Abstract
Summary
The objective of this consensus statement is to inform the clinical practice communities, research centres and policymakers across Africa of the results of the recommendations for osteoporosis prevention, diagnosis and management. The developed guideline provides state-of-the-art information and presents the conclusions and recommendations of the consensus panel regarding these issues.
Purpose
To reach an African expert consensus on a treat-to-target strategy, based on current evidence for best practice, for the management of osteoporosis and prevention of fractures.
Method
A 3-round Delphi process was conducted with 17 osteoporosis experts from different African countries. All rounds were conducted online. In round 1, experts reviewed a list of 21 key clinical questions. In rounds 2 and 3, they rated the statements stratified under each domain for its fit (on a scale of 1–9). After each round, statements were retired, modified or added in view of the experts’ suggestions and the percent agreement was calculated. Statements receiving rates of 7–9 by more than 75% of experts’ votes were considered as achieving consensus.
Results
The developed guidelines adopted a fracture risk-centric approach. Results of round 1 revealed that of the 21 proposed domains, 10 were accepted whereas 11 were amended. In round 2, 32 statements were presented: 2 statements were retired for similarity, 9 statements reached consensus, whereas modifications were suggested for 21 statements. After the 3rd round of rating, the experts came to consensus on the 32 statements. Frequency of high-rate recommendation ranged from 83.33 to 100%. The response rate of the experts was 100%. An algorithm for the osteoporosis management osteoporosis was suggested.
Conclusion
This study is an important step in setting up a standardised osteoporosis service across the continent. Building a single model that can be applied in standard practice across Africa will enable the clinicians to face the key challenges of managing osteoporosis; furthermore, it highlights the unmet needs for the policymakers responsible for providing bone health care together with and positive outcomes of patients’ care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a public health epidemic that has negative impacts on health outcomes together with an enormous economic burden. The clinical relevance of osteoporosis lies in its associated fragility fractures, especially hip fractures, and usually it is a silent disease until such an event occurs [1]. Worldwide, osteoporosis causes more than 9 million fractures a year, meaning that there is a fragility fracture every 3 s [2]. In the Western World, it is estimated that about 1 in 3 women and 1 in 5 men above the age of 50 years old will sustain a fracture during their remaining lifetime [3]. After the age of 50 years, most sites of fracture can be considered characteristic locations of osteoporosis. Hip and vertebral fractures are the most common and serious osteoporotic fractures. Other fragility fractures, particularly in women, such as those of the humerus, forearm, ribs, pelvis and tibia (but not including ankle fractures), after the age of 50 years, have been reported to be associated with low bone mineral density (BMD) [4]. The direct annual cost of treating osteoporotic fractures of people on average is reported to be between 5000 and 6500 billion US Dollars in Canada, Europe and the USA alone, not considering indirect costs such as disability and loss of productivity [5]. Therefore, prevention of this disease can significantly reduce the morbidity, mortality and costs incurred by the health system.
Across Africa, the issue of bone health continues to be a major challenge. Osteoporosis has been overlooked as a health care priority in Africa, particularly in the sub-Saharan region [6]. This has been linked to several reasons. Firstly, health authorities have been overwhelmed by the burden of communicable diseases such as tuberculosis and human immunodeficiency virus (HIV) [7]. Secondly, tools to assess the BMD and consequently diagnose osteoporosis such as dual X-ray absorptiometry (DXA) are not widely available, hindering early diagnosis and treatment of the disease. Furthermore, concerns regarding inadequate calcium intake during adolescent years, low body mass index, prolonged duration of lactation amongst women during childbearing years, low levels of vitamin D and physical inactivity amongst Africans are all risk factors for osteoporosis [8].
On another front, the demographic changes taking place in Africa have fuelled both the diagnostic and therapeutic osteoporosis inertia in Africa. Census reports showed that both the total population size and life expectancy in Africa have increased significantly in the last two decades. An overview of demographic ageing in Africa published by the United Nations [9] found that Africa will have the fastest growth rate of older adults compared to any other region in the world. Between 2020 and 2050, the older African population is projected to triple from 74.4 million to 235.1 million and will outpace that of any other region of the world [10]. This has been supported by the new Census report on ageing trends in Africa [11] which revealed that between 2017 and 2050, 50% of the world’s population is expected to be in 9 countries (India, Nigeria, Democratic Republic of the Congo, Pakistan, Ethiopia, United Republic of Tanzania, United States of America (USA), Uganda and Indonesia), i.e. 5 of them are African nations.
