Abstract
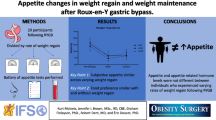
The Roux-Y gastric bypass (RYGBP) is an effective weight-reducing procedure but the involved mechanisms of action are obscure. The Roux limb is the intestinal segment that following surgery is the primary recipient for food intake. The aims of the study were to explore the mechanosensory and biomechanical properties of the Roux limb and to make correlations with preferred meal size. Ten patients participated and were examined preoperatively, 6 weeks and 1 year after RYGBP. Each subject ingested unrestricted amounts of a standardized meal and the weight of the meal was recorded. On another study day, the Roux limb was subjected to gradual distension by the use of an intraluminal balloon. Luminal volume–pressure relationships and thresholds for induction of sensations were monitored. At 6 weeks and 1 year post surgery, the subjects had reduced their meal sizes by 62% and 41% (medians), respectively, compared to preoperative values. The thresholds for eliciting distension-induced sensations were strongly and negatively correlated to the preferred meal size. Intraluminal pressure during Roux limb distension, both at low and high balloon volumes, correlated negatively to the size of the meal that the patients had chosen to eat. The results suggest that the Roux limb is an important determinant for regulating food intake after Roux-Y bypass bariatric surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The exceptional effectiveness of bariatric surgery to treat morbid obesity has highlighted the central role of the gastrointestinal tract in the regulation of body weight and metabolism [1, 2]. However, the mechanisms of action behind the altered food intake and improved metabolic control following surgery are still not completely cleared out. Weight-reducing surgical interventions were originally based on the simple principle of preventing nutrients to be digested or to be absorbed by the intestines. This could be achieved either by restricting food intake or by inducing a condition of intestinal malabsorption. The former principle is represented by, e.g. gastric banding procedures and the latter by intestinal diversion or shunt constructions. The Roux-Y gastric bypass (RYGBP) is a surgical intervention of particular interest because it has been claimed to combine restrictive and malabsorptive effects. Interestingly, patients with RYGBP not only reduce food intake but also convert their ingestive behavior towards a more optimal diet including for example fat aversion [3]. This is in contrast to true restrictive procedures, e.g., vertical band gastroplasty, where patients tend to choose a less healthy diet, i.e., fatty and carbohydrate-rich food [3, 4]. The mechanisms behind the reduced caloric intake including optimized dietary preferences following RYGBP are still enigmatic despite recent findings on the role of gastrointestinal hormones [5, 6]. Furthermore, it remains controversial to what extent the size of the gastric pouch that is in continuity with the jejunal segment (the Roux limb), or restriction at the connecting stoma, influence food intake and subsequent weight reduction [7–11]. The Roux limb per se as a possible point of action for the successful outcome from RYGBP has been investigated very rarely. The objective of the present study was therefore to explore the mechanosensory and biomechanical properties of the Roux limb in relation to food intake. More specifically, the present study explores if there exists an association between an individual’s preferred meal size and threshold for perceived sensations as well as the volume–pressure relationship of the Roux limb following balloon inflation.
Materials and Methods
Study Subjects
Patients on the waiting list for laparoscopic RYGBP were asked for voluntary participation in the study. The operative RYGBP technique included an antecolic–antegastric Roux-en-Y construction with a 10- to 20-ml gastric pouch as described in detail elsewhere [12, 13]. Altogether, ten patients (age 33 to 50 years; eight females) were enrolled and completed the protocol. All participants were non-smokers and no significant preoperative co-morbidity was allowed.
The study was performed according to the principles for experimentation with human beings as defined in the Declaration of Helsinki. The study protocol received approval from the Regional Ethical Review Board in Gothenburg (Dnr: S 674-03), and all subjects were informed about the experimental procedures and signed an informed consent form.
Investigational Procedures
All subjects underwent a preoperative study day where baseline characteristics were recorded including the results of a test meal (see Study Day A below). After surgery, the subjects participated at another two occasions, 6 weeks and 12 months post surgery, and each occasion included two study days with meal ingestion and Roux limb distension, respectively, in random order and separated by at least 1 week.
