Abstract
Objective
To evaluate the impact of laparoscopic sleeve gastrectomy (LSG) or laparoscopic Roux-en-Y gastric bypass (LRYGB) on gastroesophageal reflux disease (GERD) in patients with obesity.
Methods
Patients with class II or III obesity were treated with LSG or LRYGB. Procedure choice was based on patients and surgeon preferences. GERD symptoms, endoscopy, barium swallow X-ray, esophageal manometry, and 24-h pH monitoring were obtained before and 1 year after surgery.
Results
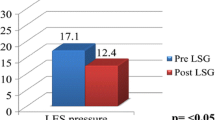
Seventy-five patients underwent surgery (83% female, 39.3 ± 12.1 years, BMI of 41.5 ± 5.1 kg/m2): 35 (46.7%) had LSG and 40 (53.3%) LRYGB. LSG patients had lower BMI (40.3 ± 4.0 kg/m2 vs. 42.7 ± 5.7 kg/m2; p = 0.041) and trend toward lower prevalence of GERD (20% vs. 40%; p = 0.061). One year after surgeries, GERD was more frequent in LSG patients (74% vs. 25%; p < 0.001) and all LSG patients with preoperative GERD continue to have GERD postoperatively. De novo GERD occurred in 19 of 28 (67.9%) of LSG patients and 4 of 24 (16.7%) patients treated with LRYGB (OR 10.6, 95%CI 2.78–40.1). Independent predictors for post-operative GERD were as follows: LSG (OR 12.3, 95%CI 2.9–52.5), preoperative esophagitis (OR 8.5, 95% CI 1.6–44.8), and age (OR 2.0, 95%CI 1.1–3.4).
Conclusions
One year after surgery, persistent or de novo GERD were substantially more frequent in patients treated with LSG compared with LRYGB. LSG was the strongest predictor for GERD in our trial. Preoperative counseling and choice of bariatric surgical options must include a detailed assessment and discussion of GERD-related surgical outcomes.

Similar content being viewed by others
References
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient--2013 update: cosponsored by American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery. Obesity (Silver Spring). 2013;21(Suppl 1):S1–27.
Hampel H, Abraham NS, El-Serag HB. Meta-analysis: obesity and the risk for gastroesophageal reflux disease and its complications. Ann Intern Med. 2005;143:199–211.
Madalosso CA, Fornari F, Callegari-Jacques SM, et al. Performance of the Montreal Consensus in the diagnosis of gastroesophageal reflux disease in morbidly obese patients. Obes Surg. 2008;18:668–74.
Madalosso CA, Gurski RR, Callegari-Jacques SM, et al. The impact of gastric bypass on gastroesophageal reflux disease in morbidly obese patients. Ann Surg. 2016;263:110–6.
Soricelli E, Casella G, Baglio G, et al. Lack of correlation between gastroesophageal reflux disease symptoms and esophageal lesions after sleeve gastrectomy. Surg Obes Relat Dis. 2018;14:751–6.
Gyawali CP, Kahrilas PJ, Savarino E, et al. Modern diagnosis of GERD: the Lyon Consensus. Gut. 2018;67:1351–62.
Nelson LG, Gonzalez R, Haines K, et al. Amelioration of gastroesophageal reflux symptoms following Roux-en-Y gastric bypass for clinically significant obesity. Am Surg. 2005;71:950–3. discussion 953-4
Madalosso CA, Gurski RR, Callegari-Jacques SM, et al. The impact of gastric bypass on gastroesophageal reflux disease in patients with morbid obesity: a prospective study based on the Montreal Consensus. Ann Surg. 2010;251:244–8.
Frezza EE, Ikramuddin S, Gourash W, et al. Symptomatic improvement in gastroesophageal reflux disease (GERD) following laparoscopic Roux-en-Y gastric bypass. Surg Endosc. 2002;16:1027–31.
Merrouche M, Sabate JM, Jouet P, et al. Gastro-esophageal reflux and esophageal motility disorders in morbidly obese patients before and after bariatric surgery. Obes Surg. 2007;17:894–900.
Varela JE, Nguyen NT. Laparoscopic sleeve gastrectomy leads the U.S. utilization of bariatric surgery at academic medical centers. Surg Obes Relat Dis. 2015;11:987–90.
Borbely Y, Schaffner E, Zimmermann L, et al. De novo gastroesophageal reflux disease after sleeve gastrectomy: role of preoperative silent reflux. Surg Endosc. 2019;33:789–93.
Howard DD, Caban AM, Cendan JC, et al. Gastroesophageal reflux after sleeve gastrectomy in morbidly obese patients. Surg Obes Relat Dis. 2011;7:709–13.
Barr AC, Frelich MJ, Bosler ME, et al. GERD and acid reduction medication use following gastric bypass and sleeve gastrectomy. Surg Endosc. 2017;31:410–5.
Burgerhart JS, Schotborgh CA, Schoon EJ, et al. Effect of sleeve gastrectomy on gastroesophageal reflux. Obes Surg. 2014;24:1436–41.
Braghetto I, Csendes A. Prevalence of Barrett’s esophagus in bariatric patients undergoing sleeve gastrectomy. Obes Surg. 2016;26:710–4.