African older adults play critical economic, family and community roles. Studies show that majority of the adults aged 60 to 64 years and around half of those aged 65 years and older in Africa remain in the labour force. Many older Africans, particularly women, contribute substantial amounts to providing unpaid home and care work [9]. Therefore, caring for this sector of the population become a priori. So far, there have not been any guidelines or treatment recommendations published for the management of osteoporosis in Africa. This guideline has been developed as an initiative by the African Society of Bone Health and Metabolic Diseases (ASBoM) with the intention of reducing the risk of osteoporosis-related fractures and thereby maintaining the quality of life for African people living with osteoporosis. It has been based on the outcomes of systematic reviews carried out in Africa on epidemiology of osteoporotic fractures as well as risk factors of osteoporosis in Africa. The objective is to provide a consensus, evidence-based information about the diagnosis, evaluation and treat-to-target management of osteoporosis in both men and postmenopausal women for the African health care professionals managing osteoporosis patients in general, regulatory bodies, health-related organizations and interested patients’ groups/laypersons. Although framed for Africa, it is hoped that these guidelines will be valuable for bone health specialists across the globe.
Methods
A qualitative synthesis of scientific evidence and consensus, based on clinical experience and existing scientific evidence, was used to formulate the study design and the following procedures. This work conforms to the preferred reporting items for systematic reviews and meta-analyses guidelines for reporting systematic reviews [12].
Study teams
Core team
Core team was composed of four experts in bone metabolism who were selected by the African Society of Bone Health and Metabolic Bone Diseases. Their task was to supervise, coordinate and assist with developing the scope of the project and initial Patient/Population, Intervention, Comparison, and Outcomes (PICO) questions. The core team prespecified outcomes as critical for each PICO question for the systematic literature review. The team also nominated the expert panel and drafting the manuscript.
Literature review team
Led by an experienced literature review consultant and based on specific research questions identified to focus on the treat-to-Target management of osteoporosis, the literature review was conducted with the assistance of an expert in methodology. The team completed the literature search (the PubMed/ MEDLINE, EMBASE and Cochrane databases), data abstraction and the quality of evidence rating [13]. Following the revision, each of the experts responsible for the literature review provided recommendations regarding each section based on evidence, when that was available or on their own experience. The level of evidence was determined for each section using the Oxford Centre for Evidence-based Medicine (CEBM) system (Table 1) [14].
Data sources and search strategies
The PICO questions (Table 2) were used to conduct the literature search in PubMed, Embase and Cochrane Library databases. Literature search strategies were carried out to locate randomised clinical trials evaluating the efficacy of osteoporosis quality improvement strategies published from 1990 to April 2021. The language was limited to English and French for pragmatic reasons. The search strategies were designed to be broad to have high sensitivity for identifying relevant literature. We used the following Medical Subject Headings (MeSH) terms: osteoporosis, postmenopausal osteoporosis, osteop?nia, T-score, bone resorption, fracture, osteoporosis treatment, osteoporosis management, calcium, vitamin D, alendronate, risedronate, etidronate, ibandronate, zoledronic acid, raloxifene, calcitonin, teriparatide, hormone replacement therapy, teriparatide, abaloparatide, romosozumab, denosumab, glucocorticoids, treatment induced osteoporosis, hip protectors, meta-analysis, systematic reviews, randomized controlled trials, bone density, FRAX, fracture liaison service, falls, Covid-19, treat to target. Keywords used were dependent on the PICO elements used in different combinations. Literature searches on 23rd April 2021 for PubMed and Cochrane Library databases, and on 28th April 2021 for Embase. Duplicate screening of literature search results was performed electronically. Additional relevant studies were retrieved by reviewing the reference lists of studies identified with the database search strategies that met the inclusion criteria.
Study selection
We selected relevant studies by applying inclusion and exclusion criteria to the literature retrieved with the search strategies.
Inclusion criteria
Articles included were systematic reviews, randomised controlled trials (RCTs), uncontrolled trials, observational studies including cohort, case–control and cross-sectional studies, or those where economic evaluation was made.
Exclusion criteria
Editorials, commentaries, conference abstracts and non-evidence-based narrative/personal reviews were excluded.
