrition studies, to identify optimal dietary compositions following bariatric surgery.

Similar content being viewed by others
References
Sjöström L, Lindroos A-K, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351(26):2683–93.
Bavaresco M, Paganini S, Lima TP, et al. Nutritional course of patients submitted to bariatric surgery. Obes Surg. 2010;20(6):716–21. https://doi.org/10.1007/s11695-008-9721-6.
McGrice MA, Porter JA. What are gastric banding patients eating one year post-surgery? Obes Surg. 2012;22(12):1855–8. https://doi.org/10.1007/s11695-012-0741-x.
Brolin RE, Robertson LB, Kenler HA, et al. Weight loss and dietary intake after vertical banded gastroplasty and Roux-en-Y gastric bypass. Ann Surg. 1994;220(6):782–90.
Kruseman M, Leimgruber A, Zumbach F, et al. Dietary, weight, and psychological changes among patients with obesity, 8 years after gastric bypass. Journal of the American Dietetic Association. 2010;110(4):527–34. https://doi.org/10.1016/j.jada.2009.12.028. Language: English. Entry Date: 20100423. Revision Date: 20150819. Publication Type: Journal Article
Freeman RA, Overs SE, Zarshenas N, et al. Food tolerance and diet quality following adjustable gastric banding, sleeve gastrectomy and Roux-en-Y gastric bypass. Obes Res Clin Pract. 2014;8(2):e115–200. https://doi.org/10.1016/j.orcp.2013.02.002.
Gesquiere I, Foulon V, Augustijns P, et al. Micronutrient intake, from diet and supplements, and association with status markers in pre- and post-RYGB patients. Clinical Nutrition (Edinburgh, Scotland). 2017;36(4):1175–81. https://doi.org/10.1016/j.clnu.2016.08.009.
Suter M, Calmes JM, Paroz A, et al. A new questionnaire for quick assessment of food tolerance after bariatric surgery. Obes Surg. 2007;17:2–8.
Cano-Valderrama O, Sánchez-Pernaute A, Rubio-Herrera MA, et al. Long-term food tolerance after bariatric surgery: comparison of three different surgical techniques. Obes Surg. 2017;27(11):2868–72. https://doi.org/10.1007/s11695-017-2703-9.
Kafri N, Valfer R, Nativ O, et al. Health behavior, food tolerance, and satisfaction after laparoscopic sleeve gastrectomy. Surgery for obesity and related diseases : official journal of the American Society for Bariatric Surgery. 2011;7(1):82–8. https://doi.org/10.1016/j.soard.2010.09.016.
Freire RH, Borges MC, Alvarez-Leite JI, et al. Food quality, physical activity, and nutritional follow-up as determinant of weight regain after Roux-en-Y gastric bypass. Nutrition (Burbank, Los Angeles County, Calif). 2012;28(1):53–8. https://doi.org/10.1016/j.nut.2011.01.011.
Soares FL, Bissoni de Sousa L, Corradi-Perini C, et al. Food quality in the late postoperative period of bariatric surgery: an evaluation using the bariatric food pyramid. Obes Surg. 2014;24(9):1481–6. https://doi.org/10.1007/s11695-014-1198-x.
Aills L, Blankenship J, Buffington C, et al. Bariatric nutrition: suggestions for the surgical weight loss patient. Surg Obes Relat Dis. 2008;4(5):S73–S108.
Kanerva N, Larsson I, Peltonen M, et al. Changes in total energy intake and macronutrient composition after bariatric surgery predict long-term weight outcome: findings from the Swedish Obese Subjects (SOS) study. Am J Clin Nutr. 2017;106(1):136–45. https://doi.org/10.3945/ajcn.116.149112.
Moizé V, Pi-Sunyer X, Mochari H, et al. Nutritional pyramid for post-gastric bypass patients. Obes Surg. 2010;20:1133–41.
Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and metaanalyses: the PRISMA statement. BMJ (Clinical Research ed). 2009;339:b2535. https://doi.org/10.1136/bmj.b2535.
de Torres Rossi RG, Dos Santos MT, de Souza FI, et al. Nutrient intake of women 3 years after Roux-en-Y gastric bypass surgery. Obes Surg. 2012;22(10):1548–53. Epub 2012/06/13. https://doi.org/10.1007/s11695-012-0688-y.