Study Day A—Meal Ingestion
The subjects arrived at the laboratory in the morning after a standardized light breakfast (consisting of one small sandwich and one glass of milk or fruit juice). They were supplied with a fore-arm venous cannula for blood sampling (data not given in this paper) and were then allowed to wait during fasting conditions over 2 to 3 h. During this time, the subjects scored feelings of hunger and satiety (data not given). The subjects were then exposed to 375 g (6 weeks) or 750 g (preop and at 1 year) hash, i.e., a mixture of meat, potatoes and onions with 150 kcal/100 g, 16 energy% protein, 42 energy% carbohydrate and 42 energy% fat. The subjects were instructed to serve themselves and eat until satisfied. Time from start to stop of ingestion was measured, as well as the weight of remaining food. Small amounts of water were allowed during ingestion, but were not included in the analysis.
Study Day B—Roux Limb Distension
This examination was performed after an overnight fast. The subject rested in a comfortable semi-recumbent position. A multi-lumen PVC catheter (modified Zinectics tube, Synmed AB, Stockholm, Sweden) was inserted nasogastrically and placed with its tip in the descending part of the Roux limb (Fig. 1). The catheter included eight separate channels with corresponding side holes positioned 20 mm apart with the most distal side hole 5 cm from the distal end of the tube. A latex balloon with a length of 35 mm was positioned at the very distal end of the catheter and was connected to the central channel that in turn was used for in- and exsufflation of air and recording intraballoon pressure. The position of the balloon in the Roux limb was standardized to be 8–10 cm below the gastro-enteroanastomosis by utilizing measurements of transmucosal potential difference (TMPD) as follows: The eight side holes positioned oral to the balloon were each connected to pressure transducers for motility recordings (see below). The tube channels were separately fed with a low flow of 150 mM NaCl (3 mL h−1), and each pressure recording line (thus electrically isolated from each other) was used as an electrode for electrical potential recording via an Ag/AgCl bridge connected to a high-impedance voltmeter with a reference electrode positioned subcutaneously. Thus, both the intraluminal hydrostatic pressure and TMPD at each side hole were displayed on-line and stored on a Macintosh personal computer (Apple Computers, CA, USA) using specially designed software (Labview, National instruments, Austin, TX, USA). The side hole recordings allowed identification of the gastro-enteroanastomosis as a clearcut step-down in TMPD from the esophagogastric values being typically 10 to 30 mV (lumen negative), to intestinal values of typically 2 to 4 mV in the Roux limb.
Protocol
After that the balloon had been correctly positioned in the Roux limb, the subjects were left for 30 min to allow baseline motility conditions to be established as assessed by the esophago-gastro-Roux manometric recording. Fasting motility conditions are commonly referred to as the migrating motility complexes (MMC) and defined into three or four phases [14]. The occurrence of MMC in patients that have undergone bariatric surgery has not been completely elucidated, and in order to standardize experimental conditions, the balloon distensions were conducted during phase II-like conditions (irregular contractions with a frequency of more than 2 contractions per 10 min). The balloon was repeatedly inflated over 2 min with gradually increasing volumes and complete emptying in between. The starting volume was 20 mL and was then consecutively increased by 7.5 mL to maximal 72.5 mL. Within this interval of volumes, mainly the diameter increased upon air inflation and the balloon maintained a cylindrical shape with an almost constant length. At each level of inflation, the subject was asked to report perception of sensation with regard to type, location, and intensity (visual analog scale (VAS) 0 to 10). The subjects were instructed to indicate unspecific, non-pain sensations in the interval between 0 and 5 and painful sensations equal to or above 5. The inflation sequence was interrupted if the induced sensation was not tolerable. At least 3 min of rest was allowed between each inflation procedure. The next inflation was performed if baseline motor conditions were present as defined by the manometric recording. After extubation, the balloon was again filled with the same amounts of air, and intraballoon pressure was recorded at each level of inflation for correction of inborn compliance of the balloon where intraluminal pressure is equal to recorded intraballoon pressure minus corresponding balloon pressure in surrounding atmosphere.
Statistics
All included individuals acted as their own controls. Friedman test was employed to identify differences over time and Wilcoxon’s test was used for paired comparisons. Correlations were evaluated using Pearson's product moment correlational analysis. A p value ≤ 0.05 was considered to be of statistical significance. All analyses were performed using the SPSS17 software package (SPSS, Chicago, IL, USA).