Expert panel
Given the fact that the developed guideline will be adopted across the continent of Africa, it was vital that the participating expert panel involved in developing the guideline would include experts from all the African continent regions (Central, North, West, East and South Africa). Expert panel members were appointed by the core team. The core leadership team nominated 17 participants. The criteria for their selection included existence of professional knowledge and experience (at least 8 years of experience) in the field of bone health, management of osteoporosis and active participation in scientific research on bone health disorders. The expert panel assisted with developing the scope of the project and refining the PICO questions. PICO questions were drafted into recommendation statements and were sent to the expert panel with the evidence report who voted on the recommendations.
Key questions used to develop the guideline
This guideline was based on a series of structured key questions that define the targeted population, fracture assessment, diagnostic tools, investigation, the comparison(s) utilised and the outcomes used to measure efficacy, effectiveness or risk. The evidence to answer the clinical questions was collected according to the following steps: formulation of clinical questions, structuring of questions, search for evidence, critical evaluation and selection of evidence, presentation of results and recommendations. These questions, shown in Table 2, formed the basis of the systematic literature search and consequently the clinical care standards.
Developing the standards of clinical care framework
Based on the answers to the structured key questions and the literature review, a structured template was developed to facilitate standardised identification of guideline components. For each guideline component, the format in which the recommendations/information was provided and extracted has been identified.
Delphi process
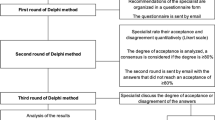
The Delphi technique is a structured method widely used to gather important information on a specific topic. It relies on the key assumption that forecasts from a group are generally more accurate than those from individuals. Therefore, the aim of the Delphi method is to construct consensus forecasts from a group of experts in a structured iterative manner. Its methodology is based on a series of questionnaires or ‘rounds’ addressed to experts. The key features of this method are the anonymity of participants and controlled feedback [15].
Delphi rounds
This was based on a three-stage on-line survey.
-
The first round: the participants were asked to consider the items identified by the systematic literature review, to suggest new items that might have been missed and to clarify items that might be unclear.
-
The second round was based on the results of the first round, and participants were asked to rate each item from 1 (not appropriate) to 9 (completely appropriate) and give their comments.
-
The third round, the participants reviewed the responses to each item obtained in the second round, after amendments wherever appropriate, and to rate the items after alterations (from 1 to 9)
Voting process
Live online-delivered voting was carried out in repeated rounds that were strictly time limited. All members of the task force were invited to participate and pre-informed of the time of opening and closure of each round of votes. Unique access links were sent out, and anonymous votes were gathered and processed. Comments on re-phrasing, potential ambiguity and unidentified overlaps were gathered regarding each statement at the same time in the voting process. Only the members of the task force had the right to vote on the statements.
Rating
Each statement is rated between 1 and 9 where 1 being ‘complete disagreement’ and 9 being ‘complete agreement’. Generally, 1–3, 4–6 and 7–9 represent disagreement, uncertainty and agreement, respectively. The ‘uncertainty’ vote represents ‘inconvenience about the accuracy of the recommendation’. There was no requirement to vote on all statements, and the members were encouraged to abstain if they felt that a statement fell outside their area of expertise. All statements were allowed for the entry of comments, which were reviewed by the scientific committee after each round of voting. The same scenario was adopted in each round of votes; the members were further urged to leave comments wherever they vote a disagreement. This enabled the panel to identify an instance of misinterpretation of statement and invalidate the vote on that statement.
Definition of consensus
Definition of consensus was established before data analyses. It was determined that consensus would be achieved if at least 75% of participants reached agreement (score 7–9) or disagreement (score 1–3) [15,16,17,18]. A statement was retired if it had a mean vote below 3 or a ‘low’ level of agreement. Statements whose rate come in the uncertainty score (4–6) were revised in view of the comments. The levels of agreement on each statement of recommendation were defined as ‘high’ if after the second round of votes, all votes on a statement fell into the agreement bracket (7–9) [18].
Data management and analysis
Survey data were combined as a total sample, included 17 individual responses, were analysed using SPSS Statistical Software (Statistical Package of Social Science, Armonk, New York), and results reported as means and standard deviation. Analysis by geography was not possible due to the anonymity of survey responses.
Ethical aspects
This study was performed in accordance with the Helsinki Declaration. Ethics approval was deemed unnecessary. Verbal informed consent was required from all the participants included in the study. All the participants were kept anonymous, in compliance with data protection regulations. The research questions, project oversight and resulting consensus-based practice guidelines were created by the core team and expert panel. The resulting guidelines do not reference or recommend any specific product; rather, they focus on how to assess and utilise the evidence to put a frame that is best suited for the patients’ management.