ADA. American Dietetics Association. Evidence analysis manual: steps in ADA evidence analysis process. Chicago: Scientific Affairs and Research; 2010. p. 43–8.
NHMRC. National Health and Medical Research Council. Levels of evidence and grades for recommendations for developers of guidelines. Commonwealth of Australia.: Canberra; 2009.
Dagan S, Keidar A, Raziel A, et al. Do bariatric patients follow dietary and lifestyle recommendations during the first postoperative year? Obesity Surgery. 2017;27(9):2258–71. https://doi.org/10.1007/s11695-017-2633-6.
Novais PF, Rasera Jr I, Leite CV, et al. Food intake in women two years or more after bariatric surgery meets adequate intake requirements. Nutrition Research. 2012;32(5):335–41. https://doi.org/10.1016/j.nutres.2012.03.016.
Novais PF, Junior IR, Shiraga EC, et al. Food aversions in women during the 2 years after Roux-en-Y gastric bypass. Obes Surg. 2011;21(12):1921–7. https://doi.org/10.1007/s11695-010-0342-5.
Leiro LS, Melendez-Araújo MS. Diet micronutrient adequacy of women after 1 year of gastric bypass. Arquivos Brasileiros de Cirurgia Digestiva. 2014;27 Suppl 1:21–5.
Dias MC, Ribeiro AG, Scabim VM, et al. Dietary intake of female bariatric patients after anti-obesity gastroplasty. Clinics. 2006;61(2):93–8.
Benson-Davies S, Davies ML, Kattelmann K. Food preferences in patients after Roux-en Y gastric bypass surgery: a pilot study examining eating behaviors and weight maintenance. Topics in Clinical Nutrition. 2013;28(1):8–14. Language: English. Entry Date: 20130614. Revision Date: 20150818. Publication Type: Journal Article
Moize V, Geliebter A, Gluck ME, et al. Obese patients have inadequate protein intake related to protein intolerance up to 1 year following Roux-en-Y gastric bypass. Obes Surg. 2003;13(1):23–8.
McGrice MA, Porter JA. The micronutrient intake profile of a multicentre cohort of Australian LAGB patients. Obes Surg. 2014;24(3):400–4. https://doi.org/10.1007/s11695-013-1101-1.
Coluzzi I, Raparelli L, Guarnacci L, et al. Food intake and changes in eating behavior after laparoscopic sleeve gastrectomy. Obes Surg. 2016;26(9):2059–67. https://doi.org/10.1007/s11695-015-2043-6.
Chou JJ, Lee WJ, Almalki O, et al. Dietary intake and weight changes 5 years after laparoscopic sleeve gastrectomy. Obes Surg. 2017;27(12):3240–6. https://doi.org/10.1007/s11695-017-2765-8.
Verger EO, Aron-Wisnewsky J, Dao MC, et al. Micronutrient and protein deficiencies after gastric bypass and sleeve gastrectomy: a 1-year follow-up. Obes Surg. 2016;26(4):785–96. https://doi.org/10.1007/s11695-015-1803-7.
Moizé V, Andreu A, Flores L, et al. Long-term dietary intake and nutritional deficiencies following sleeve gastrectomy or Roux-en-Y gastric bypass in a Mediterranean population. Journal of the Academy of Nutrition & Dietetics. 2013;113(3):400–10. https://doi.org/10.1016/j.jand.2012.11.017. Language: English. Entry Date: 20130627. Revision Date: 20150711. Publication Type: Journal Article
El Labban S, Safadi B, Olabi A. The effect of Roux-en-Y gastric bypass and sleeve gastrectomy surgery on dietary intake, food preferences, and gastrointestinal symptoms in post-surgical morbidly obese Lebanese subjects: a cross-sectional pilot study. Obesity surgery. 2015;25(12 // (AUB) *American University of Beirut*):2393–9. https://doi.org/10.1007/s11695-015-1713-8.