Results
Body Mass Index and Preferred Meal Size
As expected, all patients reduced their body mass index (BMI) following surgery with a group median of minus 13% (range −11% to −18%) and minus 33% (range −20% to −44%) at 6 weeks and 1 year, respectively (Fig. 2, upper panel). Following the Roux-Y gastric bypass surgery, nine out of ten patients served themselves and ingested less of the exposed test meal at both 6 weeks (median reduction −62%, p = 0.007) and 1 year (median reduction −41%, p = 0.009) postoperatively compared to before operation (Fig. 2, lower panel).
Balloon Distension Volume–Pressure Relationships
Inflation of air into the Roux limb-located balloon resulted in a corresponding increased intraluminal pressure. These volume–pressure relationships did not differ significantly between 6 weeks and 1 year, respectively (Fig. 3). All patients accepted the start volume (20 mL), and seven out of ten patients fulfilled the distension protocol to the maximal volume of 72.5 mL. Two patients declared both at the 6-week and 1-year visits that the Roux limb distensions induced such unpleasant abdominal sensations that the distensions had to be terminated before reaching the maximal volume.
Thresholds for Distension-Induced Sensations
Perceived sensations in association with the distension-protocol varied considerably between individuals. In general non-pain sensations were reported as unspecific feelings of bloating/distension, hunger, mild discomfort, etc. Painful sensations could for example be reported as an ache or a sudden sharp pain that then turned into an unpleasant but not painful sensation. It was thus difficult for the study participants to differentiate between the non-pain (VAS < 5) and painful (VAS ≥ 5) sensations. It follows that there was no clear difference between the threshold pressure for induction of non-pain and pain sensations (Table 1).
A negative association was found between meal size and thresholds for abdominal sensation following Roux limb distension (analyzed only with regard to non-pain sensations) both at 6 weeks (r = −0.81, p = 0.008; Fig. 4) and at 1 year (r = −0.695, p = 0.038, data not shown in figure) after the RYGBP operation.
Meal Size Versus Roux Limb Distension-Induced Intraluminal Pressure
As can be seen in Fig. 3, there was a non-linear relationship between balloon volumes and recorded intraluminal pressure. For the sake of simplicity, the two extreme points on each volume–pressure curve were chosen for further analyses: (1) the intraluminal pressure at baseline (i.e., the recorded pressure during a balloon volume of 20 mL) and (2) the highest intraluminal pressure recorded for each individual (being the pressure either at the highest tolerable balloon volume, or the maximal volume 72.5 mL, depending on if the subject allowed a full distension protocol or not).
Interestingly, 6 weeks after surgery, the preferred meal size correlated closely to baseline intraluminal pressure (Pearson’s correlation coefficient r = −0.835, p = 0.03; Fig. 5a) as well as to the highest intraluminal pressure recorded for each individual (Pearson’s correlation coefficient r = −0.922, p < 0.001; Fig. 5b). A similar picture was obtained at 1 year postoperatively with correlation coefficient (r) for baseline pressure being −0.596 (p = 0.069) and for the highest recorded pressure −0.926 (p < 0.001) (data not shown in figure).
Discussion
Roux-en-Y gastric bypass is a bariatric construction where a small gastric pouch is connected to the mid-jejunum leaving most of the stomach, the duodenum, as well as proximal jejunum unloaded from the passage of food. RYGBP is very effective for achieving maintained weight reduction by lowering energy intake. The energy intake is the function of the amount of ingested food, the energy density of the food, and meal frequency. In the present study, we report that the size (weight) of a voluntary chosen meal with standardized composition is radically reduced in individuals that have undergone RYGBP.
It is controversial to what extent the weight reduction following RYGBP is dependent on a restrictive property in addition to other mechanisms related to bypass construction. The term restrictive bariatric surgery is commonly referred to the narrowing of the stomach lumen by certain banding procedures or by gastric resection with a subsequent sleeve construction. The physical mechanism of action is the creation of flow resistance including a reduced reservoir function in the upper gut, making food ingestion uncomfortable or even painful. Both the small diameter of the gastrojejunostomy (the connection between the gastric pouch and the Roux limb) and the size of the gastric pouch are claimed to be determinants for food intake after RYGBP. A small caliber stoma would contribute with reduced passage of food and consequently a distension of the gastric pouch. Moreover, the small-sized gastric pouch is expected to contribute with a food intake restriction due to low reservoir capacity, and also due to low filling capacity, an increased wall tension in turn inducing signals of satiety or indigestion early during food intake. However, neither restriction at the gastrojejunostomy nor pouch size has been convincingly shown to be the point of action for reduced food intake and weight reduction following RYGBP [7–11]. It can be added that the surgical construction performed on the patients in the present study included a gastrojejunostomy with a diameter larger than 20 mm. This size of the stoma can hardly be expected to exert any prominent resistance to food passage [11].