Results
Literature research and evidence selection
Evidence was obtained through literature searches and 3443 potentially relevant studies were initially identified. A total of 3339 studies were excluded for duplication (1266) or by screening of title and abstracts (2073). These are the studies which did not examine population or intervention of interest, did not match study design of interest or did not report outcome measures of interest. Therefore, relevant 104 studies were included for full article review. In total, 78 studies were excluded as citations did not provide evidence matching a PICO. Therefore, 26 studies were included in this work (Fig. 1).
Expert panel characteristics
The Delphi form was sent to the expert panel (n = 17), who participated in the three rounds. Respondents were drawn from several countries covering the different geographical regions of Africa: Egypt: 8 (47%), Morocco: 1 (5.8%), South Africa: 3 (17.64%) and 1 (5.8%), from each of: Cameron, Nigeria, Ghana, Tunisia and Sudan. The participants were rheumatologists who are specialised in the management of osteoporosis with mean experience of 20.3 ± 11.24 years.
Delphi round 1
The key clinical question comprised of 22 questions. In this round, the participants were asked to rate the overall principles considered in the decision-making for treat-to-target management of patients living with osteoporosis. The response rate for round 1 was 100% (17/17). The 17 experts accepted 10 of the proposed domains, suggested amendments for the remaining 12. Of the suggested changes, comments were raised regarding the domain ‘who are targeted in this guideline’, particularly regarding definite discrimination of both male and female osteoporosis; hence, it was considered when formulating the statements. There was a diversity of comments whether to merge the statements on treatment duration and the drug holiday, but it was decided to keep them separate. Other comments suggested the stratification of osteoporosis management into pharmacological and non-pharmacological with recommendation to clarify the concomitant use of therapeutic agents and adjunctive therapy; hence, a new subheading was added. Some of the modifications consisted of minor wording changes. Table 3 shows a list of the major as well as minor osteoporosis risk factors.
Delphi round 2
Based on input from round 1, the 17 experts were presented with 32 statements stratified under 22 domains. The response rate for round 2 was 100% (17/17). Of the statements presented, two statements were retired for similarity with another statement, 9 statements reached consensus (i.e. ≥ 75% of respondents strongly agreed or agreed) and were retained, whereas modifications were suggested for 21 statements. Comments (excluding minor editing suggestions) were more frequent for 4 domains: osteoporosis fracture risk, non-pharmacologic measures for bone health, male osteoporosis and steroid-associated osteoporosis. The statements were revised and amended. In addition, one statement was suggested to be added to the daily supplementation of calcium and vitamin D therapy domain and another one was added to the non-pharmacologic measures of bone health domain.
Delphi round 3
Based on input from round 2, the 17 experts were presented with 32 statements stratified under 22 domains. The response rate for round 3 was 100% (17/17). The experts came to consensus on the 32 statement to retain in the treat-to-target management guideline. The core team reviewed and made minor revisions to one of the retained statements that reached consensus. Consensus was reached (i.e. ≥ 75% of respondents strongly agreed or agreed) on all the clinical standards. Frequency of high-rate recommendation (rank 7–9) ranged from 83.33 to 100%. The experts were comfortable with the final list of the statements and with the Delphi process overall. Table 4 shows the level of evidence and grade of recommendation assigned to each statement, in accordance with the Oxford Centre for Evidence-Based Medicine (CEBM) criteria as well as mean ± standard deviation and level of agreement [14]. Agreement was unanimous (> 80% agreement) for the wording of the statements.
Recommendations for management of osteoporosis
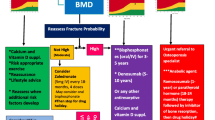
At the end of round 3, a total of twenty-two domains were obtained and a consensus was reached on all the statements developed. As health care professionals need information that is clear and readily accessible as well as applicable in standard clinical practice, it was important to articulate the developed osteoporosis guideline for the day-to-day practice. This is summarised in Fig. 2 which shows an algorithm for the treat-to-target management of postmenopausal osteoporosis.
