Abstract
Objective
To investigate the efficiency, safety, and possible mechanisms of Qingre Buyi Decoction (清热补益煎剂, QBD) in the treatment of acute radiation proctitis (ARP).
Methods
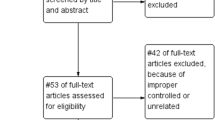
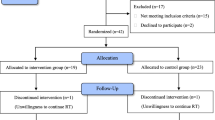
This study was a single center, prospective, single blind, randomized, and placebo-controlled clinical trial. A total of 60 patients with ARP was equally and randomly distributed into the control group (conventional treatment) and the combination group (conventional treatment plus QBD). The changes of main Chinese medicine clinical symptoms and signs, including stomachache, diarrhea, mucous or bloody stool before and after treatment, and their adverse reactions were observed after the two-week treatment. Also, D-lactate and diamine oxidase (DAO) levels, hepatic and renal function were measured. Cure rates, effective rates, and recurrence rates were compared between the two groups.
Results
The blood levels of both DAO and D-lactate were significantly decreased in the combination group as compared with those in the control group (P<0.05 or P<0.01). All main clinical symptoms and signs were alleviated more significantly in the combination group (P<0.01). The main symptom scores also were significantly decreased after treatment in the control group (P<0.01), except those for mucous or bloody stool (P>0.05). Compared to the control group, the improvements of stomachache, diarrhea, defecation dysfunction, and stool blood in the combination group were significantly better (P<0.05 or P<0.01). For the combination group, the curative rate, effective rate, and recurrence rate was 76.67%, 16.67%, and 6.67%, respectively. On the other hand, for the control group, the rate was 53.33%, 16.67%, and 30.00%, respectively. The total curative effect was significantly better in the combination group than in the control group (P<0.05). However, the recurrence rate was similar between the two groups (P>0.05). The hepatic and renal function remained normal in both groups (P>0.05). In addition, no severe adverse event was found in both groups.
Conclusions
Addition of QBD to the conventional treatment can effectively alleviate the damage of intestinal mucosal barrier function and improve all main clinical symptoms and signs of the ARP. The combination of conventional treatment with Chinese herbal medicine QBD is effective and safe for ARP.
Similar content being viewed by others
References
Korkut C, Asoglu O, Aksoy M, Kapran Y, Bilge H, Kiremit-Korkut N, et al. Histopathological comparison of topical therapy modalities for acute radiation proctitis in an experimental rat model. World J Gastroenterol 2006;12:4879–4883.
Vernia P, Fracasso PL, Casale V, Villotti G, Marcheggiano A, Stigliano V, et al. Topical butyrate for acute radiation proctitis: randomised, crossover trial. Lancet 2000;356:1232–1235.
Zhang ZZ, Wang Y, Wang L, Liu JH. Professor LIU Jianhua’s experiences on diagnosis and treatment of radiation enterocolitis. Chin Archives Tradit Chin Med (Chin) 2008;26:1503–1504.
Ministry of Health of the PRC. Diagnostic criteria for radiation proctitis. The occupational health standards of the People’s Republic of China. GBZ111-2002, Beijing: Law Press; 2004:1–3
Lu WZ. Treatment of radiation enteritis by Changyun mixture: a clinical observation of 42 cases. New J Tradit Chin Med (Chin) 2007;39(2):20–21.
Li JY, Lu Y, Hu S, Sun D, Yao YM. Preventive effect of glutamine on intestinal barrier dysfunction induced by severe trauma. World J Gastroenterol 2002;8:168–171.
Yu Y, Sheng ZY, Chai JK, Li JY, Yang XD, Yuan SA, et al. Changes in plasma D-lactate and intestinal IgA levels in severe burn patients. J Trauma Surg (Chin) 2003;5:122–124.
State Administration of Traditional Chinese Medicine of the People’s Repubtc of China. Criteria of diagnosis and therapeutic effect of disease and syndromes in traditional Chinese medicine. Nanjing: Nanjing University Press;1994:9–10.
Jahraus CD, Bettenhausen D, Malik U, Sellitti M, St Clair WH. Prevention of acute radiation-induced proctosigmoiditis by balsalazide: a randomized, double-blind, placebo controlled trial in prostate cancer patients. Int J Radiat Oncol Biol Phys 2005;63:1483–1487.
Sanguineti G, Franzone P, Marcenaro M, Foppiano F, Vitale V. Sucralfate versus mesalazine versus hydrocortisone in the prevention of acute radiation proctitis during conformal radiotherapy for prostate carcinoma. A randomized study. Strahlenther Onkol 2003;179:464–470.
Hovdenak N, Sørbye H, Dahl O. Sucralfate does not ameliorate acute radiation proctitis: randomised study and meta-analysis. Clin Oncol (R Coll Radiol) 2005;17:485–491.
Kneebone A, Mameghan H, Bolin T, Berry M, Turner S, Kearsley J, et al. The effect of oral sucralfate on the acute proctitis associated with prostate radiotherapy: a doubleblind, randomized trial. Int J Radiat Oncol Biol Phys 2001;51:628–635.
Tian YP, Wang QC. Clinical observation on Shenling Baizhu San combined with Western medicine in the treatment of rectal injury induced by radiotherapy. Chin J Integr Tradit West Med (Chin) 2008;28:159–160.
Li JY, Sun D, Lu Y, Jin H, Hu S, Sheng ZY. Effect of intestinal ischemia-reperfusion on gut barrier, absorption, penetration and transmissin. World J Gastroenterol (Chin) 2004;12:464–466.
Kamiya S, Nagino M, Kanazawa H, Komatsu S, Mayumi T, Takagi K, et al. The value of bile replacement during external biliary drainage: an analysis of intestinal permeability, integrity, and microflora. Ann Surg 2004;239:510–517.
Ruan P, Gong ZJ, Zhang QR. Changes of plasma D(−)-lactate, diamine oxidase and endotoxin in patients with liver cirrhosis. Hepatobiliary Pancreat Dis Int 2004;3:58–61.
Assadian A, Assadian O, Senekowitsch C, Rotter R, Bahrami S, Fürst W, et al. Plasma D-lactate as a potential early marker for colon ischemia after open aortic reconstruction. Eur J Vasc Endovasc Surg 2006;31:470–474.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by Key Medical Program of the “10th Five-Year Plan” of PLA Nanjing Military Area Command (No. 02MA009)
Rights and permissions
About this article
Cite this article
Wang, L., Zhang, Zz., Tu, Xh. et al. Safety and efficacy of Qingre Buyi Decoction (清热补益煎剂) in the treatment of acute radiation proctitis: A prospective, randomized and controlled trial. Chin. J. Integr. Med. 15, 272–278 (2009). https://doi.org/10.1007/s11655-009-0272-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11655-009-0272-z