The present investigation focused on the functional properties of the Roux limb. Despite that the RYGBP has been used for several decades, very little is known about the functional behavior of the Roux limb and to what extent this intestinal segment contributes to clinical outcome. Food ingestion will load and distend the Roux limb, and it can be hypothesized that the mechanosensitivity of this segment can contribute with sensations that make the subject terminate food intake. Hence, in the present study, balloon distension of the Roux limb was used because it represents a pure mechanical stimulation without simultaneous activation of mucosal chemosensitivity. Increased balloon volumes induced various unspecific sensations of discomfort (usually expressed as nausea) and pain. In general, these perceptions resembled those that previously have been reported to occur upon jejunal distensions in healthy volunteers [15, 16]. In a study by Accrino et al., the severity of the sensations had a dose (volume)–response relationship, i.e., lower balloon volumes were associated to non-painful or no sensations, whereas painful perceptions were obtained at larger distending volumes [15]. In the present study with Roux limb distension, it was not possible to establish a distinct difference between induction of non-pain and pain sensations, respectively. The reason to this is unclear and although a statistical type 2 error cannot be excluded, it may be that the mechanosensitivity of the Roux limb had adapted to the changed luminal conditions following surgical construction. Intestinal mechanosensitivity and related perceptions may also differ between obese persons and those with normal weight.
Opposite to what was expected, the perception thresholds (i.e., the lowest balloon volume giving rise to a perceived sensation) recorded in the present study correlated negatively to the preferred size of an ingested meal. Low perception thresholds (i.e., high mechanosensitivity of the Roux limb) were evident in subjects that ingested large meals (and vice versa). It may be speculated that food-induced distension, in addition to perceptions, also elicits an enhanced propulsive motility in the Roux limb that clears the lumen and makes it ready to receive more food. Future studies on Roux limb clearance are needed to further elucidate this possibility.
The present investigation also explored the biomechanical properties of the Roux limb in relation to preferred meal size 6 weeks and 1 year after RYGBP surgery. The major finding was that the size of a meal voluntarily chosen by the subject had a negative correlation to the intraluminal pressure that developed during balloon-induced distension of the Roux limb. In other words, subjects with high luminal pressure in response to balloon inflation preferred small meals. It is, therefore, reasonable to assume that the Roux limb exerts flow resistance that reduces the ingestive ability of the subject. The data suggest that individuals with “small-caliber” Roux limbs, thus with low mechanical compliance (i.e., a large net pressure increase following a given volume), have the most optimal effect with regard to reduction of food intake. To what extent this influenced BMI was not possible to conclude from the present study because of the small size of the investigated population. Although still hypothetical, a restrictive property due to the state of the Roux limb wall musculature is of great interest because it may be influenced by luminal nutrients like exposure to fat [15].
The present study has an explorative character and several study limitations need to be commented. For example, the study enrolled only ten subjects and the risk for statistical type 2 error has already been mentioned. Hence, confirmative studies in larger populations are needed also taking into account to what extent the biomechanical properties of the Roux limb are sustained over longer periods of time. Another limitation is that it is not for sure that the experimental food intake used in the study truly represents the ingestive behavior in the patient’s natural environment. A close look at the individual meal sizes in Fig. 2 shows that one subject actually increased his test meal after surgery. This turned out to be due to socio-cultural reasons. That particular subject had been fostered to eat what was served by others, but probably chose less at home when cooking and serving himself. Despite certain study limitations, the present results strongly indicate that the Roux limb is of great importance for determining food intake following RYGBP. Involved mechanisms of actions await to be elucidated in future studies. One field of considerable interest is the potential role of mechanically liberated gastrointestinal hormones like PYY and GLP-1 that in turn may influence, e.g., satiation. Unfortunately, such analyses could not be performed in the present study because blood samplings were not done in direct association to the Roux limb distensions.