An algorithm summarising the fracture-centric approach and the group’s consensus recommendations for the management of osteoporosis patients stratified according to their fracture risk. Case finding and management approach were set up according to the fracture risk category. The determination of fracture risk was carried out based on fracture risk score calculation (e.g. FRAX) and the measurement of lumbar spine and hip BMD
Discussion
The prevalence of osteoporosis is increasing steadily in developing countries secondary to increased longevity, with osteoporosis and its consequent fractures are becoming a major public health issue [21]. Epidemiological studies showed that in sub-Saharan Africa, the prevalence of osteoporosis was 20reported to range from 18.2 to 65.8% across a heterogenous at-risk population. Similar figures were reported in North Africa. The prevalence of osteoporosis in Egypt was 21.9% in men and 28.4% in women; whilst 26% of men and 53.9% of women having osteopenia [22]. The prevalence of osteoporosis in Moroccan postmenopausal women ranged between 21 and 31% [23, 24], which is similar to Tunisia, where 25% of postmenopausal women have osteoporosis [25], whereas the rate was slightly higher (35.8%) amongst Algerian women [26]. These rates were in concordance with the outcomes of studies evaluating the major clinical consequences of osteoporosis, i.e. fractures. A recent study investigating the incidence of hip fractures amongst Black South Africans found an age-adjusted hip fracture rate of 69.2 per 100,000 per annum and 73.1 per 100,000 per annum for women and men, respectively [27]. This evidence challenges the long-held view that osteoporosis-related fractures are rare in Blacks [28, 29] and highlight the importance of addressing the issue of osteoporosis in Africa.
The developed guideline agrees with the published guidelines from individual African nations for the management of osteoporosis including Egypt [30] and South Africa [31] as well as the international guidelines [32,33,34]. The guideline recommends very early intervention with osteoanabolic agents, for patients who are at very high risk of fracture. This agrees with the most recently published treatment recommendations, which endorsed the sequential as well as switch approaches of therapy [35, 36]. It also advocated a preventive approach for osteopenia patients at moderate to high risk of fractures, which agree with the recent available evidence [20]. The statements on osteoporosis management for patients with COVID-19 agree with those recently published by the National Osteoporosis Foundation [37]. This highlights the importance of having updated recommendations for osteoporosis management based on up-to-date evidence for best clinical practice. This guideline not only provides solutions for early identification of the cases, which will consequently help to will reduce fracture rates, but also enables health care professionals with special interest in bone health to face the key challenges of managing osteoporosis in Africa. The guidelines will assist the policymakers responsible for providing care for populations in relation to bone health to formulate appropriate policies.
Either a BMD-centric or a fracture risk-centric approach could be adopted to identify patients for whom pharmacological intervention should be considered. This guideline adopted the fracture risk-centric approach, though the BMD measurement was integrated, mainly for those with moderate fracture risk. This was based on the finding that DXA studies are seldomly used in Africa to assess for osteoporosis risk. This has been attributed in several cases to the lack of DXA machines. In other cases, it was linked to its prohibitive cost, even where the DXA machines are available [38]. Furthermore, the limitations of BMD for risk assessment have been one of the motives for the development of fracture risk prediction algorithms that integrate clinical risk factors for fracture. There are several fracture risk assessment tools available. Of these, the FRAX tool. (https://www.sheffield.ac.uk/FRAX/tool.aspx) has been the most extensively used. FRAX calculates the 10-year probability of a major fracture (clinical spine, humerus or wrist fracture) and 10-year probability of a hip fracture. A unique feature of FRAX is that it is based on a countries’ epidemiological data and considers competing mortality in the fracture risk estimation procedure [19].
Unfortunately, in Africa, there is a huge treatment gap between those at risk of fracture and those receiving treatment for the prevention of fragility fractures. Both the economic and societal burden of osteoporotic fragility fractures is enormous and is expected to rise owing to an increasing skew towards an older population [9, 10]. However, over the last two decades, there has been a significant shift towards the better ability to predict those at risk, using fracture prediction tools and an increasing understanding of scanning modalities, such as DXA or qualitative ultrasound scans [38]. This will allow appropriate earlier identification of patients with osteopenia or osteoporosis, who are at high or very high risk of fracturing, to benefit from osteoporosis therapy. Furthermore, a variety of generic therapeutic options are now available, at economically feasible prices. The developed guidelines endorse this armamentarium and provide a solid background to making appropriate treatment decisions, which is a step forward towards closing this gap in Africa.
The paradigm of treat-to-target aims at enhanced and individualised care of osteoporotic patients. Such strategy enables the treating clinicians to select the most appropriate initial osteoporosis therapy and guides subsequent decisions to continue, change or stop treatment [19, 33, 39]. Though some publications revealed that FRAX can be used to predict new posttreatment fracture probability and assess the reduction in the fracture risk in women currently on osteoporosis therapy [40, 41], the predominant trend is that FRAX cannot be used to monitor response to therapy. On the other hand, repeat DXA informs on the long-term treatment effect on BMD. The new concept of very high fracture risk and the development of new intervention thresholds [30, 42] provide a new manifesto based on which this guideline has been developed. The very high fracture risk and the consequent further utility loss immediately after a subsequent fracture (imminent risk) suggest that preventive treatment given as soon as possible after fracture would avoid a higher number of new fractures and reduce the attendant morbidity, compared with the treatment given later [30, 43].