Harbottle L. Audit of nutritional and dietary outcomes of bariatric surgery patients. Obesity Reviews: An Official Journal Of The International Association For The Study Of Obesity. 2011;12(3):198–204. https://doi.org/10.1111/j.1467-789X.2010.00737.x.
Ernst B, Thurnheer M, Wilms B, et al. Differential changes in dietary habits after gastric bypass versus gastric banding operations. Obesity Surgery. 2009;19(3):274–80.
Ortega J, Ortega-Evangelio G, Cassinello N, et al. What are obese patients able to eat after Roux-en-Y gastric bypass? Obesity facts. 2012;5(3):339–48. https://doi.org/10.1159/000339769.
Coughlin K, Bell RM, Bivins BA, et al. Preoperative and postoperative assessment of nutrient intakes in patients who have undergone gastric bypass surgery. Archives of Surgery (Chicago, Ill: 1960). 1983;118(7):813–6.
Warde-Kamar J, Rogers M, Flancbaum L, et al. Calorie intake and meal patterns up to 4 years after Roux-en-Y gastric bypass surgery. Obes Surg. 2004;14(8):1070–9. https://doi.org/10.1381/0960892041975668.
da Silva FB, Gomes DL, de Carvalho KM. Poor diet quality and postoperative time are independent risk factors for weight regain after Roux-en-Y gastric bypass. Nutrition (Burbank, Los Angeles County, Calif). 2016;32(11–12):1250–3. https://doi.org/10.1016/j.nut.2016.01.018.
Giusti V, Theytaz F, Di Vetta V, et al. Energy and macronutrient intake after gastric bypass for morbid obesity: a 3-y observational study focused on protein consumption. American Journal of Clinical Nutrition. 2016;103(1):18–24. https://doi.org/10.3945/ajcn.115.111732. Language: English. Entry Date: 20160115. Revision Date: 20160429. Publication Type: Article.
Laurenius A, Larsson I, Melanson KJ, et al. Decreased energy density and changes in food selection following Roux-en-Y gastric bypass. Eur J Clin Nutr. 2013;67(2):168–73. https://doi.org/10.1038/ejcn.2012.208.
Miller GD, Norris A, Fernandez A. Changes in nutrients and food groups intake following laparoscopic Roux-en-Y gastric bypass (RYGB). Obes Surg. 2014;24(11):1926–32. https://doi.org/10.1007/s11695-014-1259-1.
Reid RE, Oparina E, Plourde H, et al. Energy intake and food habits between weight maintainers and regainers, five years after Roux-en-Y gastric bypass. Canadian journal of dietetic practice and research. 2016;77(4):195–8. https://doi.org/10.3148/cjdpr-2016-013. Language: English. Entry Date: 20161121. Revision Date: 20161129. Publication Type: Article
NHMRC. Natonal Health and Medical Research Council. Departmnet of Health and Aging. Australian dietary guidelines: eat for health. 2013:https://www.eatforhealth.gov.au/sites/default/files/files/the_guidelines/n55_australian_dietary_guidelines.pdf.
Angarisani L, Santonicola A, Iovino P, et al. Bariatric surgery worldwide 2013. Obes Surg. 2015;25:1822–32.
Colquitt JL, Pickett K, Loveman E, et al. Surgery for weight loss in adults. Cochrane Database Syst Rev. 2014;8:1–244.
Goris A, Westerterp-Plantenga M, Westerterp KR. Undereating and underrecording of habitual food intake in obese men: selective underreporting of fat intake. Am J Clin Nutr. 2000;17:130–4.
Harbury CM, Verbruggen EE, Callister R, et al. What do individuals with morbid obesity report as a usual dietary intake? A narrative review of available evidence. Clin Nutr. 2016;13:15–22.
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Endocrine Practice. 2013;19(2):337–72. https://doi.org/10.4158/ep12437.Gl.
Parrott J, Frank L, Rabena R, et al. American Society for Metabolic and Bariatric Surgery integrated health nutritional guidelines for the surgical weight loss patient. Surgery for Obesity and Related Diseases. 2016;13:727–41.
le Roux CW, Bueter M, Theis N, et al. Gastric bypass reduces fat intake and preference. American Journal Of Physiology Regulatory, Integrative and Comparative Physiology. 2011;301(4):R1057–66. https://doi.org/10.1152/ajpregu.00139.2011.