Sebastianelli L, Benois M, Vanbiervliet G, et al. Systematic endoscopy 5 years after sleeve gastrectomy results in a high rate of Barrett’s esophagus: results of a multicenter study. Obes Surg. 2019;
Yehoshua RT, Eidelman LA, Stein M, et al. Laparoscopic sleeve gastrectomy--volume and pressure assessment. Obes Surg. 2008;18:1083–8.
Braghetto I, Lanzarini E, Korn O, et al. Manometric changes of the lower esophageal sphincter after sleeve gastrectomy in obese patients. Obes Surg. 2010;20:357–62.
Mion F, Tolone S, Garros A, et al. High-resolution impedance manometry after sleeve gastrectomy: increased intragastric pressure and reflux are frequent events. Obes Surg. 2016;26:2449–56.
Fornari F, Gruber AC, Lopes Ade B, et al. Symptom’s questionnaire for gastroesophageal reflux disease. Arq Gastroenterol. 2004;41:263–7.
Lundell LR, Dent J, Bennett JR, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999;45:172–80.
Ott DJ, Gelfand DW, Chen YM, et al. Predictive relationship of hiatal hernia to reflux esophagitis. Gastrointest Radiol. 1985;10:317–20.
Kahrilas PJ, Kim HC, Pandolfino JE. Approaches to the diagnosis and grading of hiatal hernia. Best Pract Res Clin Gastroenterol. 2008;22:601–16.
Levine MS, Rubesin SE. Diseases of the esophagus: diagnosis with esophagography. Radiology. 2005;237:414–27.
Felsenreich DM, Kefurt R, Schermann M, et al. Reflux, sleeve dilation, and Barrett’s esophagus after laparoscopic sleeve gastrectomy: long-term follow-up. Obes Surg. 2017;27:3092–101.
Boru CE, Greco F, Giustacchini P, et al. Short-term outcomes of sleeve gastrectomy conversion to R-Y gastric bypass: multi-center retrospective study. Langenbeck's Arch Surg. 2018;403:473–9.
Salminen P, Helmio M, Ovaska J, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss at 5 years among patients with morbid obesity: the SLEEVEPASS Randomized Clinical Trial. JAMA. 2018;319:241–54.
Jaffin BW, Knoepflmacher P, Greenstein R. High prevalence of asymptomatic esophageal motility disorders among morbidly obese patients. Obes Surg. 1999;9:390–5.
Galvez-Valdovinos R, Cruz-Vigo JL, Marin-Santillan E, et al. Cardiopexy with ligamentum teres in patients with hiatal hernia and previous sleeve gastrectomy: an alternative treatment for gastroesophageal reflux disease. Obes Surg. 2015;25:1539–43.
Kahrilas PJ, Wu S, Lin S, et al. Attenuation of esophageal shortening during peristalsis with hiatus hernia. Gastroenterology. 1995;109:1818–25.
Edmundowicz SA, Clouse RE. Shortening of the esophagus in response to swallowing. Am J Phys. 1991;260:G512–6.
Pouderoux P, Lin S, Kahrilas PJ. Timing, propagation, coordination, and effect of esophageal shortening during peristalsis. Gastroenterology. 1997;112:1147–54.
Garg H, Vigneshwaran B, Aggarwal S, et al. Impact of concomitant laparoscopic sleeve gastrectomy and hiatal hernia repair on gastro-oesophageal reflux disease in morbidly obese patients. J Minim Access Surg. 2017;13:103–8.
Mejia-Rivas MA, Herrera-Lopez A, Hernandez-Calleros J, et al. Gastroesophageal reflux disease in morbid obesity: the effect of Roux-en-Y gastric bypass. Obes Surg. 2008;18:1217–24.
Tai CM, Lee YC, Wu MS, et al. The effect of Roux-en-Y gastric bypass on gastroesophageal reflux disease in morbidly obese Chinese patients. Obes Surg. 2009;19:565–70.
Johnson DA, Fennerty MB. Heartburn severity underestimates erosive esophagitis severity in elderly patients with gastroesophageal reflux disease. Gastroenterology. 2004;126:660–4.
Flora Filho R, Zilberstein B. Reflux esophagitis and gastroesophageal reflux disease: a cross-sectional study of gastroesophageal reflux disease patients by age group. Rev Hosp Clin Fac Med Sao Paulo. 1999;54:61–7.
Wang Y, Yi XY, Gong LL, et al. The effectiveness and safety of laparoscopic sleeve gastrectomy with different sizes of bougie calibration: a systematic review and meta-analysis. Int J Surg. 2018;49:32–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Statement and Consent Statement
The Ethical Committee of the University of Passo Fundo (RS, Brazil) approved this study (number 46976715.5.0000.5342) in accordance with the Helsinki declaration and Brazilian federal regulation. This study is registered at ClinicalTrials.gov under the record number NCT03692455. Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Navarini, D., Madalosso, C.A.S., Tognon, A.P. et al. Predictive Factors of Gastroesophageal Reflux Disease in Bariatric Surgery: a Controlled Trial Comparing Sleeve Gastrectomy with Gastric Bypass. OBES SURG 30, 1360–1367 (2020). https://doi.org/10.1007/s11695-019-04286-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-04286-5