Monitoring of patients on osteoporosis therapy should include regular communication with a health care professional to make sure that (1) the osteoporosis therapy is taken correctly and regularly as well as to ensure that treatment has been initiated within 16 weeks of non-traumatic fracture; (2) calcium and vitamin D supplement therapy are taken regularly and in appropriate dose (check adherence at 3 months and at 12 months); (3) address any concerns or adverse effects the patient might have; and (4) there are no comorbidities or other medications that might impact the expected treatment outcome. Whilst BMD is considered a surrogate marker for bone strength and fracture risk, stability or a significant increase in BMD is considered an acceptable treatment outcome and is associated with a reduction in fracture risk [44]. The time interval when treatment effect can be detected may vary depending on treatment modality, risk factors and current medications. A DXA scan should only be repeated if the results will impact the clinical management, or if changes in BMD are expected to exceed the least significant change (LSC) for the DXA equipment used. The annual rates of loss during these intervals are approximately 1.8–2.3% in the spine and 1.0–1.4% in the hip. This is well below the least significant change (LSC), averaging 2–3% for most DXA machines at the total hip. Therefore, repeat DXA scan should be considered after 2–3 years of the former scan, which has been recommended in this guideline. The target of bone mineral density (BMD) (in the range of − 1.5 to − 2) as suggested in this guideline agrees with those reported in other studies [19, 30, 39].
This guideline includes health care professionals from the entire African continent, ensuring that all the regions have been covered and represented; therefore, it is expected to be implemented across the whole of Africa. The aim is to streamline the osteoporosis service provided to the patients across the continent and ensure that osteoporosis therapy is determined or escalated according to the patient’s risk factors and fracture risk within an approved framework. The Delphi technique has proven to be a reliable measurement instrument in developing new concepts and setting the direction of future-orientated research [16]. In Delphi methodology, consensus usually arises when agreement or disagreement ranges from 50 to 80% [17]. In our work, the agreement ranged between 83.3 and 100%, indicating a strong trend amongst the African health care professionals to have a treat-to-target approach for osteoporosis management. These findings agree with the results of the Spanish consensus on osteoporosis management [45] as well as the Egyptian guidelines for osteoporosis management [31], which revealed similar scores on the treat to target policy.
Limitations of the guideline
This guideline reflects the best data available at the time the report was prepared. Caution should be exercised in interpreting the data; the results of future studies may require alteration of the conclusions or recommendations in this report. It may be necessary or even desirable to depart from the guidelines in the interests of specific patients and special circumstances. Just as adherence to guidelines may not constitute defence against a claim of negligence, so deviation from them should not necessarily be deemed negligent.
Plans for guideline revision
This field of osteoporosis therapeutics is in a rapid phase of development, and revision of the scope and content of the guideline will therefore occur on regular basis. Where necessary, the guideline will be updated.
In conclusion, with changing demography, the cost of treating osteoporosis is expected to increase considerably in Africa by the year 2030. Understanding of the impact of clinical risk factors can influence prevention and treatment of osteoporotic fractures. Therefore, it is vital to screen the patients and stratify them according to their identified fracture risk. This was a wide and representative panel of experts who established consensus regarding the management of postmenopausal osteoporosis in Africa. It also expanded to give guidance for the management of osteoporosis in men and the potential role of fracture liaison service in standard practice. The algorithm developed in this study facilitates the incorporation of several recent developments into the standard patient management protocols.