In summary, the present study shows that the preferred meal size decreased radically in patients after RYGBP. Distension of the Roux limb by gradual balloon inflation was used to assess thresholds for perceptions as well as volume–pressure relationships. Roux limb distension elicited sensations of discomfort and even pain. Interestingly, subjects with a low perception threshold in the Roux limb (sensations were induced at low balloon volumes) preferred a large meal and vice versa. Furthermore, balloon-induced intra-Roux limb pressure correlated negatively to preferred meal size suggesting that the Roux limb exerts a flow resistance to luminal flow. Taken together, the results suggest that the Roux limb is an important determinant for the regulation of food intake after Roux-Y bypass bariatric surgery.
References
Sjostrom L, Lindroos AK, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351:2683–93.
Sjostrom L, Narbro K, Sjostrom CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357:741–52.
Olbers T, Bjorkman S, Lindroos A, et al. Body composition, dietary intake, and energy expenditure after laparoscopic Roux-en-Y gastric bypass and laparoscopic vertical banded gastroplasty: a randomized clinical trial. Ann Surg. 2006;244:715–22.
Brolin RL, Robertson LB, Kenler HA, et al. Weight loss and dietary intake after vertical banded gastroplasty and Roux-en-Y gastric bypass. Ann Surg. 1994;220:782–90.
le Roux CW, Welbourn R, Werling M, et al. Gut hormones as mediators of appetite and weight loss after Roux-en-Y gastric bypass. Ann Surg. 2007;246:780–5.
Ashrafian H, le Roux CW. Metabolic surgery and gut hormones—a review of bariatric entero-humoral modulation. Physiol Behav. 2009;97(5):620–31.
Nishie A, Brown B, Barloon T, et al. Comparison of size of proximal gastric pouch and short-term weight loss following routine upper gastrointestinal contrast study after laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2007;17:1183–8.
Roberts K, Duffy A, Kaufman J, et al. Size matters: gastric pouch size correlates with weight loss after laparoscopic Roux-en-Y gastric bypass. Surg Endosc. 2007;21:1397–402.
O'Connor EA, Carlin AM. Lack of correlation between variation in small-volume gastric pouch size and weight loss after laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2008;4:399–403.
Akkary E, Sidani S, Boonsiri J, et al. The paradox of the pouch: prompt emptying predicts improved weight loss after laparoscopic Roux-Y gastric bypass. Surg Endosc. 2009;23:790–4.
Cottam DR, Fisher B, Sridhar V, et al. The effect of stoma size on weight loss after laparoscopic gastric bypass surgery: results of a blinded randomized controlled trial. Obes Surg. 2009;19:13–7.
Lonroth H, Dalenback J, Haglind E, et al. Laparoscopic gastric bypass. Another option in bariatric surgery. Surg Endosc. 1996;10:636–8.
Olbers T, Lonroth H, Fagevik-Olsen M, et al. Laparoscopic gastric bypass: development of technique, respiratory function, and long-term outcome. Obes Surg. 2003;13:364–70.
Sarna SK. Cyclic motor activity; migrating motor complex: 1985. Gastroenterology. 1985;89:894–913.
Accarino AM, Azpiroz F, Malagelada JR. Selective dysfunction of mechanosensitive intestinal afferents in irritable bowel syndrome. Gastroenterology. 1995;108:636–43.
Hammer J, Fuhrer M. Intestinal chemo- and mechano-sensitivity: selective modification of small intestinal sensitivity by lipids. Aliment Pharmacol Ther. 2007;26:117–24.
Acknowledgments
This study has gained grant support from the Swedish Research Council (grant no K2010-55X-21432-01-2), the University of Gothenburg and the Sahlgrenska University Hospital (ALF), the Gothenburg Medical Association, and the Research Council of the Western Region of Sweden (VGR). The excellent support by our laboratory engineer Sören Lundberg is particularly acknowledged.
Conflicts of Interest
The authors declare that they have no conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
Per Björklund and Anna Laurenius contributed equally to this paper.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Björklund, P., Laurenius, A., Een, E. et al. Is the Roux Limb a Determinant for Meal Size After Gastric Bypass Surgery?. OBES SURG 20, 1408–1414 (2010). https://doi.org/10.1007/s11695-010-0192-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-010-0192-1