Miras AD, Jackson RN, Jackson SN, et al. Gastric bypass surgery for obesity decreases the reward value of a sweet-fat stimulus as assessed in a progressive ratio task. American Journal of Clinical Nutrition. 2012;96(3):467–73. https://doi.org/10.3945/ajcn.112.036921.
Odstrcil EA, Martinez JG, Santa Ana CA, et al. The contribution of malabsorption to the reduction in net energy absorption after long-limb Roux-en-Y gastric bypass. American Journal of Clinical Nutrition. 2010;92(4):704–13. https://doi.org/10.3945/ajcn.2010.29870. Language: English. Entry Date: 20101119. Revision Date: 20151008. Publication Type: Journal Article.
Zarshenas N, Nacher M, Loi KW, et al. Investigating nutritional deficiencies in a group of patients 3 years post laparoscopic sleeve gastrectomy. Obes Surg. 2016;26(12):2936–43.
Toh SY, Zarshenas N, Jorgensen J. Prevalence of nutrient deficiencies in bariatric patients. Nutrition (Burbank, Los Angeles County, Calif). 2009;25(11–12):1150–6. https://doi.org/10.1016/j.nut.2009.03.012.
Dodsworth A, Warren-Forward H, Baines S. A systematic review of dietary intake after laparoscopic adjustable gastric banding. Journal Of Human Nutrition And Dietetics. 2011;24:327–41.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval and Informed Consent
Not applicable to the study design.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
The search terms used in Scopus were as follows:
((TITLE-ABS-KEY (“bariatric surgery”) OR TITLE-ABS-KEY (“sleeve gastrectomy”) OR TITLE-ABS-KEY (“gastric banding”) OR TITLE-ABS-KEY (“gastric bypass”) OR TITLE-ABS-KEY (“roux-en-y gastric bypass”))) AND ((TITLE-ABS-KEY (“meal pattern”) OR TITLE-ABS-KEY (“diet quality”) OR TITLE-ABS-KEY (diet*) OR TITLE-ABS-KEY (“food groups”) OR TITLE-ABS-KEY (nutri* ) ) ) AND (LIMIT TO (DOCTYPE, “ar”) OR LIMIT-TO (DOCTYPE, “re” ) ) AND (LIMIT-TO (SUBJAREA, “MEDI”) OR LIMIT-TO (SUBJAREA, “NURS”) OR LIMIT-TO (SUBJAREA, “NEUR”) OR LIMIT-TO (SUBJAREA, “PSYC”) OR LIMIT-TO (SUBJAREA, “HEAL”) OR LIMIT-TO (SUBJAREA, “SOCI” ) ) AND (LIMIT-TO (LANGUAGE, “English” ) ) AND (EXCLUDE (EXACTKEYWORD, “Animals”) OR EXCLUDE (EXACTKEYWORD, “Animal Experiment”) OR EXCLUDE (EXACTKEYWORD, “Animal”) OR EXCLUDE (EXACTKEYWORD, “Child”) OR EXCLUDE (EXACTKEYWORD, “Rat”) OR EXCLUDE (EXACTKEYWORD, “Animal Model” ) ) AND (EXCLUDE (EXACTKEYWORD, “Adolescent”) OR EXCLUDE (EXACTKEYWORD, “Nonhuman”) OR EXCLUDE (EXACTKEYWORD, “Sibutramine”) OR EXCLUDE (EXACTKEYWORD, “Unclassified Drug”) OR EXCLUDE (EXACTKEYWORD, “Pregnancy”) OR EXCLUDE (EXACTKEYWORD, “Adipose Tissue”) OR EXCLUDE (EXACTKEYWORD, “Antiobesity Agent” ) )
Rights and permissions
About this article
Cite this article
Zarshenas, N., Tapsell, L.C., Neale, E.P. et al. The Relationship Between Bariatric Surgery and Diet Quality: a Systematic Review. OBES SURG 30, 1768–1792 (2020). https://doi.org/10.1007/s11695-020-04392-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04392-9