References
International Osteoporosis Foundation (2018): what is osteoporosis? 2018. https://www.iofbonehealth.org/what-is-osteoporosis Accessed 31 July 2021
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726–1733
Kanis J, Johnell O, Oden A, Sernbo I, Redlund-Johnell I, Dawson A, De Laet C, Jonsson B (2000) Long-term risk of osteoporotic fracture in Malmö. Osteoporos Int 11:669–674
Kanis JA, Oden A, Johnell O, Jonsson B, de Laet C, Dawson A (2001) The burden of osteoporotic fractures: a method for setting intervention thresholds. Osteoporos Int 12:417–427
Rashki Kemmak A, Rezapour A, Jahangiri R, Nikjoo S, Farabi H, Soleimanpour S (2020) Economic burden of osteoporosis in the world: a systematic review. Med J Islam Repub Iran 34:154
Handa R, Kalla AA, Maalouf G (2008) Osteoporosis in developing countries. Best Pract Res Clin Rheumatol 22:693–708
Paruk F, Tsabasvi M, Kalla AA (2021) Osteoporosis in Africa—where are we now. Clin Rheumatol 40(9):3419–3428
Billek-Sawhney B (2019) Osteoporosis risk – think twice about bone density in Ethiopians African Americans. Int Phys Med Rehab J 4(3):91–94
Yumiko Kamiya, DESA, United Nations: department of economic and social affairs. Population Division United Nations Regional Workshop, Lilongwe, July 2016. https://www.un.org/development/desa/pd/sites/www.un.org.development.desa.pd/files/unpd_ws201607_demographic_trends_in_africa_yk.pdf
Census Bureau Releases New Report on Aging in Africa, SEPTEMBER 02, 2020. RELEASE NUMBER CB20-TPS.53. https://www.census.gov/newsroom/press-releases/2020/aging-in-africa.html. Accessed 11 Aug 2021
National Institute of Aging. New census report on aging trends in Africa. https://www.nia.nih.gov/news/new-census-report-aging-trends-africa. Accessed 2 Aug 2021
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med 151:W65-94
Leclercq E, Leeflang MM, van Dalen EC, Kremer LC (2013) Validation of search filters for identifying pediatric studies. J Pediatr 162:629–634
OCEBM Levels of Evidence Working Group (2011) The Oxford levels of evidence 2. Oxford Centre for Evidence-Based Medicine, Oxford
Von der Gracht H (2012) Consensus measurement in Delphi studies: review and implications for future quality assurance. Technol Forecast Soc 79(8):1525–1536
Rowe G, Wright G (1999) The Delphi technique as a forecasting tool: issues and analysis. Int J Forecast 15:353–375
Rayens MK, Hahn EJ (2000) Building consensus using the policy Delphi method. Policy Polit Nurs Pract 1(4):308–315
Diamond IR, Grant RC, Feldman BM, Pencharz PB, Ling SC, Moore AM, Wales PW (2014) Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol 67(4):401–409
Kanis JA, Johansson H, Oden A, McCloskey EV (2011) Guidance for the adjustment of FRAX according to the dose of glucocorticoids. Osteoporos Int 22:809–816
Reid IR, Horne AM, Mihov B, Stewart A, Garratt E, Wong S, Wiessing KR, Bolland MJ, Bastin S, Gamble GD (2018) Fracture prevention with zoledronate in older women with osteopenia. N Engl J Med 379(25):2407–2416
Kinsella K, Wan H. An aging world: 2008. U.S. Census Bureau. International Population Reports. 2009; 9(1): 9
Gheita T, Hammam N (2018) Epidemiology and awareness of osteoporosis: a viewpoint from the Middle East and North Africa. Int J Clin Rheumatol 13(3):134–147
Ouzzif Z, Oumghar K, Sbai K et al (2012) Relation of plasma total homocysteine, folate and vitamin B12 levels to bone mineral density in Moroccan healthy postmenopausal women. Rheumatol Int 32(1):123–8
El Maghraoui A, Sadni S, El Maataoui A, Majjad A, Rezqi A, Ouzzif Z, Mounach A (2015) Influence of obesity on vertebral fracture prevalence and vitamin D status in postmenopausal women. Nutr Metab (Lond) 14(12):44
Ben Aissa R, Laatar A, Kerkeni S et al (2006) Prévalence de Et, l’ostéoporose chez les femmes ménopausées des gouvernorats de l’Ariana 119, de la Manouba-Tunis. Tun. Méd. 84(Suppl 10)
Haouichat C, Hammoumraoui N, Lehtihet S et al (2014) SAT0461 Prevalence of postmenopausal osteoporosis in Algerian women. Ann Rheum Dis 73:760
Paruk F, Matthews G, Cassim B (2017) Osteoporotic hip fractures in Black South Africans: a regional study. Arch Osteoporos 12(1):107
Cauley JA, Wu L, Wampler NS et al (2007) Clinical risk factors for fractures in multi-ethnic women. the women’s health initiative. J Bone Miner Res 22:1816–1826
Peled R, Dahan D, Endevelt R et al (2007) Osteoporosis among Ethiopian immigrant women: a risk analysis. Arch Osteoporos 2:45–52
El Miedany Y, Abu-Zaid MH, El Gaafary M et al (2021) Egyptian consensus on treat-to-target approach for osteoporosis: a clinical practice guideline from the Egyptian Academy of bone health and metabolic bone diseases. Egypt Rheumatol Rehabil 48:5. https://doi.org/10.1186/s43166-020-00056-9
Amod A, Ascott-Evans B, Brown S, Cassim B, Davey M, de Lange W, de Villiers T et al (2017) South African clinical guideline for the diagnosis and management of osteoporosis: JEMDSA 2017; 22(1) (Supplement 1)
Camacho PM, Petak SM, Binkley N, Diab DL, Eldeiry LS, Farooki A, Harris ST, Hurley DL, Kelly J, Lewiecki EM, Pessah-Pollack R, McClung M, Wimalawansa SJ, Watts NB (2020) American Association of Clinical Endocrinologists/American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis-2020 update. Endocr Pract 26(Suppl 1):1–46
Kanis J, Cooper C, Rizzoli R et al (2019) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 30:3–44
Meeta M, Harinarayan CV, Marwah R, Sahay R, Kalra S, Babhulkar S (2020) Clinical practice guidelines on postmenopausal osteoporosis: *an executive summary and recommendations - update 2019–2020. J Midlife Health 11(2):96–112
Eastell R, Rosen CJ, Black DM, Cheung AM, Murad MH, Shoback D (2019) Pharmacological management of osteoporosis in postmenopausal women: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 104(5):1595–1622
UK consensus guideline on the management of patients at low, high, and very high risk of osteoporotic fracture. Cyrus Cooper, Kassim Javaid, Mary Elliott, David Stephens, Nuttan Tanna. www.Guidelines.co.uk 2020 [https://www.guidelines.co.uk/musculoskeletal-and-joints-/osteoporotic-fracture-guideline/455546.article ] accessed on 15th July 2021
National Osteoporosis Foundation. Joint guidance on COVID-19 vaccination and osteoporosis management from the American Society for Bone and Mineral Research (ASBMR), American Association of Clinical Endocrinology (AACE), Endocrine Society, European Calcified Tissue Society (ECTS), the International Osteoporosis Foundation (IOF), and the National Osteoporosis Foundation (NOF). Published online March 9, 2021. Accessed July 15, 2021. https://www.nof.org/news/statement-joint-guidance-on-covid-19-vaccination-and-osteoporosis-management-from-the-asbmr-aace-endocrine-society-ects-iof-and-nof/
Atiase Y, Quarde A (2020) A call to action for osteoporosis research in sub-Saharan Africa. Ghana Med J 54(1):58–67
Lewiecki EM (2017) Osteoporosis: Treat-to-Target. Curr Osteoporos Rep 15(2):103–109
Leslie WD, Lix LM, Johansson H, Oden A, McCloskey E, Kanis JA (2012) Does osteoporosis therapy invalidate FRAX for fracture prediction? J Bone Miner Res 27:1243–1251
El Miedany YE, Gaafary ME, Yassaki AE, Youssef S, Nasr A, Ahmed I (2014) Monitoring osteoporosis therapy: can FRAX help assessing success or failure in achieving treatment goals? World J Rheumatol 4(2):14–21
Kanis JA, Harvey NC, McCloskey E et al (2020) Algorithm for the management of patients at low, high and very high risk of osteoporotic fractures. Osteoporos Int 31:1–12
Lewiecki EM (2010) Bone density testing to monitor osteoporosis therapy in clinical practice. Am Fam Physician 82(7):749–754
Lewiecki EM, Watts NB (2008) Assessing response to osteoporosis therapy. Osteoporos Int 19(10):1363–1368
Nogués X, Nolla JM, Casado E, Jódar E, Muñoz-Torres M, Quesada-Gómez JM, Canals L, Balcells M, Lizán L (2018) Spanish consensus on treat to target for osteoporosis. Osteoporos Int 29(2):489–499
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
El Miedany, Y., Paruk, F., Kalla, A. et al. Consensus evidence-based clinical practice guidelines for the diagnosis and treat-to-target management of osteoporosis in Africa: an initiative by the African Society of Bone Health and Metabolic Bone Diseases. Arch Osteoporos 16, 176 (2021). https://doi.org/10.1007/s11657-021-01035-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-021-01035-z